Zonulin and DAO Markers: Advanced Interpretation for Intestinal Barrier Labs
Biomarker analysis reveals permeability issues and informs targeted treatment plans.
Zonulin and DAO Markers: Advanced Barrier Lab Interpretation
Intestinal barrier assessment using biomarkers such as zonulin and diamine oxidase (DAO) has become a cornerstone in evaluating gut health, offering clinicians powerful tools for diagnosing and monitoring conditions related to intestinal permeability. This article provides a comprehensive overview of the latest science, clinical relevance, diagnostic interpretation, and practical implications of these advanced intestinal barrier markers.
Table of Contents
- Introduction: The Gut Barrier Function
- Biology of Zonulin and DAO
- Mechanisms of Intestinal Barrier Dysfunction
- Zonulin and DAO as Barrier Biomarkers
- Clinical Indications for Testing
- Laboratory Methods and Interpretation
- Evidence and Disease Association
- Impact of Interventions
- Clinical Application and Limitations
- Frequently Asked Questions (FAQs)
Introduction: The Gut Barrier Function
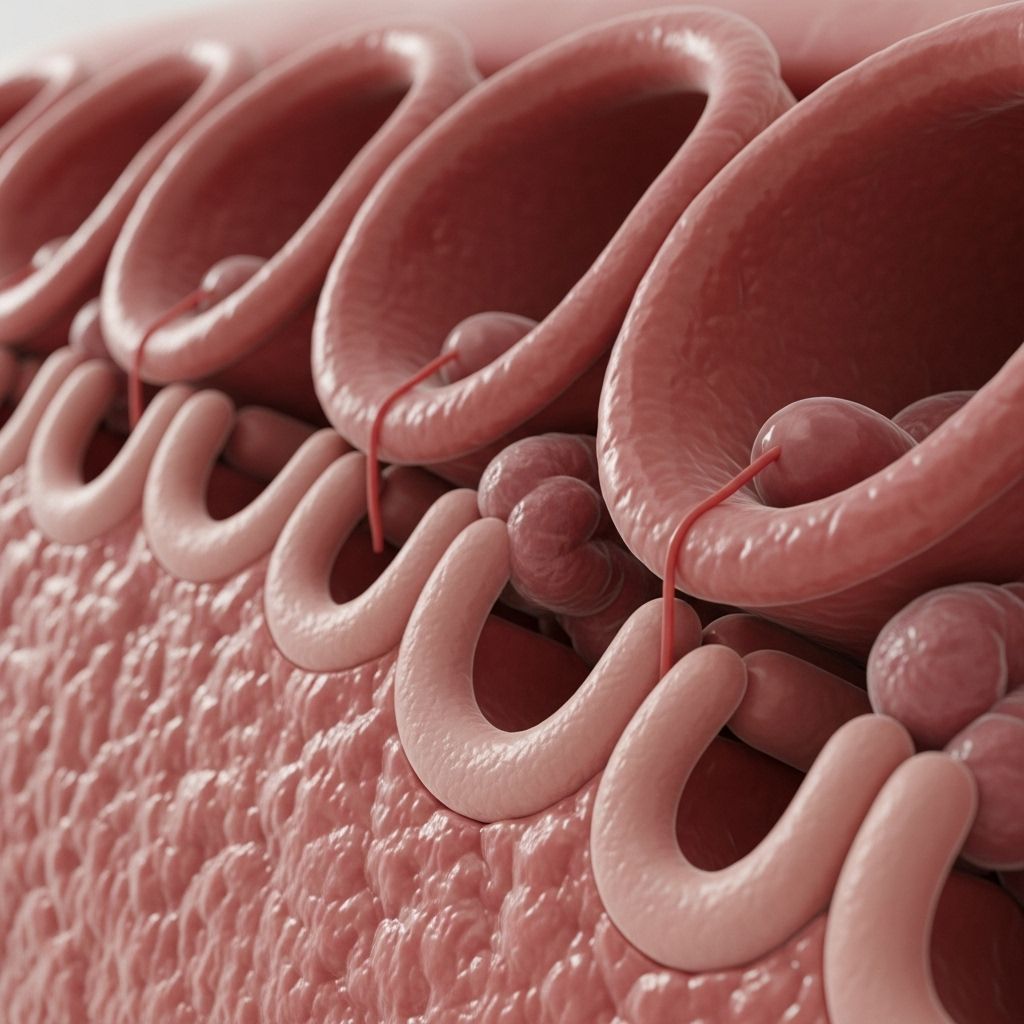
The intestinal barrier is a complex structure designed to balance nutrient absorption and immune defense. Comprised primarily of a single layer of epithelial cells joined by tight junctions, it prevents the translocation of harmful substances from the gut lumen into the circulation. When the integrity of this barrier is compromised—a phenomenon commonly referred to as ‘leaky gut’ or increased intestinal permeability—numerous health consequences can ensue, including inflammation, autoimmunity, food intolerance, and systemic symptoms.
Biology of Zonulin and DAO
Zonulin: The Tight Junction Modulator
Zonulin is a regulatory protein that acts as a gatekeeper of intestinal tight junctions. Triggered by dietary components, microbes, and toxins, it transiently opens tight junctions, thereby increasing permeability. When released excessively, it can impair barrier integrity and promote passage of macromolecules and antigens into systemic circulation, fostering inflammation and immune activation.
Diamine Oxidase (DAO): The Histamine and Barrier Marker
DAO is an enzyme abundantly present in the intestinal mucosa, where it degrades histamine from ingested food. Its levels not only reflect histamine-degrading capacity but also serve as an indicator of enterocyte health, since DAO is synthesized and released by mature intestinal cells. Reduced DAO often signals injury or loss of these cells, commonly seen in inflammatory or degenerative gut diseases.
Mechanisms of Intestinal Barrier Dysfunction
The gut barrier can be disrupted by several intrinsic and extrinsic factors:
- Genetic predisposition affecting tight junction protein expression (including zonulin modulation).
- Chronic inflammation from infections, dysbiosis, or autoimmune disease.
- Dietary triggers such as gluten, high FODMAPs, alcohol, and food additives.
- Medication-induced injury (NSAIDs, antibiotics, chemotherapy).
- Oxidative and metabolic stress.
This disruption increases paracellular permeability, allowing the passage of harmful luminal contents, which can initiate or exacerbate disease processes.
Zonulin and DAO as Barrier Biomarkers
Zonulin
- Mechanistic marker: As the only known physiological modulator of tight junctions, zonulin’s serum or plasma concentration directly reflects gut permeability status.
- Diagnostic utility: Elevated levels typically indicate a compromised barrier (“leaky gut”) and are associated with various gastrointestinal and systemic disorders.
DAO
- Marker of enterocyte integrity: DAO activity reflects the functional mass of the intestinal epithelium. Decreased DAO may indicate mucosal injury, atrophy, or inflammation.
- Indicator of histamine intolerance: Low DAO leads to decreased degradation capacity for dietary histamine, which can cause symptoms such as headaches, skin rashes, and GI distress upon histamine-rich food ingestion.
Clinical Indications for Testing
Lab assessment of zonulin and DAO is recommended in the following scenarios:
- Suspected increased intestinal permeability (chronic GI symptoms, unexplained food reactions, autoimmune diseases).
- Diagnosis or management of histamine intolerance.
- Assessment in chronic inflammatory conditions (IBD, celiac disease, IBS, allergies).
- Monitoring response to therapies targeting gut integrity (diet, probiotics, anti-inflammatories).
- Research settings exploring microbiome, barrier dysfunction, and systemic disease links.
Laboratory Methods and Interpretation
Sample Types and Testing Approaches
- Zonulin: Most commonly measured by enzyme-linked immunosorbent assay (ELISA) in serum or plasma. Fecal zonulin is also utilized but less standardized.
- DAO: Measured as enzyme activity (U/mL) or concentration in plasma/serum using colorimetric or ELISA-based assays.
Interpretative Ranges
| Marker | Reference Range* | Indicative Interpretation |
|---|---|---|
| Zonulin (serum/plasma) | Typically < 61 ng/mL (varies per lab) | Elevated: Compromised tight junctions, increased permeability |
| DAO (serum/plasma) | Typically 10-30 U/mL | Low: Enterocyte loss/injury or histamine intolerance risk High: Possible compensatory increase in some conditions |
*Ranges are indicative and may vary based on the laboratory methodology and population.
Factors Influencing Results
- Acute intestinal injury or infection can temporarily alter marker levels.
- Certain medications and supplements may modulate zonulin or DAO.
- Test timing and fasting status may impact levels; standardized protocols are recommended.
Evidence and Disease Association
Elevated Zonulin and Pathology
- Autoimmune Diseases: High serum zonulin is observed in conditions such as celiac disease, type 1 diabetes, and Graves’ disease. In Graves’ disease, higher zonulin and D-lactate correlate with disease risk, while remission tends to normalize levels.
- Irritable Bowel Syndrome (IBS): Patients with diarrhea-predominant IBS often have increased zonulin and elevated small intestinal permeability, which improves with diet modification.
- Inflammatory Bowel Diseases: Crohn’s disease and ulcerative colitis are associated with barrier dysfunction and increased zonulin.
- Food Allergies and Sensitivities: Leaky barriers allow antigen passage, instigating immune reactions. Zonulin can be a predictor of clinical severity in these settings.
DAO Deficiency and Histamine Intolerance
- Histamine intolerance: Reduced plasma DAO contributes to the inability to degrade ingested histamine, leading to systemic symptoms.
- Mucosal disease: Inflammatory and atrophic conditions (celiac, IBD, gastroenteritis) decrease DAO via enterocyte damage.
- Secondary enzyme deficiencies: Chronic inflammation causing reduced DAO also often leads to other enzymatic deficits, exacerbating food intolerance syndromes.
Impact of Interventions
New research highlights the role of nutrition and targeted therapies on barrier health as measured by zonulin and DAO:
- Dietary Interventions: Low FODMAP diets improve permeability and reduce zonulin, notably in IBS patients. Gluten avoidance benefits celiac and non-celiac gluten sensitivity by lowering zonulin.
- Probiotic Supplementation: Several randomized controlled trials confirm that select probiotics reduce serum zonulin and improve barrier function, with greater efficacy in patients versus healthy controls. However, intervention duration and strain specificity affect outcomes.
- Anti-inflammatory and gut-repair agents: Nutrients such as omega-3 fatty acids and fiber, and lifestyle modifications, contribute to barrier restoration by modulating inflammation and the microbiome.
Clinical Application and Limitations
How to Integrate Marker Interpretation in Practice
- Use zonulin as a sensitive screen for compromised gut integrity in unexplained GI or systemic symptoms, or as a marker of disease activity in autoimmune and inflammatory syndromes.
- Evaluate DAO when patients present with signs of histamine intolerance or persistent GI symptoms despite dietary interventions.
- Track changes in marker levels to monitor response to dietary, microbiome-targeted, or anti-inflammatory therapies.
Limitations and Considerations
- Assay variability: Different laboratories use varying methods, which can result in discrepancies in reference ranges and outcomes.
- Non-specific elevations: Zonulin sometimes rises in acute conditions or transiently without chronic barrier dysfunction.
- DAO influences: DAO levels can be reduced by medications, micronutrient deficiencies (zinc, copper, vitamin B6), or unrelated mucosal injury.
- Markers are best interpreted as part of a comprehensive clinical assessment, considering patient history, symptoms, and other laboratory findings.
Frequently Asked Questions (FAQs)
What does an elevated zonulin level mean?
Elevated zonulin indicates increased intestinal permeability, signifying compromised tight junctions in the gut epithelium and suggesting susceptibility to systemic immune activation or inflammation.
Can DAO deficiency be reversed?
In many cases, restoring gut mucosal integrity via dietary changes, inflammation management, and microbiome support can improve DAO production, though some chronic diseases may cause persistent reduction.
Is there a gold standard for leaky gut testing?
No single test is definitively diagnostic; measuring zonulin, DAO, and other permeability markers together, interpreted within clinical context, gives the most meaningful assessment.
Are these tests useful for non-GI symptoms?
Yes, since gut permeability dysfunction can contribute to systemic disorders, including neurological, dermatological, and metabolic diseases, barrier markers like zonulin and DAO have value beyond traditional GI conditions.
How often should these markers be re-tested?
Frequency depends on clinical scenario—generally at baseline to guide treatment and after 3 to 6 months to evaluate therapeutic impact or symptom changes.
References
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.796212/pdf
- https://www.imd-berlin.de/en/special-areas-of-competence/food-intolerances/leaky-gut/intestinal-permeability
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1143548/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11357486/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7582069/
- https://precisionpointdiagnostics.com/test/advanced-barrier-assessment-plasma/
- https://www.rupahealth.com/lab-tests/precision-point-advanced-intestinal-barrier-assessment
Read full bio of Sneha Tete












