Yeast Infection vs. UTI: Key Differences, Symptoms, Causes & Treatment
Clear insights into women's reproductive discomfort and tailored care approaches.
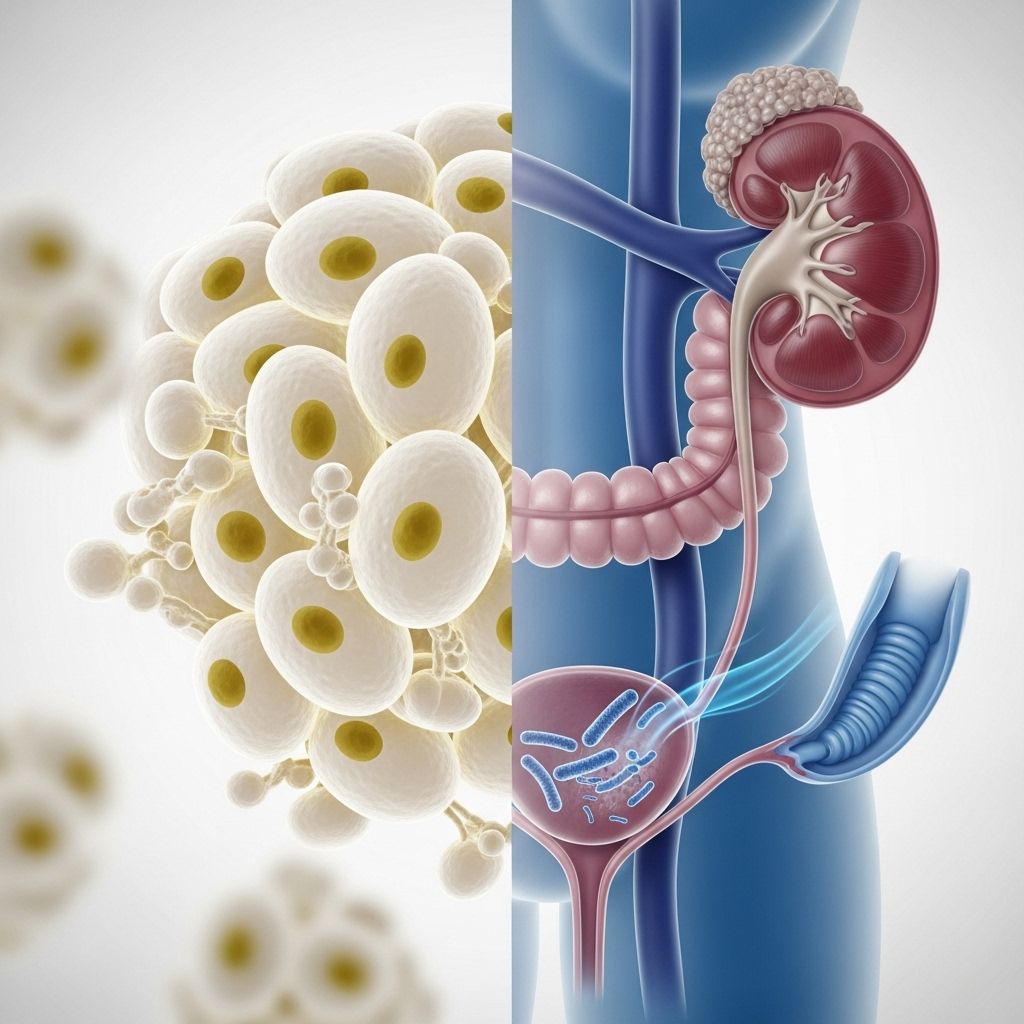
Yeast Infection vs. Urinary Tract Infection (UTI): What’s the Difference?
Yeast infections and urinary tract infections (UTIs) are two of the most common genitourinary conditions, regularly causing discomfort and concern, especially among women. Though both conditions can affect similar anatomical regions and share overlapping symptoms—such as pain and irritation—their causes, symptoms, and treatments differ significantly. Recognizing these differences helps ensure proper diagnosis, effective treatment, and relief for sufferers.
Summary Table: UTI vs. Yeast Infection
| Symptom | UTI | Yeast Infection |
|---|---|---|
| Pain or burning during urination | ✔️ | ✔️ |
| Frequent urge to urinate | ✔️ | ❌ |
| Lower abdominal pressure | ✔️ | ❌ |
| Blood in urine | ✔️ | ❌ |
| Cloudy or odorous urine | ✔️ | ❌ (discharge odorless) |
| Vaginal itchiness | ❌ | ✔️ |
| Thick, whitish vaginal discharge | ❌ | ✔️ |
| Swelling of vagina/vulva | ❌ | ✔️ |
How to Tell the Difference: Core Symptoms
- Yeast Infection: Causes intense itching, burning, irritation, and swelling of the vagina and vulva. Characterized by a thick, white (cottage cheese-like) and usually odorless discharge. Pain may occur during urination but is due to external irritation.
- UTI: Primarily causes pain or burning during urination, frequent or urgent need to urinate (even with little output), lower abdominal pain, and sometimes blood or a strong odor in urine. Vaginal itching and discharge are not typical.
Understanding these symptom distinctions is crucial because the two infections often require different treatments and can lead to complications if misdiagnosed.
What Causes Yeast Infections?
- Organism: Overgrowth of Candida fungus, normally present in small quantities within the vaginal ecosystem.
- Triggers and Risk Factors:
- Recent antibiotic use (which disrupts normal bacterial balance)
- Diabetes
- Hormonal changes (including pregnancy, birth control)
- Immunosuppressive medications (e.g., steroids, chemotherapy)
- Tight or non-breathable clothing, excessive sweating
If you find yourself facing the discomfort of a yeast infection, understanding various treatment options is crucial. Discovering effective home remedies and prevention tips for yeast infections can empower you to tackle the symptoms head-on while promoting long-term health. These practical strategies can significantly improve your quality of life and prevent future infections.
When the balance of microbes in the vagina is disturbed, Candida may multiply and cause symptomatic infection.
What Causes Urinary Tract Infections?
- Organism: Most UTIs are caused by bacteria, especially Escherichia coli (E. coli), which normally lives in the digestive tract.
- Risk Factors:
- Female anatomy (shorter urethra and proximity to rectum)
- Increased sexual activity
- Poor hygiene or wiping from back to front
- Older age
- Diabetes and obesity
If you're experiencing discomfort or unusual symptoms, it’s vital to understand the complexities of vaginal health. Exploring our guide on understanding vaginal rashes: causes, symptoms, diagnosis, and treatment can equip you with valuable knowledge. This resource will help identify potential issues and facilitate informed discussions with your healthcare provider.
Bacteria can ascend the urinary tract, affecting the bladder (cystitis), urethra (urethritis), and occasionally the kidneys (pyelonephritis).
How Are Yeast Infections and UTIs Diagnosed?
- Anamnesis (medical history and symptoms)
- Physical exam (inspection of vulva and vagina for yeast infection)
- Urine sample (testing for bacteria, blood, or inflammatory cells for UTI)
- Lab tests (microscopic analysis, cultures of vaginal discharge or urine)
Doctors sometimes treat based on symptoms, but laboratory confirmation is valuable for distinguishing the infections and ensuring accurate therapy.
Does a Yeast Infection Cause a UTI?
No, a yeast infection itself does not directly cause a UTI. However, factors disrupting vaginal flora—such as antibiotics—can increase risk for both conditions. Both can occur simultaneously, but treating one does not automatically resolve the other.
Is It Possible to Have Both a UTI and Yeast Infection at the Same Time?
Yes. There’s no direct causal connection, but shared risk factors may mean they occur together, particularly after antibiotic use or disruptions in normal vaginal health.
Treatment Options
Yeast Infection Treatments
- Antifungal medications: Oral (e.g., fluconazole) or topical (e.g., clotrimazole, miconazole) creams/suppositories are standard.
- Duration: Most topical courses run 1–7 days. Oral therapy is generally a single dose.
- Supportive care: Wear loose-fitting cotton underwear, avoid irritants (douches, scented products).
- When to seek help: If symptoms persist, worsen, or recur frequently.
UTI Treatments
- Antibiotics: Chosen according to organism and sensitivity (common options: nitrofurantoin, trimethoprim-sulfamethoxazole, or fosfomycin).
- Supportive care: Hydration, urinary analgesics for pain (e.g., phenazopyridine).
- When to seek help: Signs of kidney infection (back pain, fever, vomiting) or blood in urine warrant urgent medical attention.
Odor Differences
- UTI: Urine may appear cloudy, discolored, and carry a strong, sometimes foul odor.
- Yeast infection: Discharge remains thick, white, and typically odorless.
Itching Differences
- UTI: Itching is rarely experienced. Discomfort is centered on the urinary tract, not external genitalia.
- Yeast infection: Severe itching and burning of the vulva and vaginal area are hallmark symptoms, often accompanied by swelling.
Complications and When to See a Doctor
- UTIs: Untreated infections can progress to painful kidney infections that may be dangerous. Seek medical care if symptoms include high fever, chills, vomiting, or flank pain.
- Yeast infections: Chronic, recurrent yeast infections may indicate underlying health issues or immune problems and require medical evaluation.
If you are unsure which infection you have, consult a healthcare provider for proper testing and diagnosis.
Prevention Strategies
- For UTIs:
- Wipe from front to back
- Urinate after sexual intercourse
- Stay hydrated and do not hold urine for extended periods
- Avoid using irritating feminine hygiene products
- For Yeast Infections:
- Avoid overly tight or non-breathable clothing
- Limit use of scented soaps, douches, or vaginal sprays
- Manage blood sugar if diabetic
- Use antibiotics only as directed by a doctor
- Maintain good vaginal hygiene
Although prevention is not always possible, adopting these practices can lower risk for both infections.
Frequently Asked Questions (FAQs)
Q: Can a yeast infection quickly become a UTI?
A: No, they are different conditions with distinct causes. However, vaginal flora imbalance can increase vulnerability to both, especially after use of antibiotics.
Q: Is sexual activity a risk factor for both?
A: Yes. Sexual activity can introduce bacteria into the urinary tract (UTI risk) and also disrupt the normal vaginal microenvironment (yeast infection risk).
Q: Can men get yeast infections or UTIs?
A: While UTIs are much rarer in men, they do occur, especially with prostate problems. Men can get yeast infections, typically in the groin area or as oral thrush, but vaginal yeast infections are exclusive to women.
Q: Should I avoid intercourse until treated?
A: Yes, it’s wise to wait until your infection resolves to reduce symptoms, avoid passing infection or causing further irritation.
Diagnosis Process at a Glance
- Assess symptoms (itching, discharge, urination pain, frequency)
- Physical examination (vulva, vagina, abdomen)
- Laboratory testing (urine test for UTI, vaginal swab for yeast)
- Further testing as needed for recurrent or complex cases
When to Seek Emergency Medical Attention
- If experiencing severe pain, high fever, vomiting, or back pain
- If blood is present in urine or discharge
- Symptoms persisting or recurring despite treatment
Takeaway: Importance of Accurate Diagnosis
While UTIs and yeast infections can cause overlapping discomfort, their symptoms, causes, and treatments differ. Quick, accurate diagnosis and appropriate therapy are essential to avoid complications and restore comfort. If in doubt, always consult your healthcare provider for testing and treatment advice.
Further Resources and Support
- Talk to your doctor for personalized advice and care plans.
- Visit reputable healthcare sites for information (CDC, Mayo Clinic, Planned Parenthood).
- Consult a pharmacist for over-the-counter remedies and support.
References
- https://flo.health/menstrual-cycle/health/symptoms-and-diseases/yeast-infection-vs-uti
- https://www.baptisthealth.com/blog/health-and-wellness/uti-vs-yeast-infection
- https://www.goodrx.com/conditions/urinary-tract-infection/uti-or-yeast-infection
- https://www.healthline.com/health/yeast-infection-vs-urinary-tract-infection
- https://www.monistat.com/vaginal-health-blog-articles/it-uti-or-yeast-infection-learn-how-to-tell-difference
- https://www.ynhhs.org/articles/difference-between-yeast-infection-kidney-infection-bladder-infection-and-uti
- https://foxvalleyobgyn.com/blog/the-complete-guide-to-understanding-yeast-infections-and-utis/
- https://www.twentyeighthealth.com/sex-health-guide/utis-vs-yeast-infections-how-to-tell-the-difference
- https://www.everlywell.com/blog/virtual-care/uti-vs-yeast-infection/
Read full bio of Sneha Tete












