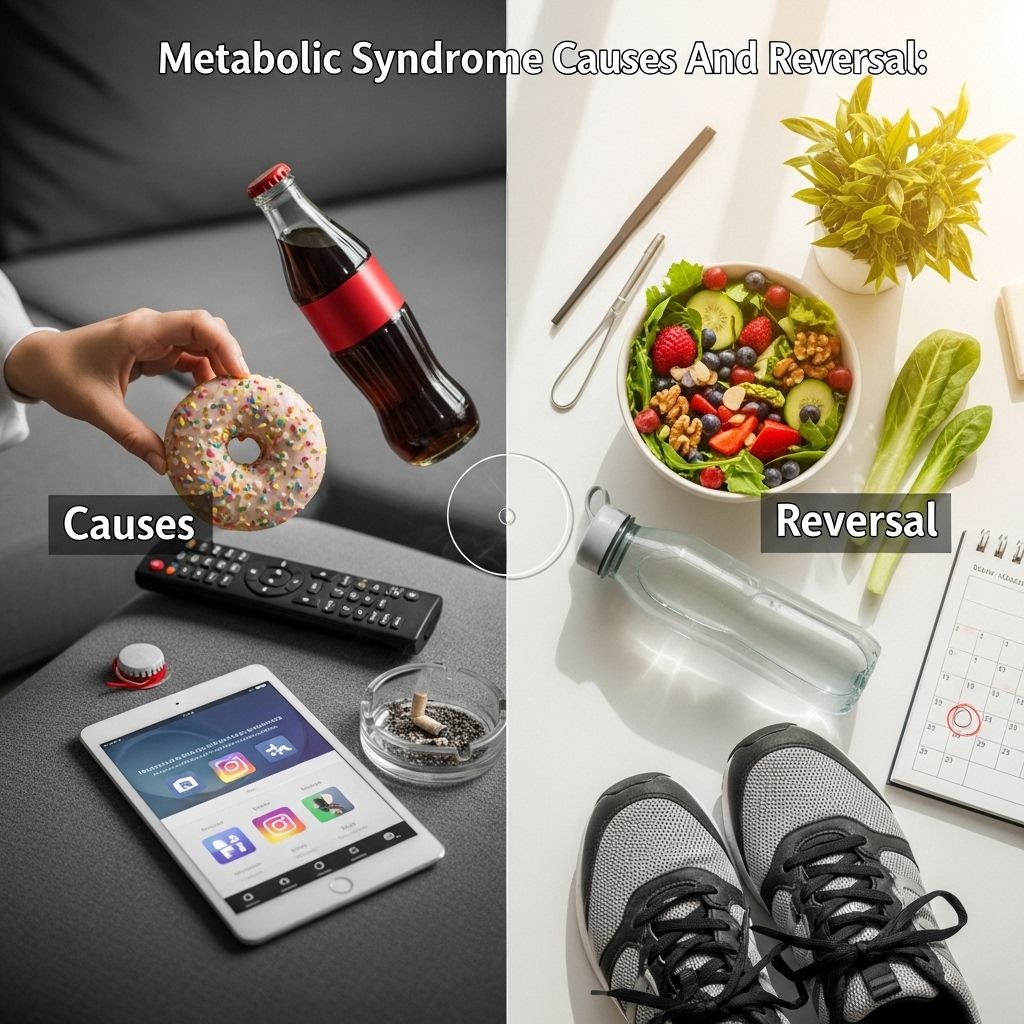
What is Metabolic Syndrome? Complete Guide to Causes & Reversal
Addressing hidden risk factors with simple lifestyle shifts can transform your well-being.
Metabolic syndrome represents one of the most significant health challenges of our time, affecting approximately one in three adults in developed countries. This cluster of interconnected conditions dramatically increases the risk of cardiovascular disease, type 2 diabetes, and stroke, making it a critical health concern that demands immediate attention and understanding.
Table of Contents
- Understanding Metabolic Syndrome
- Diagnostic Criteria and Components
- Symptoms and Warning Signs
- Root Causes and Risk Factors
- Health Consequences and Complications
- Proven Reversal Strategies
- Dietary Interventions
- Lifestyle Modifications
- Medical Management
- Frequently Asked Questions
Understanding Metabolic Syndrome
Metabolic syndrome, also known as syndrome X or insulin resistance syndrome, is not a single disease but rather a constellation of interconnected metabolic abnormalities that occur together more frequently than would be expected by chance. This clustering of conditions creates a dangerous synergy that exponentially increases health risks beyond what each individual component would contribute alone.
The syndrome represents a fundamental disruption in how the body processes energy, stores fat, and regulates blood sugar levels. At its core, metabolic syndrome reflects the body’s inability to effectively manage the modern lifestyle characterized by processed foods, sedentary behavior, and chronic stress. The condition affects virtually every organ system and represents a state of chronic metabolic dysfunction that, if left unchecked, progresses to serious disease states.
Diagnostic Criteria and Components
Healthcare providers diagnose metabolic syndrome when a patient presents with at least three of the following five key components:
Central Obesity
Abdominal or visceral obesity, characterized by excessive fat accumulation around the waistline, is perhaps the most visible component of metabolic syndrome. The diagnostic criteria specify a waist circumference of more than 40 inches (102 cm) in men and more than 35 inches (89 cm) in women. This type of fat distribution, often described as “apple-shaped,” is particularly dangerous because visceral fat actively produces inflammatory substances and hormones that disrupt normal metabolic processes.
Elevated Blood Pressure
Hypertension is defined as blood pressure readings of 130/85 mmHg or higher, or current use of antihypertensive medications. This component reflects the cardiovascular strain associated with metabolic dysfunction and often develops silently, earning hypertension the nickname “the silent killer.”
Dyslipidemia
The lipid abnormalities in metabolic syndrome include two specific patterns: elevated triglycerides (150 mg/dL or higher) and reduced HDL cholesterol levels (less than 40 mg/dL in men and less than 50 mg/dL in women). This dyslipidemic profile promotes atherosclerosis and significantly increases cardiovascular risk.
Insulin Resistance and Glucose Intolerance
Elevated fasting blood glucose levels of 100 mg/dL or higher indicate impaired glucose metabolism and insulin resistance. This component often represents the early stages of type 2 diabetes development and reflects the body’s diminishing ability to regulate blood sugar effectively.
| Component | Diagnostic Threshold | Clinical Significance |
|---|---|---|
| Waist Circumference | Men: >40 inches, Women: >35 inches | Indicates visceral obesity and inflammation |
| Blood Pressure | ≥130/85 mmHg | Cardiovascular strain and arterial damage |
| Triglycerides | ≥150 mg/dL | Increased atherosclerotic risk |
| HDL Cholesterol | Men: <40 mg/dL, Women: <50 mg/dL | Reduced cardioprotective factors |
| Fasting Glucose | ≥100 mg/dL | Insulin resistance and diabetes risk |
Symptoms and Warning Signs
Many components of metabolic syndrome develop silently, making early detection challenging. However, several warning signs may indicate the presence of this condition:
Physical Symptoms
The most obvious physical manifestation is the accumulation of abdominal fat, creating an “apple-shaped” body profile. Patients may also experience symptoms related to elevated blood glucose levels, including increased thirst, frequent urination, fatigue, and blurred vision. Some individuals report difficulty losing weight despite dietary efforts and experience persistent hunger or cravings for carbohydrates.
Subtle Indicators
Less obvious symptoms include skin changes such as acanthosis nigricans (dark, velvety patches of skin, particularly around the neck and armpits), which indicates insulin resistance. Sleep disturbances, mood changes, and decreased energy levels are also common but often overlooked indicators of metabolic dysfunction.
Root Causes and Risk Factors
The development of metabolic syndrome results from a complex interplay of genetic, environmental, and lifestyle factors. Understanding these root causes is essential for effective prevention and treatment strategies.
Insulin Resistance: The Central Mechanism
Insulin resistance stands as the primary driver of metabolic syndrome. This condition occurs when cells in muscles, fat tissue, and the liver become less responsive to insulin, the hormone responsible for regulating blood glucose levels. When cells resist insulin’s effects, the pancreas compensates by producing more insulin, leading to hyperinsulinemia. This excess insulin contributes to weight gain, particularly around the abdomen, and triggers a cascade of metabolic abnormalities.
Lifestyle Factors
Modern lifestyle patterns significantly contribute to metabolic syndrome development. Sedentary behavior reduces muscle glucose uptake and promotes weight gain. Poor dietary choices, particularly excessive consumption of processed foods high in refined sugars and unhealthy fats, overwhelm the body’s metabolic capacity. Chronic stress elevates cortisol levels, which promotes abdominal fat storage and insulin resistance.
Genetic Predisposition
Genetic factors influence individual susceptibility to metabolic syndrome. Certain ethnic groups, including Hispanic Americans, African Americans, and Asian Americans, show higher rates of the condition. Family history of diabetes, cardiovascular disease, or obesity also increases risk, suggesting inherited metabolic vulnerabilities.
Age and Hormonal Changes
The risk of metabolic syndrome increases with age due to natural changes in body composition, hormone levels, and cellular function. Menopause in women and andropause in men alter hormone profiles in ways that promote weight gain and metabolic dysfunction.
Health Consequences and Complications
Metabolic syndrome dramatically increases the risk of serious health complications, making early intervention crucial for long-term health outcomes.
Cardiovascular Disease
Individuals with metabolic syndrome face a two to three-fold increased risk of heart disease and stroke. The combination of hypertension, dyslipidemia, and insulin resistance accelerates atherosclerosis, leading to coronary artery disease, heart attacks, and stroke. The inflammatory state associated with metabolic syndrome further compounds cardiovascular risk.
Type 2 Diabetes
Metabolic syndrome increases the risk of developing type 2 diabetes by approximately five-fold. The progressive insulin resistance eventually overwhelms the pancreas’s ability to produce sufficient insulin, leading to persistent hyperglycemia and diabetes diagnosis.
Additional Complications
Beyond cardiovascular disease and diabetes, metabolic syndrome is associated with numerous other health problems including non-alcoholic fatty liver disease, sleep apnea, polycystic ovary syndrome in women, chronic kidney disease, and certain cancers. These complications underscore the systemic nature of metabolic dysfunction.
Proven Reversal Strategies
The encouraging news about metabolic syndrome is that it is largely preventable and reversible through comprehensive lifestyle interventions. Research consistently demonstrates that targeted changes in diet, physical activity, and lifestyle habits can effectively reverse the components of metabolic syndrome.
Weight Management
Even modest weight loss of 5-10% of body weight can significantly improve all components of metabolic syndrome. Weight reduction decreases insulin resistance, lowers blood pressure, improves lipid profiles, and reduces abdominal fat accumulation. The key is sustainable, gradual weight loss achieved through balanced approaches rather than extreme measures.
Physical Activity Prescription
Regular physical activity serves as a powerful medicine for metabolic syndrome. Both aerobic exercise and resistance training contribute to reversal, with combined approaches showing optimal results. Aerobic exercise improves insulin sensitivity and cardiovascular health, while resistance training builds muscle mass, which increases glucose uptake and metabolic rate.
Dietary Interventions
Nutrition forms the cornerstone of metabolic syndrome reversal, with specific dietary patterns showing remarkable effectiveness in improving metabolic health.
Mediterranean Diet Approach
The Mediterranean diet, rich in vegetables, fruits, whole grains, legumes, nuts, olive oil, and moderate amounts of fish, has demonstrated superior effectiveness in reversing metabolic syndrome. This eating pattern reduces inflammation, improves insulin sensitivity, and promotes healthy weight management while providing sustainable, enjoyable meal options.
Carbohydrate Quality and Timing
Focus on complex carbohydrates with high fiber content while minimizing refined sugars and processed starches. Distributing carbohydrate intake throughout the day and combining carbohydrates with protein and healthy fats helps stabilize blood glucose levels and reduce insulin spikes.
Portion Control and Mindful Eating
Implementing portion control strategies and practicing mindful eating techniques help address overconsumption and promote better metabolic health. These approaches include eating slowly, recognizing hunger and satiety cues, and avoiding distractions during meals.
Lifestyle Modifications
Stress Management
Chronic stress contributes significantly to metabolic syndrome through cortisol elevation and behavioral changes. Effective stress management techniques include meditation, yoga, deep breathing exercises, and regular relaxation practices. These interventions can lower cortisol levels and reduce stress-induced eating behaviors.
Sleep Optimization
Quality sleep is essential for metabolic health. Poor sleep disrupts hormones that regulate hunger and satiety while increasing insulin resistance. Establishing consistent sleep schedules, creating optimal sleep environments, and addressing sleep disorders like sleep apnea are crucial components of metabolic syndrome reversal.
Smoking Cessation and Alcohol Moderation
Smoking cessation and limiting alcohol consumption support metabolic health improvement. Smoking increases insulin resistance and cardiovascular risk, while excessive alcohol consumption contributes to weight gain and metabolic dysfunction.
Medical Management
While lifestyle interventions remain the primary treatment approach, medical management may be necessary for certain individuals, particularly those with advanced metabolic dysfunction or multiple risk factors.
Pharmacological Interventions
Medications may be prescribed to address specific components of metabolic syndrome when lifestyle measures prove insufficient. These may include antihypertensive medications for blood pressure control, statins for dyslipidemia, and metformin for insulin resistance and glucose management.
Monitoring and Follow-up
Regular medical monitoring ensures that interventions are effective and allows for timely adjustments in treatment plans. This includes periodic assessment of all metabolic syndrome components and screening for complications.
Frequently Asked Questions
Q: Can metabolic syndrome be completely reversed?
A: Yes, metabolic syndrome can often be completely reversed through comprehensive lifestyle changes including weight loss, regular physical activity, and dietary improvements. Many people can normalize all components with sustained efforts.
Q: How long does it take to reverse metabolic syndrome?
A: Improvements can begin within weeks of implementing lifestyle changes, but complete reversal typically takes several months to a year of consistent efforts, depending on individual factors and severity.
Q: Is metabolic syndrome genetic?
A: While genetics play a role in susceptibility, lifestyle factors are the primary drivers. Even those with genetic predisposition can prevent or reverse metabolic syndrome through appropriate interventions.
Q: What is the most important component to address first?
A: Weight management and physical activity typically provide the most comprehensive benefits, as they simultaneously address multiple components of metabolic syndrome including insulin resistance, blood pressure, and lipid levels.
Q: Can children develop metabolic syndrome?
A: Yes, metabolic syndrome is increasingly recognized in children and adolescents, primarily related to childhood obesity and sedentary lifestyles. Early intervention is crucial for preventing long-term complications.
Metabolic syndrome represents a critical health challenge, but one that responds remarkably well to comprehensive lifestyle interventions. By understanding its causes and implementing proven reversal strategies, individuals can not only overcome this condition but also achieve optimal metabolic health and significantly reduce their risk of serious complications. The key lies in taking action early and maintaining consistent, sustainable changes that support long-term health and vitality.
References
- https://my.clevelandclinic.org/health/diseases/10783-metabolic-syndrome
- https://medlineplus.gov/metabolicsyndrome.html
- https://www.healthdirect.gov.au/metabolic-syndrome
- https://www.medicalnewstoday.com/articles/263834
- https://www.nhlbi.nih.gov/health/metabolic-syndrome/causes
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2675814/
Read full bio of medha deb












