Vitamin D’s Role in Barrier Function: Immune and Gut Health Explored for Optimal Well-Being
Reinforcing your body’s natural shields and promoting balance from within.
Vitamin D’s Role in Barrier Function: Immune and Gut Health Explored
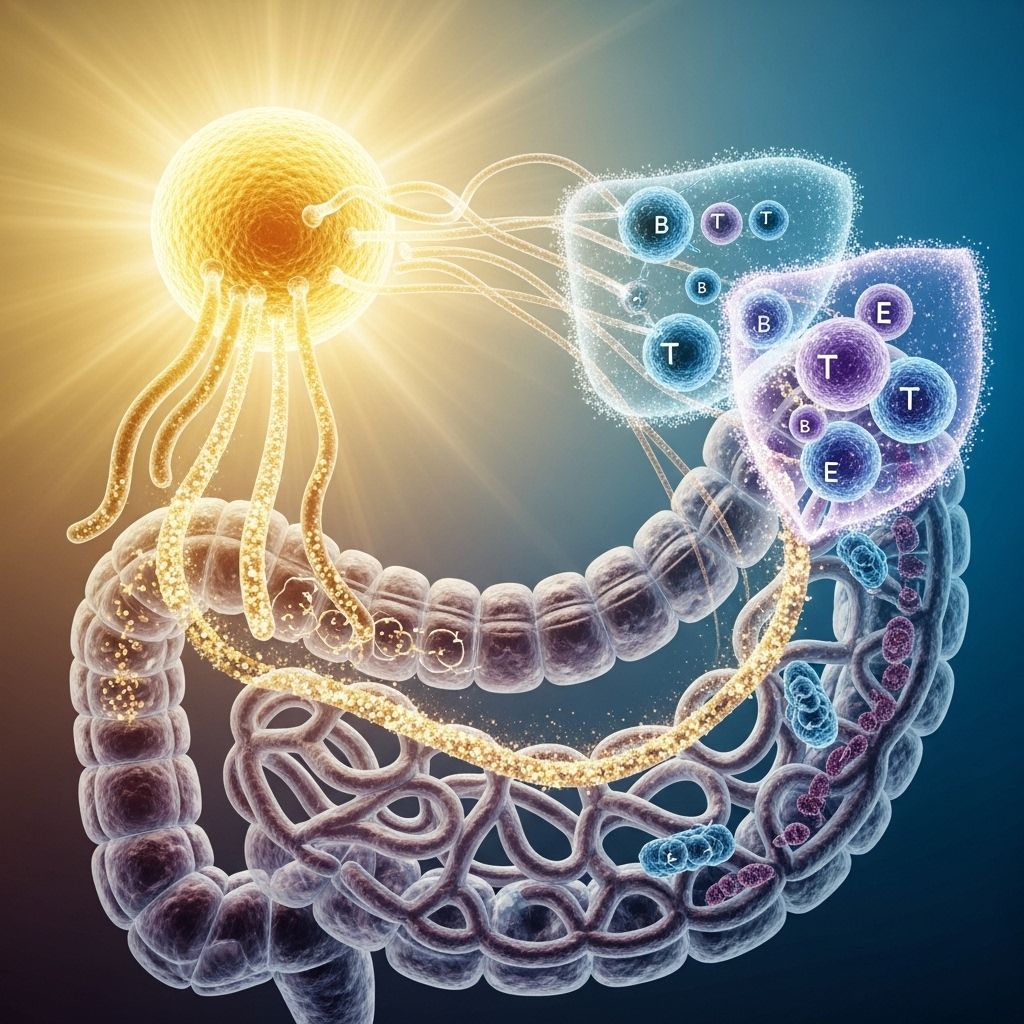
Vitamin D, long recognized for its role in bone metabolism, has emerged as a powerful regulator of both immune defenses and intestinal barrier integrity. Mounting evidence indicates that vitamin D’s influence extends to cellular immunity, inflammation, and the preservation of physical barriers that protect against external threats. In this comprehensive article, we delve into the mechanisms through which vitamin D supports barrier functions in both the immune and gastrointestinal systems, and review the implications for health, disease prevention, and therapeutic strategies.
Table of Contents
- Introduction: The Vital Role of Barrier Function in Health
- Vitamin D and Immune Barrier Regulation
- Vitamin D’s Impact on Gut Barrier Integrity
- Cellular and Molecular Mechanisms
- Consequences of Vitamin D Deficiency on Barriers
- Clinical Implications and Therapeutic Perspectives
- Frequently Asked Questions (FAQ)
- Key Takeaways
- References
Introduction: The Vital Role of Barrier Function in Health
Physical and immunological barriers are critical to the body’s defense against environmental threats, including pathogens and toxins. These barriers are not only passive physical walls but also involve active immunological surveillance, communication, and repair mechanisms. Key elements include:
- Intestinal epithelium – Acts as a selective filter, absorbing nutrients while restricting pathogen entry.
- Immune cells – Constantly sample and respond to threats at barrier sites.
- Tight junctions and mucus – Maintain compartmentalization and protect underlying tissues.
Vitamin D, primarily produced in the skin via sunlight exposure and supplemented through diet, interacts with these barriers at multiple levels, influencing both structural integrity and immunological responses.
Vitamin D and Immune Barrier Regulation
Vitamin D modulates immunity through direct and indirect effects on various immune cells, enhancing barrier functions and promoting a balanced response to potential threats. The biologically active form, calcitriol (1,25-dihydroxyvitamin D3), exerts its effects by binding the vitamin D receptor (VDR), which is expressed in many cell types, including those integral to the immune system.
Innate Immune System
- Antimicrobial peptide production: Vitamin D upregulates cathelicidin and β-defensin expression, critical molecules that disrupt bacteria, viruses, and fungi upon first contact with barrier surfaces.
- Modulation of innate immune cell function: Vitamin D influences monocytes, macrophages, and neutrophils by regulating cytokine production, promoting an anti-inflammatory M2 phenotype, and limiting excessive inflammation.
- Toll-like receptors (TLRs): It increases the expression of TLR2 and NOD2, enhancing pathogen recognition while mitigating excessive activation.
Adaptive Immune System
- Promoting immune tolerance: Vitamin D drives the differentiation of tolerogenic dendritic cells and regulatory T cells (Tregs), dampening aberrant immune activation and supporting tissue repair.
- Balancing helper T cell responses: It inhibits proinflammatory Th1 and Th17 cell differentiation while favoring Th2 and Treg polarization.
- B-cell regulation: Vitamin D limits B-cell proliferation and lowers antibody (IgG, IgM) production, preventing overactive humoral immunity.
Vitamin D and Epithelial Barrier Immune Surveillance
The mucosal epithelium in organs like the gut is patrolled by specialized immune cells such as innate lymphoid cells, dendritic cells (DCs), and resident macrophages. Vitamin D signaling fortifies these defenses by:
- Enhancing the barrier’s antimicrobial surface arsenal
- Facilitating clearance of penetrant microbes while promoting restoration of homeostasis
- Modulating cytokine secretion to prevent chronic inflammation
| Cell Type | Vitamin D Action | Barrier Implication |
|---|---|---|
| Innate lymphoid cells | Enhances VDR, antimicrobial gene transcription | Improves mucosal defense, limits pathogen colonization |
| Macrophages | Promotes anti-inflammatory (M2) phenotype, AMP production | Facilitates resolution of inflammation and tissue repair |
| Dendritic cells | Encourages tolerogenic state, limits overactivation | Reduces risk of autoimmunity at barrier sites |
| T and B lymphocytes | Promotes Treg development, limits excessive antibody release | Preserves immune homeostasis at epithelium |
Vitamin D’s Impact on Gut Barrier Integrity
The gut serves as a frontline of environmental interaction, constantly exposed to dietary and microbial antigens. Its physical barrier is formed by a single layer of epithelial cells sealed by tight junctions, covered by protective mucus, and reinforced by immune sentinels.
Vitamin D Receptors in the Gut
- VDR is expressed throughout the intestinal tract, especially on epithelial and key immune cells.
- Activation of VDR regulates expression of genes critical for junctional integrity, mucosal immunity, and microbial homeostasis.
Molecular Mechanisms of Barrier Support
- Strengthening tight junctions: Active vitamin D upregulates claudins, occludin, and ZO-1, minimizing paracellular leakiness.
- Enhancement of mucus and antimicrobial peptide production: Defends against bacterial penetration and maintains optimal microbial ecology.
- Blunting of proinflammatory cascades: By restricting Th1/Th17 activation and proinflammatory cytokine secretion, vitamin D curbs chronic injury to the gut lining.
Vitamin D, Microbiota, and Homeostasis
- Vitamin D helps regulate gut microbiota composition, fostering a healthy community structure and containing overgrowth of harmful organisms.
- Impaired vitamin D signaling disrupts this balance, leading to dysbiosis and increased risk of infection and inflammation.
Cellular and Molecular Mechanisms
Vitamin D acts at several levels to maintain robust barrier defense:
- Direct genomic effects: Calcitriol-VDR complexes activate or repress hundreds of genes related to immunity, inflammation, and cellular repair.
- AMP (antimicrobial peptide) regulation: Vitamin D stimulates production of cathelicidin and β-defensin, which directly neutralize pathogens at the barrier surface.
- Tight junction reinforcement: Promotes the production and localization of proteins (such as claudin-1, ZO-1) that form the seals between gut epithelial cells.
- Immunomodulation: Fosters development of regulatory T cells over proinflammatory Th cells, limiting damage to host tissues during immune activation.
Consequences of Vitamin D Deficiency on Barriers
Low vitamin D jeopardizes both immune and gut barrier function, predisposing to increased inflammation and infectious susceptibility:
- Intestinal consequences: Deficiency is linked to increased gut permeability, loss of tight junction integrity, and greater risk for colonic inflammation and infection.
- Chronic inflammation: Without adequate vitamin D, the immune system is more likely to mount an exaggerated response, inciting tissue-damaging cytokines (e.g., IL-1, IL-6, TNF-α) and promoting chronic inflammatory diseases such as inflammatory bowel disease (IBD).
- Impaired infection clearance: Reduced synthesis of antimicrobials and weakened recruitment of tolerogenic immune cells delay recovery from gut infections and increase damage.
Case Study Table: Risks of Vitamin D Deficiency
| Barrier Function | Effect of Deficiency | Clinical Consequences |
|---|---|---|
| Gut Epithelial Integrity | Disruption of tight junctions | Increased “leaky gut”, risk of IBD, food allergies |
| Immune Surveillance | Overactive or unbalanced immunity | Greater susceptibility to infections, autoimmunity |
| Antimicrobial Defenses | Reduced AMP production | Slower pathogen clearance, chronic infection |
Clinical Implications and Therapeutic Perspectives
Understanding vitamin D’s impact on immune and gut barrier function highlights its importance beyond bone health, with major implications for disease prevention and treatment. Considerations include:
- Optimization of vitamin D status: Avoidance of severe deficiency benefits immune health and reduces risk of infection and inflammatory disease.
- Potential for adjunct therapy: Vitamin D supplementation may complement existing treatments for autoimmune, infectious, and inflammatory disorders affecting barrier tissues.
- Individual variability: Requirements and responses can differ based on genetics, age, chronic disease, and environmental factors.
Current guidelines emphasize maintaining vitamin D sufficiency (serum 25(OH)D levels typically above 30 ng/mL), but optimal targets for immunological and barrier protection may vary, and ongoing research continues to refine these recommendations.
Frequently Asked Questions (FAQ)
Q: How does vitamin D help prevent gut “leakiness”?
Vitamin D maintains and repairs the tight junction proteins in intestinal epithelial cells, ensuring a selective barrier that blocks harmful substances and microbes from entering the bloodstream while permitting nutrient absorption. This action reduces the risk of “leaky gut” and its related inflammatory consequences.
Q: Can vitamin D help reduce the risk of autoimmune or inflammatory diseases of the gut?
Evidence suggests that adequate vitamin D helps modulate immune responses in the gut, lowers chronic proinflammatory signaling, and supports regulatory T cell function, thereby decreasing the risk or severity of autoimmune disorders such as Crohn’s disease or ulcerative colitis.
Q: What are the best sources of vitamin D for barrier support?
The primary natural source is sunlight-driven synthesis in the skin; dietary sources include fatty fish, fortified foods, and supplements. Clinical monitoring of vitamin D levels is especially important in individuals with limited sun exposure, dark skin, or existing gastrointestinal disease.
Q: How quickly can vitamin D supplementation impact barrier function?
While some immune and barrier effects may occur within weeks of supplementation, broader improvements—such as reduced infection frequency or inflammation—can take longer and may depend on correcting an existing deficiency. Individual response times may vary.
Q: Should I take vitamin D to help with gut or immune issues?
Consult with a healthcare provider who can assess vitamin D status, recommend personalized supplementation if needed, and monitor progress as part of a comprehensive care plan. Self-medication without guidance is not advised, especially at high doses.
Key Takeaways
- Vitamin D supports both immune and gut barrier function by promoting antimicrobial defenses, maintaining structural integrity, and regulating immunological tolerance.
- Deficiency weakens barrier defenses, increases inflammation, and heightens susceptibility to infection and chronic disease.
- Optimizing vitamin D status—via safe sun exposure, diet, and supplements when needed—is a foundational strategy for barrier protection and overall health resilience.
References
- Vitamin D’s Effect on Immune Function – PMC – PubMed Central
- Vitamin D and immunomodulation in the skin: a useful affirmative – ExplorationPub
- Vitamin D Deficiency Promotes Epithelial Barrier Dysfunction and Colonic Injury – Journal of Infectious Diseases
- Vitamin D and intestinal homeostasis: Barrier, microbiota – PubMed
References
Read full bio of Sneha Tete












