Understanding Vaginal Rashes: Causes, Symptoms, Diagnosis, and Treatment
Discover relief paths and prevention tips for healthier, more comfortable intimate skin.
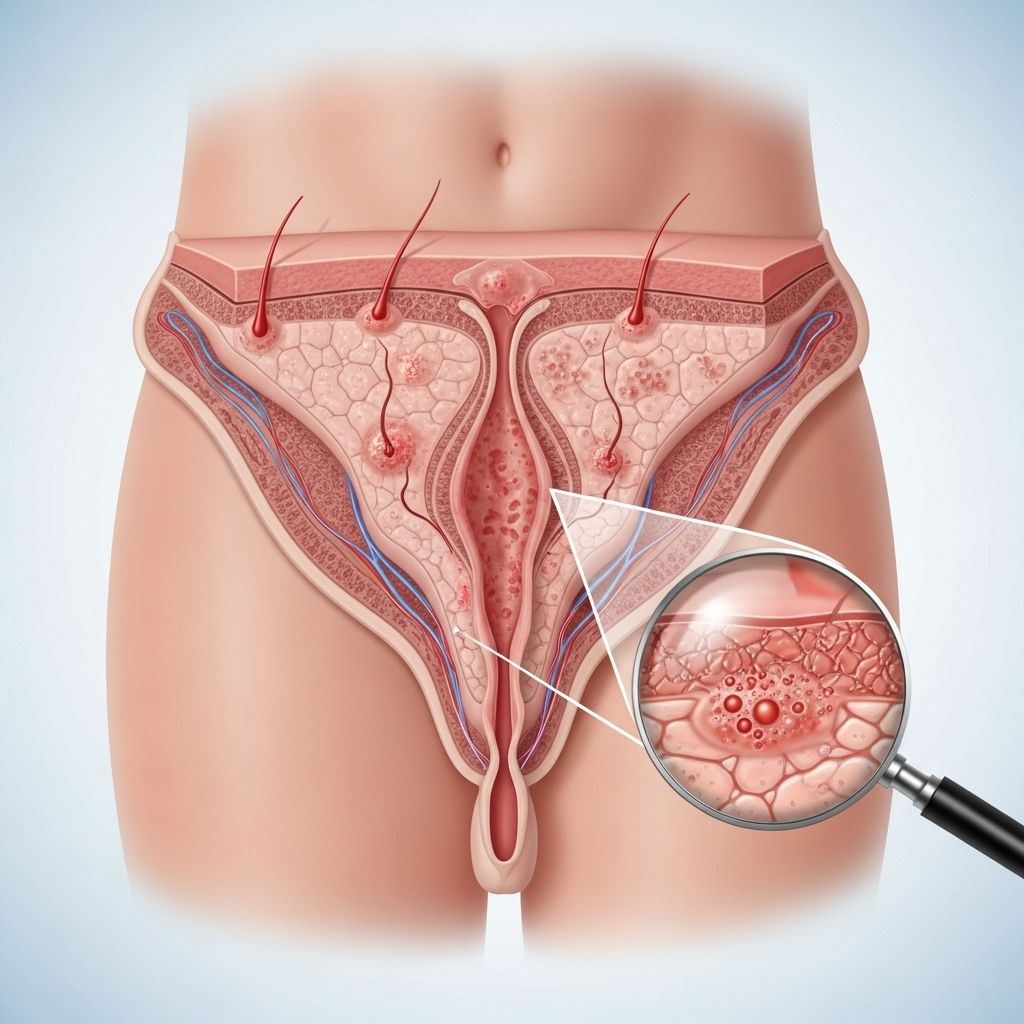
Vaginal rash is a common yet often misunderstood condition that can cause significant discomfort and distress. While the term “vaginal rash” is frequently used, such rashes typically occur on the external genital areas (the vulva) rather than inside the vagina itself. This article provides a thorough exploration of the underlying causes, symptoms, diagnostic processes, treatment options, and prevention strategies for vaginal rashes, empowering you to detect, manage, and seek care effectively.
What Is a Vaginal Rash?
A vaginal rash refers to any irritation, discoloration, or inflammation affecting the vulvar skin. The affected area may include the labia, perineum, groin folds, and surrounding regions. Vaginal rashes can range from mild, self-limiting irritations to intense discomfort and significant skin damage.
- Common symptoms include redness, swelling, itching, burning, bumps, or blisters.
- Rashes may be accompanied by abnormal discharge, painful urination, or pain during sex.
- The severity, duration, and appearance of the rash can vary depending on the underlying cause.
Common Causes of Vaginal Rash
There are numerous potential causes for a vaginal rash. Understanding these can help in identifying the best approach to relief and treatment. The main categories include:
1. Dermatitis and Allergic Reactions
- Contact Dermatitis: Irritation from scented soaps, bubble baths, detergents, fabric softeners, pads, pantyliners, or latex (in condoms or gloves) can trigger a skin reaction. New hygiene products or laundry detergents are often culprits. Symptoms: intense itching, redness, mild swelling, sometimes blisters or bumps.
- Atopic Dermatitis (Eczema): Chronic itchy and inflamed vulvar skin, often linked to a personal or family history of allergies or asthma.
- Allergic Reactions: Reactions to topical medications, spermicides, lubricants, or even latex may also cause rashes.
2. Infections
- Yeast Infections (Candidiasis): Overgrowth of Candida fungus leads to intense itching, redness, swelling, and a thick, white, “cottage cheese”-like discharge. Often triggered by antibiotics, hormonal changes, or immunosuppression.
- Bacterial Vaginosis (BV): Disruption in the usual vaginal bacteria balance can create a rash accompanied by thin, grayish discharge and a fishy odor.
- Sexually Transmitted Infections (STIs):
- Genital Herpes: Causes blistering, painful sores on vulvar skin, often recurring.
- Trichomoniasis: A parasitic infection causing redness, discharge, and discomfort.
- Syphilis: May cause painless sores, progressing to rashes if untreated.
- Human Papillomavirus (HPV): Can cause warts or skin changes.
It's important to differentiate between infections for appropriate treatment. To learn more about this, be sure to explore our comparison of yeast infections and UTIs, which outlines the key differences in their symptoms, causes, and effective treatments. - Molluscum Contagiosum: Viral infection resulting in small, shiny, painless bumps, which may become inflamed if infected.
3. Parasitic Infestations
- Pubic Lice (Crabs): Tiny insects living in pubic hair, causing irritation, itchiness, and sometimes visible eggs (nits).
- Scabies: Infestation by itch mites that burrow into the skin; symptoms include intense itching and a bumpy rash, often worse at night. Spread through skin-to-skin contact or shared bedding/towels.
4. Skin Conditions
- Psoriasis: An autoimmune skin condition that causes thickened, red, scaly patches on the vulva or elsewhere. Scratching can worsen symptoms and may increase the risk of infection.
- Lichen Sclerosus: Chronic skin disorder (mostly postmenopausal women) causing thin, white, patchy skin with itching and discomfort.
- Lichen Planus: Another chronic inflammatory skin disease, leading to purple or red flat-topped bumps and sometimes open sores on the vulva.
5. Other Causes
- Mechanical Irritation: Tight underwear, rough fabrics, prolonged wearing of wet clothing, panty liners, or cycling may cause friction and minor rashes.
- Sweat and Heat: Moisture trapped in the groin area, especially in hot weather, can irritate sensitive vulvar skin.
- Hormonal Changes: Menstruation, pregnancy, or menopause can impact vaginal and vulvar tissue, making it more susceptible to irritation or infection.
Symptoms of a Vaginal Rash
Symptoms can vary depending on the underlying cause, but commonly include:
- Redness or discoloration of the vulva or groin fold
- Intense itching (pruritus)
- Swelling or puffiness
- Dryness, rough patches, or scaling
- Pain or burning sensation (especially during urination or sexual intercourse)
- Bumps, blisters, or open sores
- Changes in vaginal discharge (color, texture, or odor)
How to Diagnose a Vaginal Rash
Getting the right diagnosis is key to effective treatment. Diagnosis usually involves:
- Medical History: Your doctor will ask about symptom onset, duration, menstrual and sexual history, hygiene practices, use of products, and any prior similar episodes.
- Physical Examination: A careful visual inspection of the affected area to assess the rash’s appearance, pattern, and extent.
- Laboratory Tests:
- Swab tests for yeast, bacteria, or STIs
- Microscopy or cultures
- Skin scraping for mites (if scabies is suspected)
- Blood tests (for some chronic causes or difficult cases)
- Patch Testing: Rarely, to determine allergy triggers in persistent or unexplained cases.
Treatment Options for Vaginal Rashes
Treatment depends on the specific cause, but major strategies include:
General Measures
- Discontinue potential irritants (change soaps, detergents, products that touch the area)
- Wear loose, breathable cotton underwear and avoid tight synthetic garments
- Keep the area clean and gently pat dry after washing
- Use cool compresses or sitz baths for soothing relief
- Avoid scratching, which can worsen symptoms or lead to infection
Specific Medical Treatments
| Condition | Treatment |
|---|---|
| Contact Dermatitis | Avoidance of triggers; topical corticosteroids for inflammation |
| Yeast Infection (Candidiasis) | Antifungal creams, suppositories, or oral medications |
| Bacterial Vaginosis | Antibiotics (oral or vaginal) |
| Trichomoniasis | Oral antiprotozoal medication (e.g., metronidazole) |
| Genital Herpes | Antiviral medications (oral or topical) |
| Pubic Lice/Scabies | Prescription creams and thorough cleaning of clothing/bedding |
| Psoriasis/Eczema | Topical steroids, immunomodulators, and moisturizers |
| Lichen Sclerosus/Other Chronic Conditions | Long-term topical steroids; possible referral to a dermatologist |
Prevention: How to Lower the Risk of Vaginal Rashes
Enhancing everyday habits can significantly reduce the likelihood of vaginal rashes. Recommended steps include:
- Use fragrance-free, hypoallergenic soaps and detergents
- Choose breathable, natural-fiber underwear and change underwear daily
- Avoid douching or use of scented feminine hygiene sprays
- Wipe front to back after going to the bathroom
- Change pads, pantyliners, and tampons regularly
- Practice safe sex and use protection with new partners
- Manage underlying conditions (like diabetes) that may predispose to yeast or bacterial infections
When to See a Doctor
You should contact your healthcare provider if:
- Rash is severe, persistent, or recurrent
- Symptoms are accompanied by severe pain, open sores, or blisters
- There is fever, chills, or unexplained abdominal pain
- There is abnormal or foul-smelling discharge
- You suspect you have been exposed to an STI or your partner has symptoms
Prompt medical attention can prevent complications and help identify any underlying health issues.
Frequently Asked Questions (FAQs)
Q: Is a vaginal rash always a sign of a sexually transmitted infection?
A: No. While some STIs may present with a rash, many vaginal rashes are caused by non-infectious factors such as allergies, irritation, eczema, yeast imbalance, or other skin conditions. Determining the cause may require a medical evaluation.
Q: Can I treat a vaginal rash at home?
A: Mild rashes from irritation may resolve with simple measures like avoiding suspected triggers, practicing gentle hygiene, and using fragrance-free products. However, persistent, recurrent, or severe symptoms require professional evaluation and treatment.
Q: How can I differentiate between yeast infection and other causes?
A: Yeast infections often present with intense itching, redness, swelling, and a thick, white, clumpy discharge. Other causes may present with pain, thin discharge, or different types of lesions. Only definitive testing can confirm the diagnosis.
Q: Are there long-term complications from vaginal rashes?
A: Most mild rashes heal without permanent effects, but untreated underlying infections or chronic skin disorders can cause scarring, pigment changes, or spread infection. Accurate diagnosis and prompt management are important to prevent complications.
Q: What should I avoid if I have a vaginal rash?
A: Avoid scratching, harsh soaps, douches, perfumed products, tight clothing, and activities that aggravate symptoms, like cycling or swimming in chlorinated pools. Stick to gentle cleansing and loose, breathable clothing until healed.
Key Takeaways
- A vaginal rash is usually a vulvar issue and can be caused by a wide range of factors, from mild irritants to more serious infections.
- Symptoms such as itching, burning, and redness require prompt self-care and, if persistent, professional evaluation.
- Simple measures—like using gentle products and practicing safe hygiene—can often prevent many common rashes.
- If in doubt, see a healthcare provider for personalized advice, accurate diagnosis, and safe, effective treatment.
References
- https://www.medicalnewstoday.com/articles/vaginal-rash
- https://www.swingwomenswellness.com/services/vaginal-rashes-and-sores/
- https://www.webmd.com/sexual-conditions/rash-near-vagina
- https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=tw12153
- https://myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=tm7035
- https://my.clevelandclinic.org/health/diseases/24336-vulvar-dermatitis
- https://www.healthdirect.gov.au/vaginal-irritation-and-infection
- https://my.clevelandclinic.org/health/diseases/15175-vulvitis
Read full bio of medha deb












