Understanding the Menstrual Cycle Phases: A Complete Guide
Discover how shifting hormone levels shape your mood, energy, and fertility every month.
Understanding the Menstrual Cycle: An In-Depth Guide
The menstrual cycle is a complex, dynamic process involving hormonal and physiological changes designed to prepare the body for possible pregnancy every month. While many associate the cycle with menstruation itself, it is composed of four distinct sequential phases, each playing a crucial role in reproductive health. This guide explores each phase, associated hormonal changes, common symptoms, and frequently asked questions, providing a holistic understanding for anyone wishing to learn more about their cycle.
What Is the Menstrual Cycle?
The menstrual cycle refers to the recurring series of events that occur in the female reproductive system, typically ranging between 21 to 35 days in length, although the classic “average” is 28 days. Every cycle starts with menstruation (period) and ends the day before the next period begins. While most people notice the physical changes during menstruation, the cycle is driven by a complex interplay of key reproductive hormones: estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH). Understanding this cycle is essential for recognizing fertility patterns, diagnosing reproductive issues, and managing health concerns.
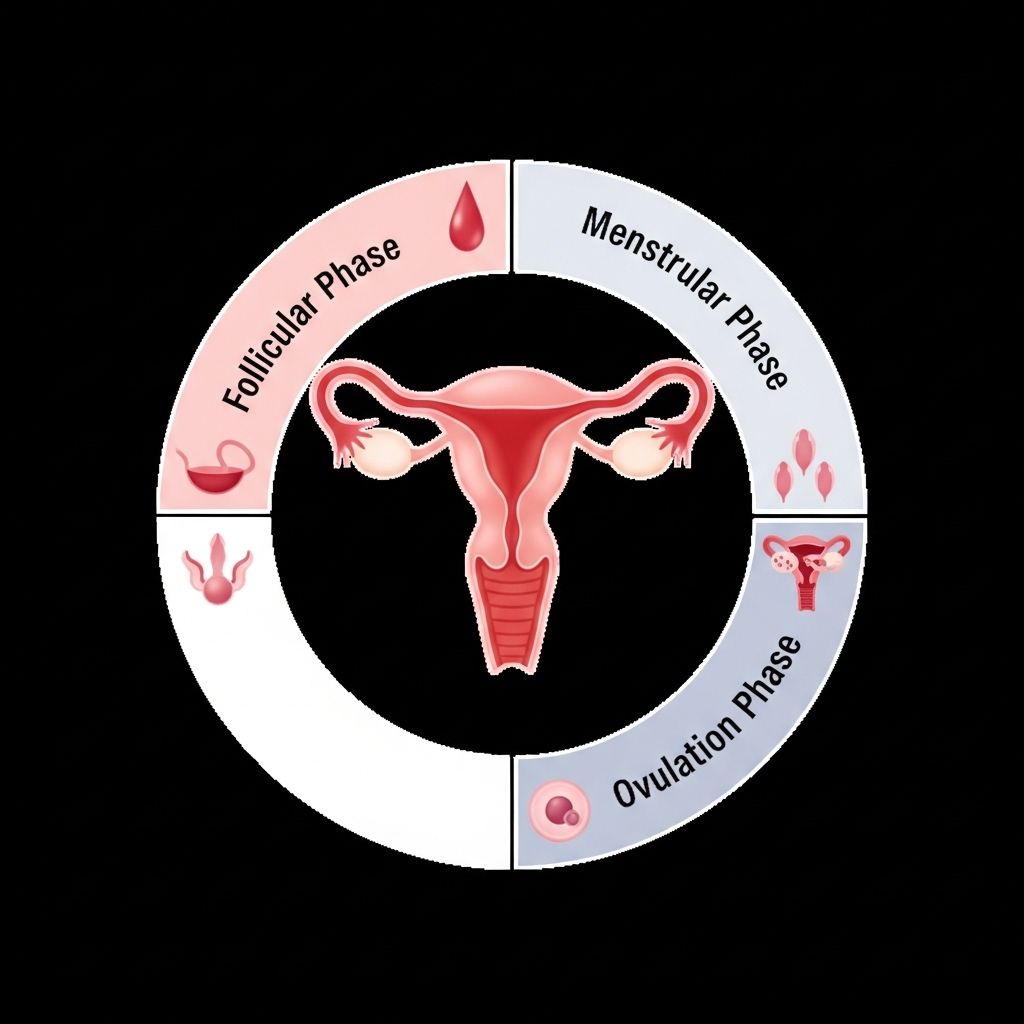
The Four Phases of the Menstrual Cycle
The cycle is divided into four phases:
- Menstruation (Period)
- Follicular Phase
- Ovulation
- Luteal Phase
Each is governed by precise hormonal signaling and bodily changes. Let’s examine each stage in order of occurrence.
1. Menstruation
Duration: 3–7 days
Hormones: Estrogen and progesterone are at their lowest, triggering the shedding of the uterine lining.
- Begins on the first day of bleeding and signals the start of a new cycle.
- Characterized by blood, mucus, and uterine cells leaving the body through the vagina.
- Physical symptoms may include abdominal cramps, bloating, fatigue, breast tenderness, and mood changes.
- Hormones are at their lowest, often leading to lower energy and mood.
This phase’s function is to shed the unfertilized uterine lining and reset the cycle. The drop in progesterone and estrogen leads to the start of menstrual bleeding.
2. Follicular Phase
Duration: 13–16 days (often overlaps with menstruation)
Hormones: FSH rises to stimulate ovarian follicles; estrogen increases, prepping uterine lining.
- Starts on the first day of your period and ends when ovulation begins.
- The pituitary gland releases FSH, which stimulates follicle growth in the ovaries. Each follicle contains an immature egg.
- One follicle becomes dominant and matures, while the rest regress.
- Estrogen levels rise, thickening the endometrial lining and preparing it for potential implantation.
You might feel increasing energy and mood improvement during this phase, as rising estrogen has positive effects on brain chemistry and general well-being. Toward its end, a surge of LH triggers ovulation.
3. Ovulation
Duration: Typically 1 day (the event of egg release)
Hormones: Brief peak of LH and estrogen.
- Occurs about mid-cycle—usually day 14 in a 28-day cycle but varies individually.
- Triggered by an LH surge, a mature egg is released from the dominant follicle in the ovary.
- The egg travels down the fallopian tube, awaiting fertilization.
- This phase is when you are most fertile; unprotected sex around ovulation carries the greatest chance of conception.
- Often accompanied by a slight rise in basal body temperature, thinner cervical mucus, and sometimes mild pelvic discomfort (mittelschmerz).
Signs of ovulation can be monitored via LH urine tests, tracking symptoms, or measuring body temperature.
4. Luteal Phase
Duration: 12–14 days (from ovulation until menstruation begins)
Hormones: Progesterone peaks; estrogen remains moderately high then drops.
- The ruptured follicle becomes the corpus luteum, which secretes high levels of progesterone and some estrogen.
- Progesterone thickens the lining and maintains readiness for possible embryo implantation.
- If fertilization does not occur, the corpus luteum disintegrates, hormone levels decline, and menstruation begins.
- This phase is often associated with PMS symptoms: mood changes, irritability, bloating, breast tenderness, headaches, and cravings.
If fertilization and implantation occur, progesterone and estrogen remain high, supporting early pregnancy. Otherwise, the sharp hormonal decline triggers menstrual bleeding, restarting the entire cycle.
Menstrual Cycle Phases Compared
| Phase | Duration | Main Hormones | Key Events | Typical Symptoms |
|---|---|---|---|---|
| Menstruation | 3–7 days | ↓ Estrogen, ↓ Progesterone | Shedding uterine lining | Cramps, fatigue, mood changes |
| Follicular Phase | 13–16 days | ↑ FSH, ↑ Estrogen | Follicle growth, lining thickens | Rising energy, improved mood |
| Ovulation | ~1 day | LH surge, Estrogen peak | Egg release | Mild pelvic pain, temperature rise |
| Luteal Phase | 12–14 days | ↑ Progesterone | Corpus luteum forms, lining maintained | PMS symptoms, breast tenderness |
Common Symptoms and Experiences Throughout the Cycle
- Menstrual cramps: Caused by uterine contractions during menstruation.
- Bloating & breast tenderness: Often peak in the luteal phase.
- Mood changes: Low mood during menstruation; increased agitation or depression premenstrually.
- Changes in energy: Lowest during menstruation, improves through follicular and peaks at ovulation.
- Fertility: Fertile window usually spans the few days before and the day of ovulation.
- Discharge & cervical mucus: Thin, slippery, and clear at ovulation; sticky and scant during luteal phase.
What Affects the Menstrual Cycle?
The menstrual cycle is sensitive to lifestyle and medical factors, which can lead to irregularities:
- Stress: Can delay or shorten cycles by affecting hormonal signaling.
- Diet and nutrition: Extreme caloric deficits or poor nutrition may stop or lengthen cycles.
- Exercise: Intense physical activity can lower estrogen levels, sometimes stopping menstruation.
- Medications: Hormonal birth control, certain psychiatric or thyroid medications can alter cycle length and symptoms.
- Medical conditions: PCOS, thyroid disorders, or hyperprolactinemia can cause irregular cycles.
- Adolescence & menopause: Cycles are typically irregular at the beginning and near the end of reproductive years.
How to Track Your Menstrual Cycle
- Use a calendar or digital app to note the start and end dates of each period.
- Record symptoms, flow levels, and mood changes.
- For contraceptive or conception purposes, add signs such as basal body temperature, cervical mucus changes, and ovulation predictor kits.
Recording patterns over several months helps identify irregularities, predict fertile windows, and provide crucial health data for medical consultations.
Frequently Asked Questions About Menstrual Cycle Phases
Q: Can menstrual cycles be shorter or longer than 28 days?
A: Yes, a healthy cycle can range from 21 to 35 days. Adolescents often have longer cycles, while adults may have cycles as short as 21 days.
Q: How do hormonal birth control methods affect menstrual phases?
A: Hormonal contraceptives suppress ovulation, alter the growth of the uterine lining, and often eliminate the luteal phase, which can result in lighter or absent periods.
Q: When is the best time to get pregnant?
A: The days leading up to and including ovulation are the most fertile. This is usually around mid-cycle, but exact timing varies by the individual.
Q: What causes premenstrual syndrome (PMS)?
A: PMS stems from hormonal fluctuations in the luteal phase, especially declining progesterone and estrogen before menstruation.
Q: What should I do if my cycles become very irregular?
A: Track your cycle for a few months and speak with a healthcare provider. Cycle irregularities can be caused by stress, medical conditions, or hormonal imbalances, and professional assessment is recommended.
Key Takeaways
- The menstrual cycle has four primary phases: menstruation, follicular phase, ovulation, and luteal phase.
- Hormonal changes orchestrate physiological and emotional shifts throughout the month.
- Understanding these phases is vital for managing reproductive health, identifying fertility windows, and recognizing abnormal symptoms.
- Awareness of lifestyle and health factors affecting the cycle empowers proactive health choices.
For further questions or individualized concerns, consult your healthcare provider. Tracking your cycle provides valuable information about your overall health and can facilitate more effective medical care and decision-making.
References
- https://www.naturalcycles.com/cyclematters/what-is-the-menstrual-cycle
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/menstrual-cycle
- https://my.clevelandclinic.org/health/articles/24417-luteal-phase
- https://www.goodhousekeeping.com/health/a44289160/menstrual-cycle-phases/
- https://www.goodhousekeeping.com/health/fitness/a46585709/cycle-syncing-workouts/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7575238/
- https://www.cdc.gov/hygiene/about/menstrual-hygiene.html
- https://flo.health/menstrual-cycle/health/emotions/menstrual-cycle-phases-and-moods
Read full bio of Sneha Tete












