Efficacy of Ultrasound-Guided Fascial Hydrodissection in Pain Management and Functional Restoration
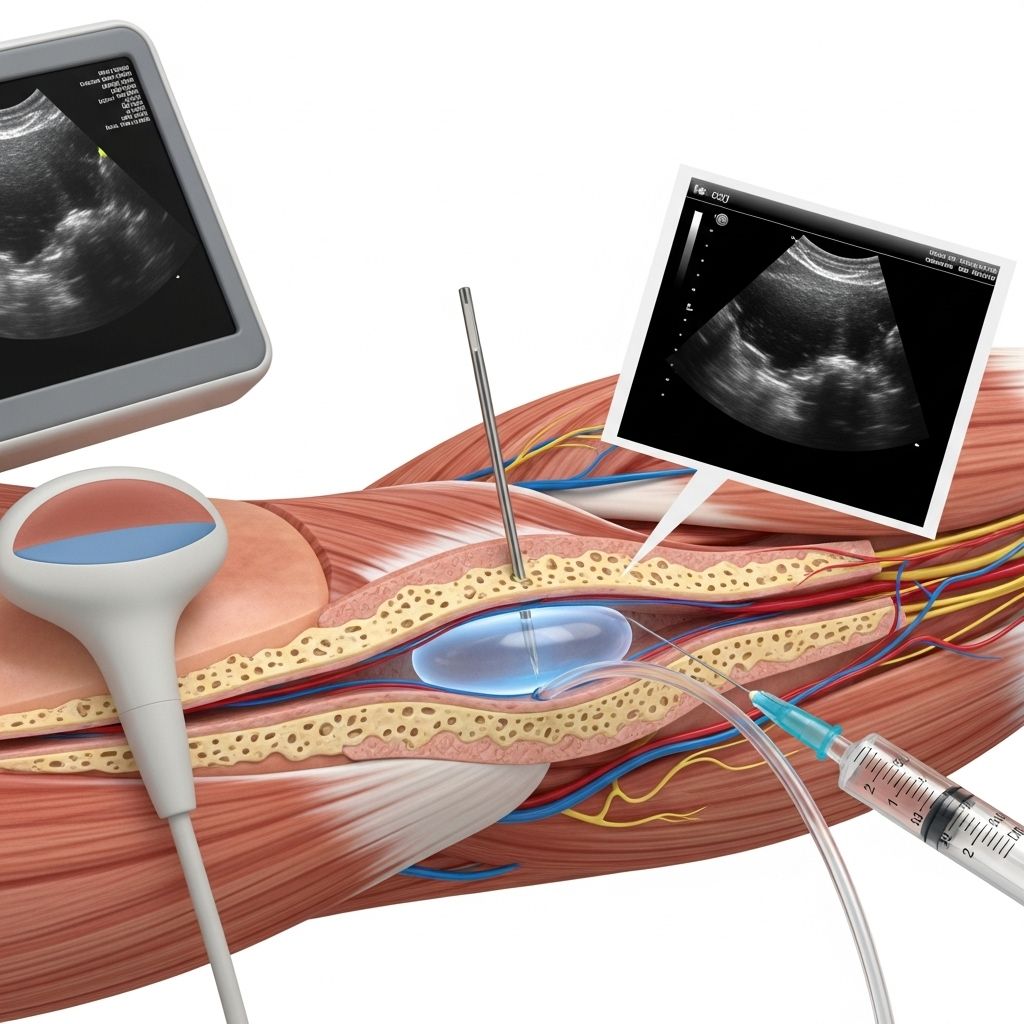
This precise technique separates tissue layers to ease discomfort and restore movement.
Ultrasound-guided fascial hydrodissection (US-FHD) is an innovative technique rapidly gaining ground in interventional pain management, sports medicine, and physical rehabilitation. Its minimally invasive, image-guided approach holds promise for a wide range of patients suffering from chronic pain, nerve entrapment, and fascial adhesions. This article systematically explores the clinical efficacy, supporting evidence, mechanisms of action, and practical considerations for US-FHD—bridging current research with frontline practice.
Table of Contents
- Introduction
- Understanding Fascial Hydrodissection
- Mechanisms of Action
- Clinical Indications and Applications
- Procedure Overview
- Clinical Evidence and Efficacy
- Safety, Complications, and Contraindications
- Patient Outcomes and Case Studies
- Comparisons to Other Approaches
- Frequently Asked Questions
- Conclusion and Future Directions
Introduction
Chronic musculoskeletal pain and nerve entrapment syndromes affect millions worldwide, often leading to diminished quality of life and functional impairment. Traditional treatments—including physical therapy, medications, and surgery—are not always effective or may carry notable risks. Ultrasound-guided fascial hydrodissection offers an evolving, minimally invasive therapeutic alternative, capable of precisely targeting affected tissues without the trauma of open surgery. But how robust is the evidence for its effectiveness? This review delves into the science and clinical results.
Understanding Fascial Hydrodissection
Fascia is a pliable, connective tissue network enveloping muscles, nerves, and organs, playing critical roles in structural support, force transmission, and movement. When fascial layers become adherent, thickened, or scarred—often due to injury, surgery, or chronic inflammation—they can entrap nerves and restrict movement, leading to pain and neurological symptoms.
Fascial hydrodissection refers to the injection of fluid at strategic anatomical planes—most notably between fascial layers or around nerves—under real-time ultrasound visualization. The primary goals are:
- Freeing nerves from adhesions or compressive scar tissue
- Restoring normal tissue gliding between fascial planes
- Reducing pain and restoring function by decompressing soft tissue and neural structures
This method can target peripheral nerves, muscle-tendon interfaces, or large fascial planes, effectively treating a diverse range of pain syndromes and functional limitations.
Mechanisms of Action
The primary therapeutic mechanism in US-FHD is mechanical separation of adhered or compressed structures by hydrostatic fluid injection. The injected solution—often saline, local anesthetic, or regenerative substances such as dextrose or platelet-rich plasma—gently cleaves tissue planes as visualized via ultrasound. Key mechanisms include:
- Physical liberation of fascial adhesions: The fluid dissects and separates entangled tissue planes, restoring normal mobility.
- Nerve decompression: Entrapped or “tethered” nerves are released from scar or fibrosis, easing pain and neuropathic symptoms.
- Hydration and modulation: The injection provides local hydration, which may decrease tension and sensitivity in dense or overused fascial layers.
- Anti-inflammatory effects: Addition of local anesthetics, corticosteroids, or regenerative injectates may further reduce local inflammation, promote healing, and support long-term outcomes.
This minimally traumatic technique contrasts with surgical dissection, which can provoke repeat scarring and additional soft tissue damage.
Clinical Indications and Applications
US-FHD is utilized across a spectrum of clinical scenarios. Its indications span:
- Nerve entrapments: Carpal tunnel syndrome (median nerve), cubital tunnel (ulnar nerve), tarsal tunnel, thoracic outlet, and dorsal scapular or cluneal nerve syndromes
- Chronic fascial pain: Myofascial pain syndromes, thoracolumbar fascia, piriformis syndrome, and stubborn lower back pain
- Post-surgical scar tissue: Scar-related nerve entrapment or fascial restrictions following orthopedic or general surgery
- Tendinopathies and musculoskeletal injuries: Stenosing tenosynovitis, peroneal or ankle tendon entrapment, and others
It is also used for hydrorelease of muscle-bound adhesions, improved mobility in post-traumatic cases, and as a supplementary intervention in multi-modal pain management protocols.
Frequently Treated Regions
- Dorsal scapular nerve (upper back/shoulder blade pain)
- Cluneal nerve (lower back pain)
- Median nerve (carpal tunnel syndrome)
- Ulnar nerve (cubital tunnel syndrome)
- Superficial or sural nerve (ankle, foot pain)
These regions frequently respond favorably to US-FHD, especially when conventional therapies fail or are contraindicated.
Procedure Overview
The ultrasound-guided fascial hydrodissection procedure is characterized by several critical steps and technical nuances:
- Real-time ultrasound visualization: Ensures precise localization of fascial planes, nerves, and injection trajectory, reducing risk to adjacent structures.
- Slow needle advancement: The needle is advanced incrementally, guided by ultrasound, with constant visualization to avoid vascular or neural injury.
- Continuous fluid injection: A steady stream of fluid is injected during advancement to gently separate tissue and ease needle progression.
- Patient feedback: Patients are encouraged to report sensations during the process—such as numbness, aching, or “release”—which are common during fascial decompression.
Injectate Solutions
- Isotonic saline (most common)
- Local anesthetics
- Dextrose (5-10%) for neuro-modulation
- Corticosteroids (for severe inflammation)
- Platelet-rich plasma (PRP) or growth factors (regenerative aims)
The exact composition and volume depends on indication, extent of adhesion, and provider expertise.
Clinical Evidence and Efficacy
Published clinical studies, case reports, and observational trials increasingly support the efficacy of US-FHD for chronic pain, nerve entrapment, and restoring function. The main findings include:
- High success rates: Studies report up to 90% success in symptom improvement for specific nerve entrapments such as carpal tunnel and dorsal scapular syndrome.
- Improved range of motion and pain relief: Many patients experience immediate or rapid reduction in pain, increased movement, and decreased paresthesias following hydrodissection, with sustained results after one or several sessions.
- Reduced need for surgery: For many, US-FHD offers a viable alternative to open surgical release, avoiding the risks and protracted recovery of surgery, especially in recurrent or revision cases.
- Minimally invasive, outpatient procedure: Typically performed in an office or outpatient setting with little to no downtime.
Case Study Excerpt
A patient with chronic lower back pain and loss of range of motion after lumbar surgery underwent thoracolumbar fascial hydrodissection under ultrasound guidance. Post-procedure, the patient reported instant pain relief and increased flexibility. The improvement persisted over subsequent follow-ups, highlighting the technique’s potential for lasting benefit in post-surgical cases.
Clinical Outcomes Table
| Indication | Target Region | Reported Success Rate | Key Outcomes |
|---|---|---|---|
| Carpal Tunnel | Median Nerve | 80-90% | Pain relief, improved grip, sensory restoration |
| Thoracolumbar Pain | Thoracolumbar Fascia | ~90% | Immediate reduction in pain, greater ROM |
| Cubital Tunnel | Ulnar Nerve | Up to 85% | Decreased tingling, ulnar hand symptoms |
Safety, Complications, and Contraindications
When performed by a trained clinician under continuous ultrasound guidance, US-FHD is considered highly safe with low complication rates. Potential risks include:
- Bleeding or vascular injury
- Transient nerve irritation (rarely permanent)
- Infection at injection site
- Allergic or adverse reaction to injectate
Absolute contraindications are active local infection, allergy to injectate components, and uncorrected coagulopathy. Caution is recommended in patients with severe anatomical distortion or poorly visualized target tissue on ultrasound.
Patient Outcomes and Case Studies
Numerous clinic-based reports and structured studies describe positive outcomes with US-FHD. Key highlights include:
- Immediate symptom relief and “release” sensation upon fascial separation
- Restoration of joint or nerve mobility
- Reduced reliance on pain medications
- Significant improvements in functional scores and quality of life in persistent pain syndromes
Many patients who failed conservative therapy or sought to avoid repeat surgeries have regained prior levels of activity—sometimes even after a single session. Multiple sessions may be required for larger or more fibrotic regions.
Comparisons to Other Approaches
| Method | Invasiveness | Guidance | Recovery | Scarring Risk | Repeatability |
|---|---|---|---|---|---|
| US-Guided Hydrodissection | Minimally invasive | Ultrasound | Immediate/minimal | None | High |
| Open Surgical Release | Invasive | Direct visualization | Weeks to months | Moderate to high | Limited |
| Physical Therapy/Needling | Non-invasive | Anatomic landmarks | Gradual | None | Unlimited |
US-FHD stands out for its balance between efficacy, safety, and opportunity for repeated application without cumulative tissue trauma.
Frequently Asked Questions
What is the difference between nerve hydrodissection and fascial hydrodissection?
Nerve hydrodissection focuses on releasing nerves entrapped within scarred or adhered tissue, whereas fascial hydrodissection targets separation of fascial planes irrespective of nerve involvement. Both can be performed in combination, and both employ similar ultrasound-guided injection strategies.
How soon are results noticed after the procedure?
Patients often report significant pain relief and improved motion immediately after treatment. Some may require several sessions for maximum and durable benefit, especially for large or complex fascial adhesions.
How safe is the procedure?
When performed by experienced clinicians with ultrasound guidance, US-FHD is low-risk. Most complications are minor and transient. Serious adverse events are rare.
What types of pain respond best to US-guided fascial hydrodissection?
Chronic neuropathic pain due to nerve entrapment, myofascial pain syndromes, and post-surgical scar-related discomfort are the most responsive, especially when conventional treatments fail.
Is the procedure covered by insurance?
Coverage varies depending on indication, region, and insurer. It is increasingly recognized for nerve entrapment and chronic pain conditions unresponsive to standard care.
Conclusion and Future Directions
Ultrasound-guided fascial hydrodissection is establishing itself as a highly effective intervention for chronic pain and nerve/mechanical entrapment syndromes. Supported by growing clinical evidence, it offers instant and long-term relief for many patients previously limited by other therapies. Its minimally invasive, safe, and repeatable nature, paired with the versatility of ultrasound guidance, makes it a compelling option for care providers. Ongoing studies are expected to further delineate patient selection, comparative effectiveness, and long-term outcomes—heralding a promising future for precision-guided fascial interventions.
References
- https://www.orthopedicscolorado.com/post/nerve-hydrodissection-setting-the-captives-free
- https://proback.com/our-technologies/fascial-hydrodissection-or-hydrorelease/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7414936/
- https://www.youtube.com/watch?v=-DzPhvO3kqA
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10750391/
- https://onlinelibrary.wiley.com/doi/full/10.1002/jcu.23947
- https://www.nature.com/articles/s41598-025-19107-2
Read full bio of Sneha Tete












