Safe Management of Minor Ailments in Patients with a C. Difficile History: Essential Guidelines
Customized treatment plans minimize relapse risk while supporting healthy gut flora.
Clostridioides difficile infection (CDI) poses unique challenges in the management of seemingly minor ailments due to risks of recurrence, complications with standard treatments, and the pivotal role of gut microbiota in patient recovery and long-term health. For healthcare professionals and patients, understanding meticulous protocols and maintaining vigilance are necessary for the safe resolution of everyday health concerns in this special population.
Table of Contents
- Understanding C. Difficile History and Implications
- Risk Assessment Prior to Treatment
- Common Minor Ailments and Tailored Management
- Medication Use: Special Precautions
- Antibiotic Stewardship in Minor Illness
- Role of Probiotics & Microbiome Restoration
- Preventing Recurrence: Patient and Provider Strategies
- Patient Education and Follow-Up
- Frequently Asked Questions (FAQs)
- References
Understanding C. Difficile History and Implications
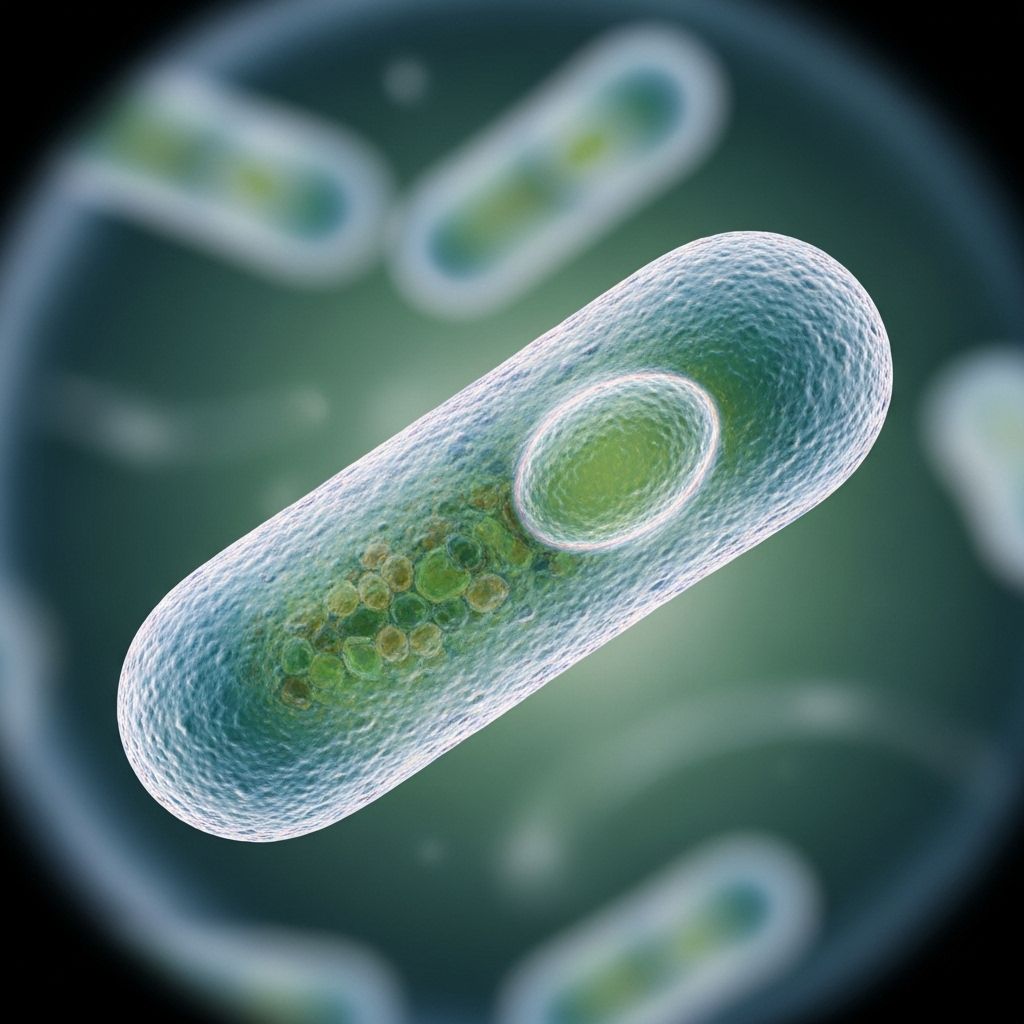
Clostridioides difficile (formerly Clostridium difficile) is a spore-forming bacterium that can cause intestinal infections, primarily marked by diarrhea and potentially severe colitis. Patients with a history of CDI face unique challenges because the disrupted gut microbiota increases their vulnerability to recurrent disease, particularly when exposed to antibiotics, acid-suppressive agents, or other factors that alter gastrointestinal flora.
- CDI is most commonly triggered by recent antibiotic use, but may also occur with immune suppression or advanced age.
Recurrence rates are high, with 20–30% of patients experiencing a second episode and higher risk with each subsequent recurrence. - Even after clinical recovery, patients may experience prolonged periods of disrupted gut flora, increasing susceptibility to reinfection.
- The approach to any new medical issue—no matter how minor—must incorporate safeguards against CDI relapse.
Risk Assessment Prior to Treatment
Before recommending or administering treatment for minor ailments (such as coughs, colds, minor injuries, or skin conditions), it is essential to:
- Review the patient’s full history of CDI episodes, recurrences, and treatments used.
- Determine current gut health, recent antibiotic exposures, and any ongoing immunosuppressive therapy.
- Assess other risk factors: age, underlying gastrointestinal disease (e.g., IBD), and recent hospitalizations.
- Consult with infectious disease specialists for immunocompromised patients or those with complex histories.
Key Considerations for Risk Assessment
- Even mild ailments may escalate if inappropriate medications are used due to disrupted gut flora resilience.
- Minimize hospital exposure—treat as much as safely possible in outpatient or home settings.
Common Minor Ailments and Tailored Management
Many minor ailments may be managed with little or no pharmacological intervention in patients with a CDI history, avoiding unnecessary risks. When medical management is necessary, the choice of therapy must reflect CDI risk.
| Ailment | Considerations and Preferred Management |
|---|---|
| Upper Respiratory Tract Infections (colds, pharyngitis) |
|
| Skin Infections (minor wounds, mild cellulitis) |
|
| Urinary Tract Infections |
|
| Pain and Fever (headache, musculoskeletal pain, minor injury) |
|
| Gastrointestinal Disturbances (nausea, functional bowel symptoms) |
|
| Allergic Reactions (mild urticaria, hay fever) |
|
Medication Use: Special Precautions
Certain medications may precipitate CDI recurrence or worsen gut flora disruption. Key strategies include:
- Avoid broad-spectrum antibiotics when treating minor bacterial infections, opting for narrow-spectrum agents with the lowest CDI risk possible.
- Avoid high-risk antibiotics, notably clindamycin, cephalosporins, and fluoroquinolones, unless no alternative exists.
- Minimize or avoid acid-suppressive medications such as proton pump inhibitors (PPIs) unless essential, as they increase CDI risk.
- Use antimotility agents with extreme caution during any gastrointestinal complaints to avoid exacerbation or masking of CDI symptoms.
Antibiotic Stewardship in Minor Illness
Antibiotic stewardship is paramount in the care of patients with a previous CDI. Best practices include:
- Reserving antibiotics for clear, evidence-based indications only.
- Choosing the narrowest spectrum and shortest effective course.
- Discussing alternatives to antibiotics for self-limited illnesses with patients, emphasizing non-pharmacological therapies when appropriate.
- Documenting the discussion, indication, chosen drug, and duration in the patient’s record for transparency and monitoring.
Table: Common Antibiotics and CDI Risk
| Antibiotic | Relative CDI Risk |
|---|---|
| Clindamycin | High |
| Fluoroquinolones | High |
| Cephalosporins | Moderate to High |
| Broad-spectrum Penicillins | Moderate |
| Macrolides | Moderate |
| Tetracyclines | Low |
| Nitrofurantoin, Fosfomycin | Low |
Role of Probiotics & Microbiome Restoration
Rebuilding the gut microbiome after CDI is crucial for decreasing future infection risk.
- Evidence on routine probiotic use is mixed, but certain strains (e.g., Saccharomyces boulardii) may reduce recurrence, especially when antibiotics cannot be avoided. Discuss risks and benefits with patients as probiotics can be contraindicated in immunocompromised individuals.
- A diet rich in fiber, prebiotics, and fermented foods supports the restoration of healthy gut flora post-CDI.
- For recurrent CDI not responding to standard therapy, fecal microbiota transplantation (FMT) may be considered under specialist guidance.
Preventing Recurrence: Patient and Provider Strategies
Because the risk of CDI recurrence is substantial, multifaceted prevention strategies are imperative:
- Rigorous hand hygiene for all healthcare workers and patients, using soap and water (alcohol-based gels are less effective against spores).
- Environmental cleaning with sporicidal agents in households and clinical areas where CDI was previously present.
- Avoid unnecessary changes in diet or medications that can affect gut flora (such as abrupt introduction of new laxatives or acid suppressors).
- Early recognition of CDI symptoms: persistent diarrhea (≥3 unformed stools in 24 hours), fever, abdominal cramping, or unexplained leukocytosis should prompt testing and urgent medical evaluation.
Provider Checklist: Preventing CDI Recurrences
- Flag CDI history in the patient’s medical record for easy identification at all care points.
- Alert pharmacy and all treating clinicians of CDI history before prescribing or dispensing antibiotics.
- Educate patients on recognizing early symptoms of recurrence and instruct them to report new GI symptoms promptly.
- Schedule close follow-up (telehealth or in-person) after prescribing antibiotics for any indication.
Patient Education and Follow-Up
Empowering patients plays a large role in sustaining remission and early recognition of complications. Key educational points include:
- Explain the link between antibiotic use and recurrence, and reinforce why some treatments may be withheld or substituted.
- Highlight self-care approaches for common minor ailments (hydration, rest, symptomatic relief).
- Discuss safe use of over-the-counter medications. Patients should avoid starting new medications, especially antibiotics or acid suppressors, without consulting their provider.
- Advise immediate medical attention if symptoms suggestive of CDI (persistent or bloody diarrhea, high fever, severe abdominal pain) recur.
Advice for Home Management
- Maintain a healthy, balanced diet with adequate fiber.
- Monitor for early signs of infection relapse—do not delay reporting symptoms.
- Keep a list of previous episodes and treatments to share with any new healthcare providers.
Frequently Asked Questions (FAQs)
Q: Can I take antibiotics for minor infections if I have a history of C. difficile?
A: Antibiotics should be prescribed only when absolutely necessary, and your clinician should choose the safest, narrow-spectrum option available. Always inform every healthcare provider of your CDI history so appropriate precautions are taken.
Q: Are probiotics safe and effective after a C. difficile infection?
A: Some probiotics may reduce recurrence risk, but they are not universally recommended for all patients. They may not be safe for individuals who are immunocompromised. Discuss probiotic use with your clinician before starting any supplement.
Q: What over-the-counter medications are safe for pain or fever?
A: Acetaminophen is generally preferred. NSAIDs should be used with caution due to gastrointestinal risks, especially in patients with a CDI history.
Q: What should I do if I experience diarrhea again?
A: If you develop three or more loose stools in 24 hours, especially with pain or fever, contact your healthcare provider immediately for evaluation and possible testing for C. difficile recurrence.
Q: Is there a role for dietary supplements or special diets to prevent C. difficile recurrence?
A: A balanced diet with diverse fiber sources and possibly fermented foods may help restore healthy gut microbiota. Evidence for specific supplements is mixed—consult your healthcare provider before making major dietary changes.
References
- Clostridioides difficile infection – Wikipedia
- AAFP – Clostridioides difficile Infection: Update on Management
- Clostridium difficile: The evolving story – PMC
References
- https://en.wikipedia.org/wiki/Clostridioides_difficile_infection
- https://www.aafp.org/pubs/afp/issues/2020/0201/p168.html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2533571/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11324037/
- https://academic.oup.com/cid/article/46/Supplement_1/S4/456218
- https://www.cdc.gov/c-diff/hcp/clinical-overview/index.html
- https://publications.aap.org/pediatrics/article/152/3/e2023062307/193288/Clostridioides-difficile-Infection-in-Children
Read full bio of Sneha Tete












