The Link Between Thyroid Dysfunction and Impaired Barrier Function: Exploring the Gut-Thyroid Axis and Systemic Impacts
Imbalanced hormones disrupt gut and skin defenses by altering microbiota, immune balance.
The Link Between Thyroid Dysfunction and Impaired Barrier Function
Increasing research demonstrates a dynamic and reciprocal connection between thyroid dysfunction and impaired barrier function in the body. This complex relationship involves multifactorial interactions among endocrinology, immunology, gut microbiota, and epithelial physiology. It has significant implications for the development and management of autoimmune thyroid diseases, chronic hypothyroidism, and related systemic disorders. In this article, we delve into how thyroid dysfunction and compromised barrier function are interlinked, emphasizing the gut-thyroid axis, immune modulation, and practical considerations for diagnostics and therapeutics.
Table of Contents
- Introduction to Thyroid Dysfunction and Barrier Function
- Thyroid Gland Functions and Disorders
- What is Barrier Function and Why Is It Important?
- Thyroid Dysfunction and the Epithelial Barrier
- The Gut-Thyroid Axis: Microbiota and Immune Interaction
- Autoimmune Thyroid Disease and Barrier Impairment
- Brain Barrier Function and Thyroid Hormones
- Dermatologic Manifestations
- Diagnosis and Biomarkers
- Therapeutic Approaches and Future Directions
- Frequently Asked Questions (FAQs)
Introduction to Thyroid Dysfunction and Barrier Function
The thyroid gland is integral to metabolic and hormonal balance, affecting nearly every tissue in the human body. Dysfunction in this gland—manifesting as hypothyroidism or hyperthyroidism—not only disrupts metabolic processes but also has a bidirectional relationship with barrier functions, such as epithelial integrity in the gut, skin, and even the blood-brain barrier. Impaired barrier function is implicated in increased vulnerability to autoimmune responses, chronic inflammation, and altered nutrient absorption, which in turn affects thyroid activity itself.
Thyroid Gland Functions and Disorders
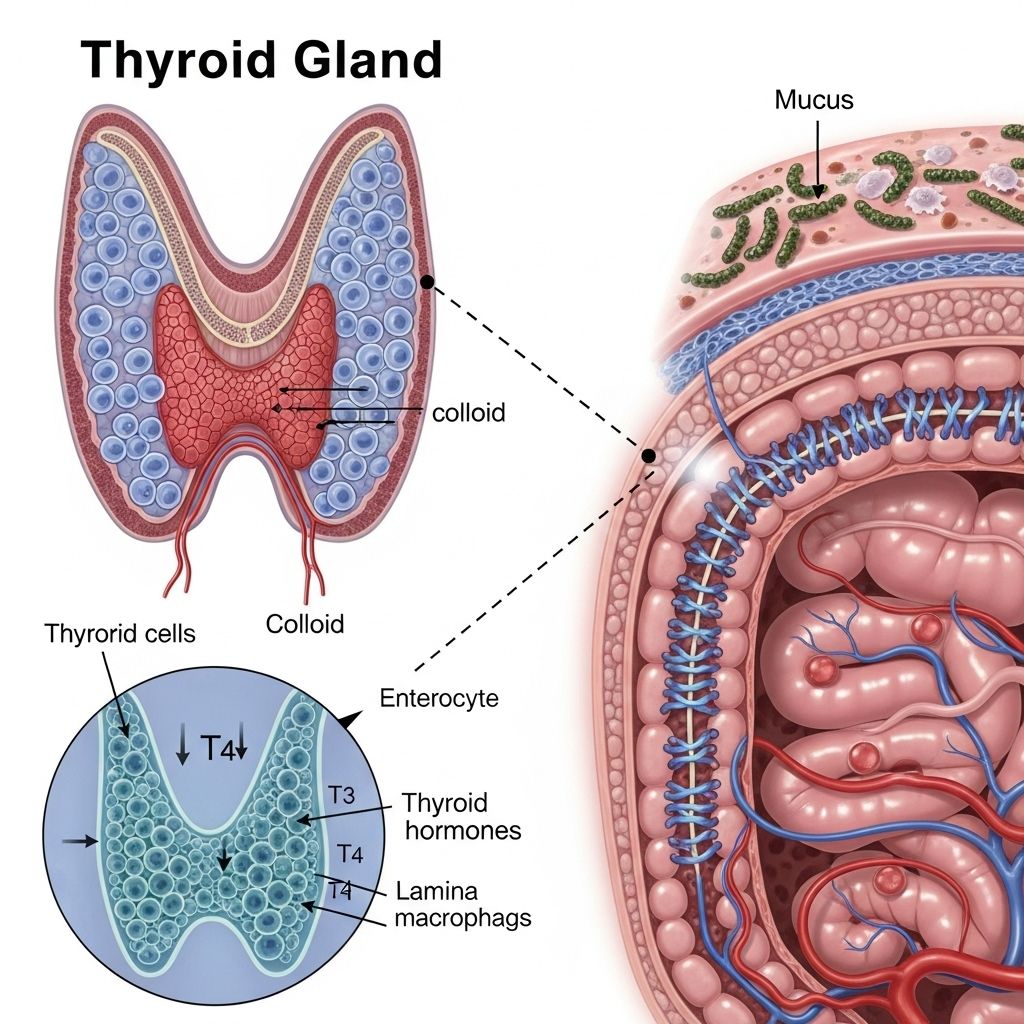
The thyroid gland, located in the neck, produces hormones—primarily thyroxine (T4) and triiodothyronine (T3)—that regulate metabolism, growth, and development. Common thyroid disorders include:
- Hypothyroidism: Reduced hormone production, leading to fatigue, weight gain, and slowed bodily functions.
- Hyperthyroidism: Excess hormone production, inducing anxiety, weight loss, and increased metabolic rate.
- Autoimmune Thyroid Diseases (AITD): Includes Hashimoto’s thyroiditis (leading to hypothyroidism) and Graves’ disease (associated with hyperthyroidism).
These conditions are often accompanied by changes in barrier function and tissue homeostasis, especially within the gut and skin.
What is Barrier Function and Why Is It Important?
Barrier function refers to the structural and physiological defenses that separate internal organs and tissues from the external environment and from potentially harmful substances within the body. Major barriers include:
- The intestinal epithelial barrier: Controls absorption, blocks pathogens, and regulates immune activity.
- The skin barrier: Protects against dehydration, pathogens, and environmental insults.
- The blood-brain barrier: Shields neural tissue from toxins and inflammatory molecules.
Impaired barrier function is associated with increased permeability (leaky gut), immune dysregulation, and vulnerability to infection and autoimmunity.
Thyroid Dysfunction and the Epithelial Barrier
Thyroid hormones are crucial for the differentiation, maturation, and repair of epithelial tissues, including the skin and gut. Hypothyroidism can hinder the formation and maintenance of these barriers, while excess thyroid hormone may accelerate turnover but risk incomplete maturation. Several mechanisms highlight this relationship:
- Gut Motility: Reduced in hypothyroidism, leading to altered microbiota and increased intestinal permeability.
- Nutrient Absorption: Thyroid hormones regulate the expression of key transporters for micronutrients such as iodine and selenium, both essential for immune and epithelial function.
- Epidermal Integrity: Deficiency impairs barrier formation, increases skin dryness, susceptibility to infection, and delayed healing.
Clinical studies confirm that patients with thyroid dysfunction display barrier impairment symptoms systemically, with especially pronounced alterations in the gut and skin.
The Gut-Thyroid Axis: Microbiota and Immune Interaction
The gut-thyroid axis is a central hub where endocrine and immune factors intersect. The gut microbiota shapes immune responses, modulates epithelial permeability, and directly influences thyroid function. Key aspects include:
- Microbiota composition shifts: Hypothyroidism and AITD patients often have fewer beneficial bacteria (such as Bifidobacterium and lactic acid bacteria) and an increase in harmful species (Bacteroides fragilis), compared to healthy controls.
- Immune tolerance: A balanced microbiota supports immune tolerance to tissue antigens, protecting against autoimmunity. Dysbiosis disrupts this balance, promoting chronic inflammation and autoantibody production.
- Micronutrient regulation: The gut flora regulates absorption of iodine and selenium, required for optimal thyroid hormone synthesis and repair of epithelial barriers.
| Protective Microbiota | Risk Microbiota |
|---|---|
| Bifidobacterium, Lachnospiraceae UCG008, Actinobacteria, Verrucomicrobia | Intestinimonas, Eubacterium brachy group, Ruminiclostridium5, Ruminococcaceae UCG004 |
Emerging evidence suggests a bidirectional relationship: not only does hypothyroidism disrupt gut homeostasis, but altered microbiota can impair thyroid function, perpetuating disease cycles.
Effects of Gut Microbiota on Thyroid Function
- Microbial metabolites modulate immune cell signaling, influencing the risk of autoimmunity.
- Gut dysbiosis may elevate thyroid-specific autoantibodies (e.g., TPOAb, TGAb, TRAb).
- Bacterial-induced malabsorption of selenium and iodine impairs thyroid hormone synthesis and immune regulation.
Autoimmune Thyroid Disease and Barrier Impairment
Autoimmune thyroid diseases (AITD), such as Hashimoto’s thyroiditis and Graves’ disease, are frequently accompanied by impaired gut barrier function and intestinal dysbiosis. Pathophysiological mechanisms include:
- Elevated thyroid-specific autoantibodies disrupt epithelial and immune homeostasis.
- Intestinal permeability promotes translocation of microbial and dietary antigens, activating immune responses that target thyroid tissue.
- Shared pro-inflammatory cytokines (e.g., IL-17 from Th17 cells) drive both barrier dysfunction and autoimmune processes.
- Selenium deficiency, due to malabsorption, impairs the antioxidant defense of both thyroid and epithelial cells.
AITD patients show significant changes in microbiota composition compared to healthy individuals, with increased harmful bacteria and a loss of protective strains. These alterations perpetuate a cycle of immune activation and barrier impairment, creating therapeutic challenges and necessitating targeted interventions.
Brain Barrier Function and Thyroid Hormones
Thyroid hormones are vital for brain barrier integrity, especially during fetal and postnatal development. Systemic hypothyroidism or impaired thyroid hormone transporters (e.g., MCT8, OATP1C1) can severely compromise brain barriers, leading to abnormal gene expression, neurodevelopmental delay, and heightened vulnerability to inflammation. Experimental models show:
- Systemic hypothyroidism alters twice the number of brain genes, compared to isolated cerebral hypothyroidism.
- Impaired thyroid hormone signaling affects local and systemic transcriptional profiles, impacting genes involved in barrier maintenance and neuroimmune regulation.
Dermatologic Manifestations
Thyroid hormones accelerate skin barrier formation, and deficiency is associated with impaired epidermal function, dry and fragile skin, and delayed wound healing. Specific manifestations include:
- Hypothyroidism: Increased dryness, rough texture, decreased sweating, susceptibility to infections.
- Hyperthyroidism: Warm, moist skin, increased metabolism but potential for incomplete barrier maturation.
Epidermal barrier repair is compromised in both conditions if hormone balance is not restored.
Diagnosis and Biomarkers
Diagnosis of thyroid dysfunction typically involves serum hormone measurement (TSH, T4, T3) and autoantibody panels (TPOAb, TGAb, TRAb). Emerging diagnostics also assess:
- Gut permeability tests (e.g., lactulose/mannitol ratio) to evaluate barrier function.
- Microbiota profiling: Sequencing techniques identify dysbiosis and guide probiotic selection.
- Selenium and iodine status: Critical for hormone synthesis and barrier repair.
Therapeutic Approaches and Future Directions
Understanding the link between thyroid dysfunction and barrier impairment informs new therapeutic strategies:
- Probiotics and prebiotics: Target specific microbiota to restore gut-thyroid axis homeostasis and improve barrier function.
- Selenium and iodine supplementation: Ensure adequate hormone synthesis and epithelial repair.
- Anti-inflammatory treatments: Modulate pro-inflammatory cytokines to dampen autoimmune processes and support barrier integrity.
- Personalized medicine: GM-based diagnostics inform individual approaches for thyroid and barrier dysfunction management.
Ongoing research seeks to unravel additional mechanistic links and develop targeted interventions for multisystem restoration in thyroid and barrier pathologies.
Frequently Asked Questions (FAQs)
Q: How can thyroid dysfunction lead to impaired intestinal barrier function?
Thyroid dysfunction, particularly hypothyroidism, reduces gut motility and alters immune signaling, resulting in increased intestinal permeability and susceptibility to infections and inflammation.
Q: Can improving gut health reverse thyroid dysfunction?
Emerging evidence suggests that targeted microbiota restoration—through probiotics, prebiotics, and dietary support—can improve thyroid function by restoring the gut-thyroid axis. However, the effect varies by individual and disease state.
Q: What role do micronutrients play in the thyroid-barrier link?
Selenium and iodine are essential for thyroid hormone synthesis and immune modulation. Gut barrier impairment can cause malabsorption of these nutrients, worsening thyroid and epithelial health.
Q: Are skin changes always present in thyroid dysfunction?
Skin manifestations are common but not universal in thyroid disease. Hypothyroidism frequently presents with dry, coarse skin, while hyperthyroidism can accelerate skin turnover.
Q: What are the future prospects for treating linked thyroid and barrier dysfunction?
Innovative approaches include microbiome-targeted therapies, immune modulation, and micronutrient supplementation as part of personalized, multi-disciplinary care. Clinical trials are ongoing to refine these treatments for diverse patient populations.
References
- https://www.dovepress.com/gut-microbiota-changes-and-its-potential-relations-with-thyroid-disord-peer-reviewed-fulltext-article-IJGM
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1267383/full
- https://www.ncbi.nlm.nih.gov/books/NBK285549/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10214500/
- https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1465928/full
- https://myacare.com/blog/exploring-the-gut-microbiome-hypothyroidism-connection
Read full bio of medha deb












