Stress & Skin Circulation: The Cortisol Connection Explained in Depth
Finding calm can minimize flare-ups, strengthen barrier function, and boost resilience.
Stress & Skin Circulation: The Cortisol Connection Explained
Understanding the profound ways psychological stress impacts skin health is essential. Central to this relationship is cortisol, a stress hormone that drives changes in skin circulation, immunity, barrier function, and appearance. This comprehensive guide explains the intricate interplay between stress, cortisol, and your skin, offering insights and practical tips for healthier, more resilient skin.
Table of Contents
- Introduction: The Mind-Skin Connection
- Skin Circulation Basics
- Cortisol and the Body’s Stress Response
- How Stress Affects Skin Circulation
- Cortisol’s Impact on Skin Health
- Stress-Linked Skin Conditions
- Barrier Function and Wound Healing
- Aging Skin: Circulation and Collagen
- Managing Stress for Better Skin
- Frequently Asked Questions
- Conclusion & Takeaways
Introduction: The Mind-Skin Connection
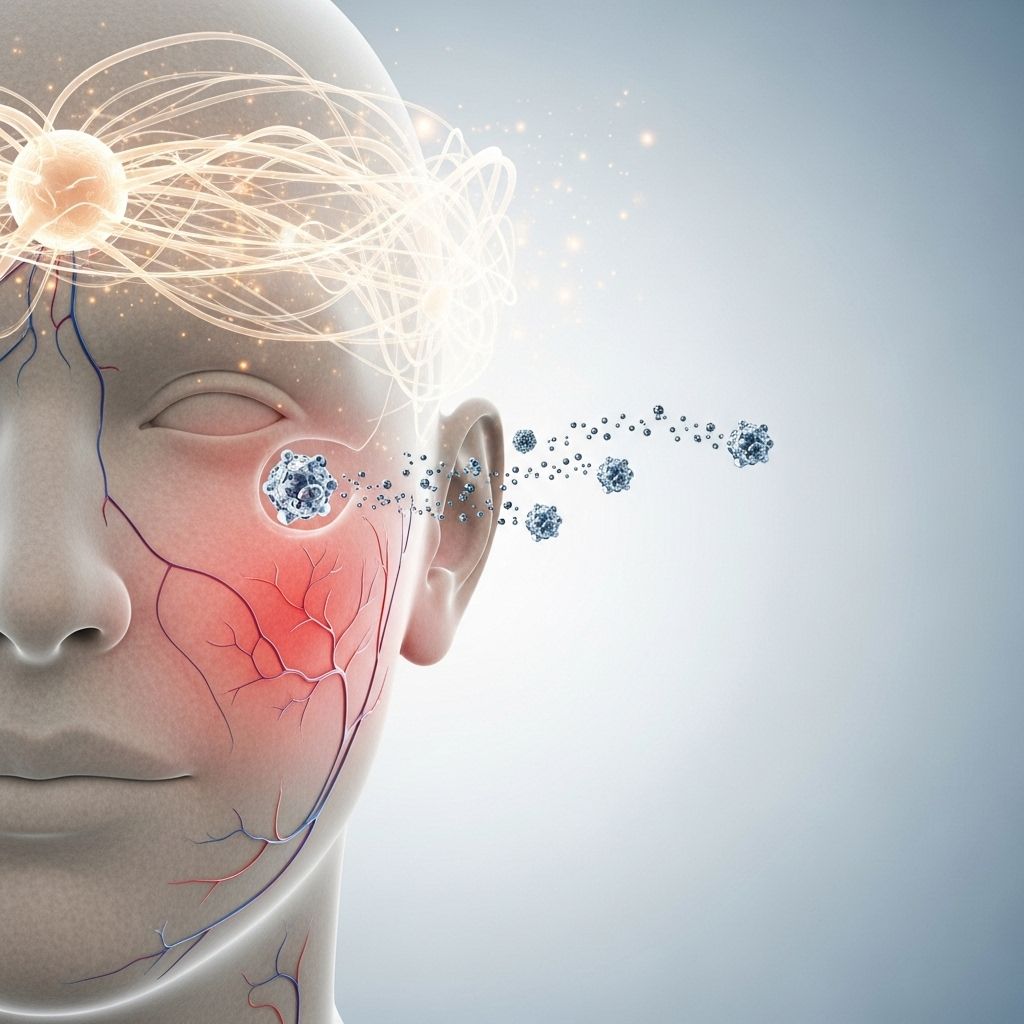
The relationship between the mind, body, and skin is longstanding. Psychological stress doesn’t just affect your mood or energy; it triggers a cascade of reactions that directly alter the health and appearance of your skin. Modern research points to cortisol, the body’s chief stress hormone, as a central mediator in this process, affecting everything from skin circulation to inflammatory responses and barrier function. Understanding this connection is the starting point for making targeted interventions to improve both mental wellbeing and skin health.
Skin Circulation Basics
Skin circulation refers to the flow of blood through the vessels in the skin. This process:
- Delivers oxygen and essential nutrients to skin cells.
- Removes metabolic waste products.
- Regulates skin temperature and color.
- Supports the skin’s barrier function and natural healing processes.
Disruption of skin circulation can manifest as paleness, blotchiness, redness, or impaired healing. Blood flow is tightly regulated by the nervous system, hormones, and local chemical factors. Stress and cortisol play a key role in modulating these processes.
Cortisol and the Body’s Stress Response
Cortisol is produced by the adrenal glands as part of the body’s fight-or-flight response. When a stressful event occurs, the following sequence unfolds:
- Brain signals (via the hypothalamus) trigger release of corticotropin-releasing hormone (CRH).
- CRH stimulates the pituitary gland to secrete ACTH (adrenocorticotropic hormone).
- ACTH prompts the adrenal cortex to release cortisol into the bloodstream.
Cortisol is necessary in small, short bursts—mobilizing energy, raising alertness, and readying tissues to respond to danger. However, chronic psychological stress means cortisol stays high for long periods, disrupting normal physiological functions, especially in the skin.
Peripheral HPA Axis in Skin
Remarkably, the skin possesses its own version of the hypothalamic-pituitary-adrenal (HPA) axis components such as CRH, ACTH, and their receptors. Skin cells can locally produce and respond to stress hormones, meaning stress impacts skin both systemically and locally .
How Stress Affects Skin Circulation
Under stress, your body’s first response is to redirect blood flow towards essential organs (heart, lungs, muscles) in preparation for action. This shift causes subtle but important changes in the skin:
- Reduced blood flow to the skin, leading to paleness or a dull complexion.
- Constriction of skin vessels (vasoconstriction) as blood is shunted away.
- With prolonged stress, skin blood vessels may become dysfunctional, resulting in redness, uneven tone, or flare-ups of conditions like rosacea.
These changes are regulated both by the nervous system (acting almost instantly) and by hormonal shifts, primarily involving cortisol.
Cortisol’s Impact on Skin Health
Cortisol, while crucial in emergency situations, can undermine skin health in several ways when chronically elevated:
1. Increased Sebum and Oil Production
- Stimulates sebaceous glands to produce more sebum (oil), leading to clogged pores and acne .
- Excess oil mixes with dead skin and bacteria, increasing risk of breakouts.
2. Impaired Skin Barrier Function
- Cortisol and other stress hormones disrupt skin’s protective barrier (the stratum corneum), making it easier for irritants and microbes to penetrate .
- Results in dryness, flakiness, and increased sensitivity to environmental triggers.
3. Delayed Wound Healing
- High cortisol inhibits skin cell proliferation and differentiation, slowing repair of damaged tissues .
- Wounds, scrapes, and acne lesions persist longer and scar more easily.
4. Accelerated Breakdown of Collagen & Elastin
- Cortisol speeds up breakdown of collagen and elastin, essential proteins for firm, youthful skin.
- Results in thinning skin, reduced elasticity, and more pronounced wrinkles .
5. Heightened Inflammatory Response
- Cortisol disrupts normal immune balance, sometimes suppressing (which means slower healing) and sometimes provoking inflammation (aggravating existing skin problems).
- Can worsen conditions like eczema, psoriasis, or trigger rashes and hives.
Stress-Linked Skin Conditions
Many common dermatological conditions are aggravated by stress and elevated cortisol, including:
- Acne: Increased oil, clogged pores, and inflammation worsen breakouts, particularly on the face, chest, and back .
- Eczema: Stress weakens the skin barrier and triggers immune dysregulation, flaring up itchy, inflamed patches of eczema .
- Psoriasis: Inflammatory responses heightened by cortisol and local immune factors can provoke or intensify psoriasis flares.
- Rosacea: Vessel instability linked to stress can increase facial redness and visible blood vessels.
- Hives (Urticaria) and Rashes: Stress-induced histamine release causes swollen, red, itchy welts or diffuse rashes .
- Hair Loss: Excess cortisol can move hair follicles into a resting phase, leading to shedding or thinning.
Barrier Function and Wound Healing
The stratum corneum is the outermost layer of the skin, serving as the body’s main barrier against moisture loss and infection. Cortisol disrupts this layer in several ways:
- Reduces production of lipids (such as ceramides) that maintain hydration.
- Impairs protein synthesis necessary for strong cell connections.
- Leads to increased water loss, dryness, and a rough texture .
- Decreases immune function at the skin level, increasing risk of infection and delayed wound healing .
Studies have shown that blocking stress hormone receptors or replenishing lost skin lipids can restore normal barrier function, underscoring cortisol’s pivotal impact.
Aging Skin: Circulation and Collagen
As skin ages, circulation slows and the structure changes. Chronic stress and cortisol speed up these changes by:
- Halting collagen and elastin synthesis, with cortisol actively breaking down existing fibers.
- Reducing skin’s supply of oxygen and nutrients due to impaired circulation.
- Promoting oxidative stress, which leads to cellular damage and visible signs of aging (fine lines, dullness, sagging).
- Exacerbating uneven pigmentation or spots due to disruption of melanocyte activity.
| Short-term (Acute stress) | Long-term (Chronic stress) |
|---|---|
| Temporary increase in alertness Possible brief flushing or paleness | Persistent acne, dull complexion Dryness, sensitive skin, wrinkles |
| Enhanced immune surveillance in skin | Chronic inflammation, flare of eczema/psoriasis |
| No significant impact on collagen | Accelerated collagen breakdown, sagging, visible aging |
| Wound healing not affected | Delayed healing, risk of infection |
Managing Stress for Better Skin
Effective skin care goes beyond creams or cleansers—it must include stress reduction strategies that keep cortisol in check. Consider these evidence-based approaches:
- Mindfulness and meditation: Lowers cortisol and calms inflammation.
- Exercise: Regular movement promotes circulation and helps normalize hormone levels.
- Sleep hygiene: Quality sleep is crucial for skin repair and hormone regulation.
- Anti-inflammatory diet: Omega-3 rich foods, antioxidants, fruits, and vegetables support skin health inside out.
- Skin care routines: Gentle, moisturizing products restore barrier function. Avoid harsh scrubs/detergents that worsen dryness.
- Professional support: Dermatologists can recommend tailored regimens; therapists can support chronic stress management.
Frequently Asked Questions (FAQs)
Q: How does cortisol specifically cause acne?
A: Cortisol increases sebum (oil) production in skin glands, which, combined with stress-related inflammation, clogs pores and creates an environment for acne bacteria to flourish.
Q: Can managing stress alone clear up my skin issues?
A: While stress management significantly helps reduce flare-ups, especially for stress-exacerbated conditions like eczema and acne, other factors (like genetics, diet, and environment) also play a role. Best results come from a holistic approach.
Q: Why does my skin feel itchier when I’m stressed?
A: Stress—via CRH and cortisol—activates immune and inflammatory pathways that increase histamine release and sensitivity in skin nerves, often causing itching or heightened reactivity.
Q: Are certain skin types more affected by stress?
A: Yes. People prone to oily, sensitive, or inflammatory skin conditions (like acne, eczema, or rosacea) typically notice more pronounced effects from stress.
Q: Can topical skin care counteract stress effects?
A: Mild, barrier-repairing creams (containing ceramides, glycerin, or fatty acids) can help repair stress-damaged barriers. However, addressing internal stress and cortisol remains vital for long-term improvement.
Conclusion & Takeaways
Understanding the cortisol connection reveals why managing stress is as important for skin health as any lotion or prescription. Chronic stress triggers a hormonal domino effect that undermines the skin’s barrier, slows healing, alters circulation, accelerates aging, and intensifies existing conditions. Prioritizing holistic well-being—by managing stress, nourishing the body, and using gentle skin care—builds a foundation for radiant, resilient skin at any stage of life.
References
- Dermatology Seattle: How Stress Affects Your Skin
- PubMed Central: Brain-Skin Connection: Stress, Inflammation, and Skin Aging
- Westlake Dermatology: How Stress Is Damaging Your Skin
References
- https://dermatologyseattle.com/how-stress-affects-your-skin-expert-dermatologist-advice-and-solutions/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4082169/
- https://www.westlakedermatology.com/blog/how-stress-is-damaging-your-skin/
- https://www.ucihealth.org/blog/2024/08/cortisol-face
- https://news.cuanschutz.edu/department-of-medicine/cortisol-face
- https://www.health.harvard.edu/blog/stress-may-be-getting-to-your-skin-but-its-not-a-one-way-street-2021041422334
- https://aadermatology.com/healthy-skin-month-stress-affects-skin/
- https://www.ncbi.nlm.nih.gov/books/NBK538239/
- https://health.osu.edu/health/skin-and-body/is-cortisol-face-real
Read full bio of Sneha Tete












