The Impact of Stress on Digestion and the Vagus Nerve: Unraveling the Gut-Brain Connection for Better Health
Calm stress to ease digestion and strengthen the nerve pathways that support gut health.
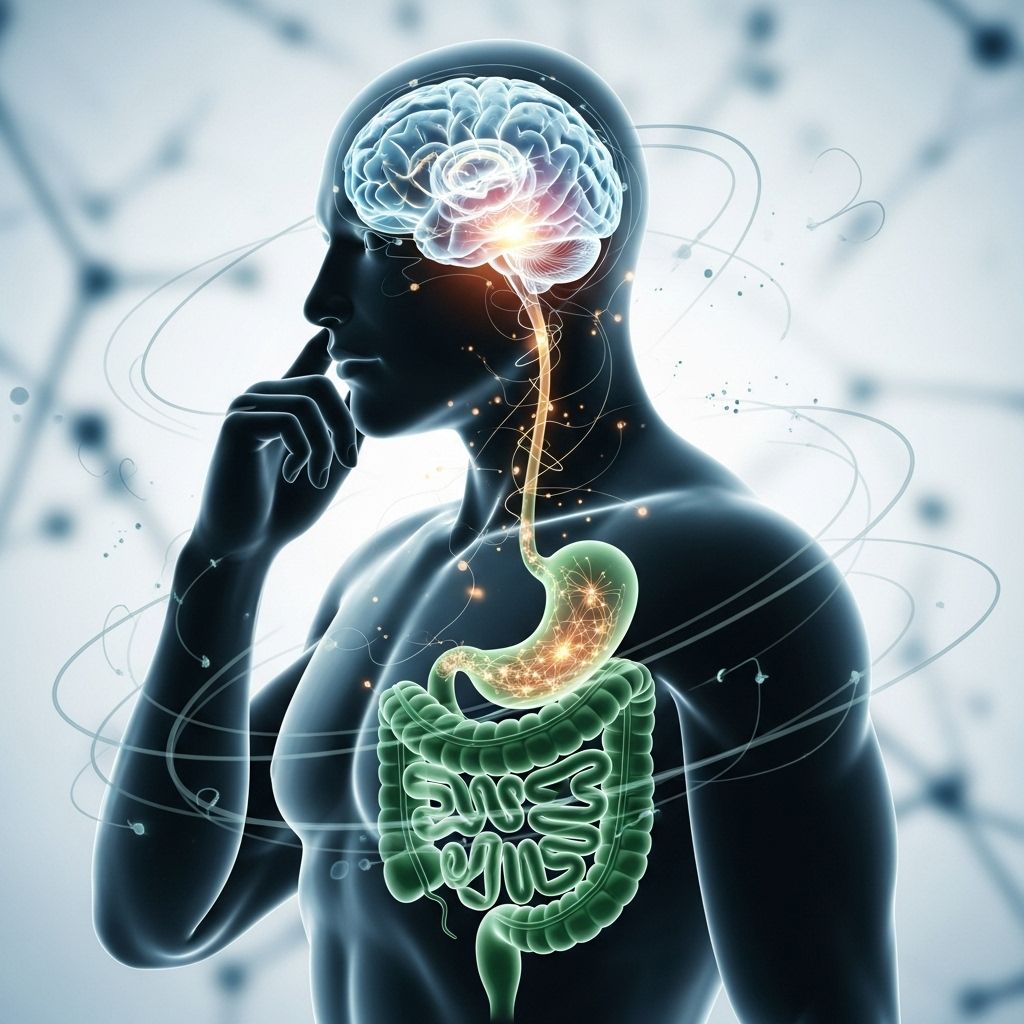
Our digestive system is in constant conversation with our brain, and few things disrupt this dialogue more profoundly than stress. This article dives deep into how psychological stress affects digestive health, the central role of the vagus nerve, and what you can do to support wellbeing at the intersection of mind and gut.
Table of Contents
- Understanding the Gut-Brain Axis
- The Role of the Vagus Nerve in Digestion
- How Stress Impacts Digestion
- Stress-Related Digestive Disorders
- Mechanisms: How Stress Alters Gut Function
- The Vagus Nerve in Stress Response
- Symptoms and Signs
- Supporting Gut Health During Stress
- Frequently Asked Questions (FAQs)
Understanding the Gut-Brain Axis
The gut-brain axis is a complex, bidirectional network linking the central nervous system (CNS)—primarily the brain—and the gastrointestinal (GI) tract. Communication occurs via multiple pathways:
- Nerves (especially the
vagus nerve
) - Hormones
- Immune system mediators
- Gut microbiota (the trillions of bacteria resident in your intestines)
This axis allows the gut and brain to exchange information, influencing emotions, stress response, pain perception, and even immune function. A healthy gut-brain connection is essential for optimal digestion and overall wellbeing.
The Role of the Vagus Nerve in Digestion
The vagus nerve is the largest and most important nerve connecting the brain to the digestive tract. It helps regulate several critical digestive processes:
- Production and release of stomach acid and digestive enzymes
- Movement of food through the digestive system (motility)
- Communication of sensation (fullness, pain, nausea) from the gut to the brain
When the vagus nerve sends calming, parasympathetic signals—often known as “rest and digest”—it promotes smooth, balanced digestion. When the nerve’s function is suppressed or disrupted by stress, digestive efficiency drops, and symptoms frequently arise.
How Stress Impacts Digestion
Stress, whether acute or chronic, triggers a “fight-or-flight” response that redirects energy and resources to vital organs needed for immediate survival. Digestion, being a non-essential process during emergencies, is suppressed. Here’s how:
- Decrease in digestive enzymes and stomach acid
- Slowed movement of food through the GI tract (delayed gastric emptying)
- Reduced blood flow to the intestinal walls
- Changes in the composition of gut bacteria (microbiome)
These changes can lead to multiple symptoms, from “butterflies” and mild nausea to chronic digestive disorders.
Common Digestive Symptoms Triggered by Stress
- Indigestion and bloating
- Heartburn and acid reflux
- Nausea or a “knot” in the stomach
- Constipation or diarrhea (sometimes alternating)
- Abdominal pain or cramping
- Loss of appetite or overeating
The Vicious Cycle: Stress and Gut Sensitivity
For many, digestive discomfort increases anxiety, creating a feedback loop where worrying about gut symptoms amplifies both stress and digestive troubles. This cycle is particularly prominent in functional GI disorders like irritable bowel syndrome (IBS).
Stress-Related Digestive Disorders
While stress alone rarely “causes” chronic GI diseases, it is a powerful trigger for symptom flare-ups and can contribute to the onset of functional disorders. Some of the most common include:
- Irritable Bowel Syndrome (IBS): Characterized by abdominal pain, bloating, constipation, diarrhea, or an alternating pattern. Stress is a central player in IBS onset and symptom severity.
- Gastroesophageal Reflux Disease (GERD): Stress worsens reflux by slowing gastric emptying and increasing stomach acid.
- Functional Dyspepsia: Upper abdominal discomfort, nausea, and fullness often worsened by stressful events or anxiety.
- Peptic Ulcers: While ulcers are primarily caused by infection (H. pylori) or medications, stress can exacerbate the condition and delay healing.
- Inflammatory Bowel Diseases (IBD) like Crohn’s or Ulcerative Colitis: Stress can trigger or worsen flares, although it is not the root cause.
Mechanisms: How Stress Alters Gut Function
Researchers have identified several physiological changes that occur in the digestive tract under stress:
- Altered GI Motility: Stress can speed up (causing diarrhea) or slow down (leading to constipation) the movement of food through your intestines.
- Increased Intestinal Permeability: Often dubbed “leaky gut,” stress can make the gut lining more permeable to bacteria and toxins, potentially triggering inflammation.
- Changes in Gut Secretions: Reduced digestive enzymes and stomach acid impede proper breakdown and absorption of nutrients.
- Impaired Blood Flow: Blood is shunted away from the intestines, reducing their function and increasing nausea or pain.
- Immune Modulation: Stress disrupts the immune component of the gut, leading to higher production of pro-inflammatory cytokines and altering the balance of gut bacteria.
- Mast Cell Activation: Special immune cells (mast cells) respond to brain-gut signals and release chemicals that drive pain, motility changes, and inflammation.
The Vagus Nerve in Stress Response
During relaxation—or “rest and digest”—the vagus nerve is highly active. It slows the heart rate, increases digestive secretions, and mediates anti-inflammatory signals throughout the gut.
When stress strikes, sympathetic (“fight-or-flight”) signals overpower the vagus nerve, leading to:
- Suppressed signaling to digestive organs (reduced motility and secretions)
- Decreased production of neurotransmitters promoting gut harmony and balance
- Increased stress hormones (cortisol, adrenaline) circulating in the gut
- Loss of anti-inflammatory influence, raising risk for chronic discomfort or disease
Chronic stress can even “downregulate” the vagus nerve itself, reducing its activity, worsening inflammation, and triggering persistent GI dysfunction .
Symptoms and Signs of Stress-Induced Digestive Issues
Everyone experiences stress differently, but some of the most frequent gut-related complaints include:
- Bloating or excess gas
- Irregular bowel movements: diarrhea, constipation, or both
- Stomach cramps or pain
- Indigestion, heartburn, or reflux after eating
- Sensation of “butterflies,” knots, or persistent unease in the abdomen
- Nausea, especially in acute anxiety or high-pressure situations
- Reduced or increased appetite
If you notice a consistent link between emotional stress and these types of symptoms, your digestive complaints may be stress-mediated rather than structural.
Supporting Gut Health During Stress
1. Activate the Relaxation Response
- Practice deep breathing, progressive muscle relaxation, or meditation to stimulate the vagus nerve.
- Take breaks to decompress during stressful periods; even a few minutes can help calm your body’s stress chemistry.
- Gentle physical activity such as walking or yoga encourages parasympathetic (rest-and-digest) tone.
2. Focus on Mindful Eating
- Eat your meals slowly and in a calm environment, away from distractions or emotional triggers.
- Avoid overeating or consuming heavy/fatty foods during periods of high stress.
- Chew food thoroughly to help your digestive enzymes work more effectively.
3. Maintain a Healthy Gut Microbiome
- Eat a diverse, plant-rich diet to support beneficial bacteria.
- Avoid unnecessary antibiotics and manage chronic stress, both of which disrupt the microbiota.
- Consider probiotic foods (like yogurt or fermented vegetables) if tolerated.
4. Seek Professional Help if Needed
- If digestive symptoms persist or affect quality of life, consult your healthcare provider to rule out underlying GI disorders.
- Mental health support (therapy, stress management programs) can have profound positive effects on gut symptoms.
Restoring vagal tone and addressing stress can significantly improve not only digestive symptoms but your overall sense of wellbeing.
Frequently Asked Questions (FAQs)
Q: How exactly does stress “shut down” digestion?
A: During stress, the body releases hormones like adrenaline and cortisol, which signal the sympathetic nervous system to divert blood flow and resources away from the digestive tract. This suppresses digestive secretions, reduces gut motility, and impairs nutrient absorption.
Q: What is the vagus nerve, and how can I support it?
A: The vagus nerve is the main parasympathetic nerve connecting your brain to most major organs, including the gut. Activities like slow, deep breathing, meditation, laughter, and regular movement all help increase vagal tone and enhance “rest and digest” processes.
Q: Do stress-related digestive symptoms mean I have a serious disease?
A: Not necessarily. Stress can trigger uncomfortable but harmless symptoms (like bloating, cramping, or diarrhea). However, if symptoms are severe, prolonged, or accompanied by “red flags” (significant weight loss, bleeding, fever), see a medical professional for evaluation.
Q: Can meditation or mindfulness really help my digestion?
A: Yes. Mindfulness-based stress reduction, meditation, and breathing exercises have shown positive results in reducing symptoms of IBS, indigestion, and other functional GI disorders by calming the stress response and supporting vagal nerve health.
Q: How fast do stress-related gut symptoms resolve?
A: This varies. For mild, acute stress, symptoms may fade within hours if you can relax. Chronic stress may require lifestyle changes and professional support to resolve persistent digestive issues.
Key Takeaways
- **Stress suppresses digestion** by diverting energy away from the gut via the “fight-or-flight” response.
- The
vagus nerve
is vital in promoting digestion and relaying gut-brain signals; stress inhibits its function. - Common results include bloating, diarrhea, constipation, and exacerbation of conditions like IBS and reflux.
- Managing stress and strengthening vagal tone can dramatically improve digestive health.
References
- Stress and the Digestive System – BYU CAPS
- How Does Stress Affect the Digestive System? – Houston Methodist
- The Hidden Connection Between Stress and Your Gut – North Central Health Care
- How Stress Affects Digestion—And What You Can Do About It – Henry Ford Health
- Stress and the gut: pathophysiology, clinical consequences – PubMed
References
- https://caps.byu.edu/stress-and-the-digestive-system
- https://www.houstonmethodist.org/blog/articles/2023/feb/how-does-stress-affect-the-digestive-system/
- https://www.norcen.org/services/mental-health/stress-awareness-month/stress-and-your-gut/
- https://www.henryford.com/Blog/2021/07/How-Stress-Affects-Digestion
- https://pubmed.ncbi.nlm.nih.gov/22314561/
- https://www.health.harvard.edu/newsletter_article/stress-and-the-sensitive-gut
- https://physoc.onlinelibrary.wiley.com/doi/full/10.1113/JP281951
- https://pubmed.ncbi.nlm.nih.gov/37756251/
Read full bio of medha deb












