Stress Damaging the Gut Barrier: How Cortisol Drives Intestinal Permeability and Health Risks
Cortisol’s impact on intestinal defenses offers clues to preventing inflammation.
Stress Damaging the Gut Barrier: Cortisol and Permeability
The relationship between psychological stress and gut health has become a major area of research, revealing the significant role of stress hormones—particularly cortisol—in disrupting intestinal barrier integrity. This disruption increases intestinal permeability, commonly referred to as “leaky gut”, which can drive inflammation and heighten susceptibility to chronic diseases.
Table of Contents
- Introduction
- Gut Barrier Function: Structure and Importance
- The Stress Response: HPA Axis and Cortisol Release
- Mechanisms: How Stress and Cortisol Damage the Gut Barrier
- Consequences of Increased Intestinal Permeability
- Stress, Cortisol, and the Gut Microbiome
- Links to Chronic Disease
- Mitigating Stress-Induced Gut Barrier Damage
- Frequently Asked Questions
Introduction
Stress is a biological response affecting multiple body systems, notably the digestive tract. Acute and chronic psychosocial stress both activate the body’s hypothalamic-pituitary-adrenal (HPA) axis, resulting in increased glucocorticoid hormone production—primarily cortisol. Research in both animals and humans demonstrates that this hormonal surge negatively impacts the delicate intestinal barrier, primarily by increasing permeability and fostering pro-inflammatory changes.
Gut Barrier Function: Structure and Importance
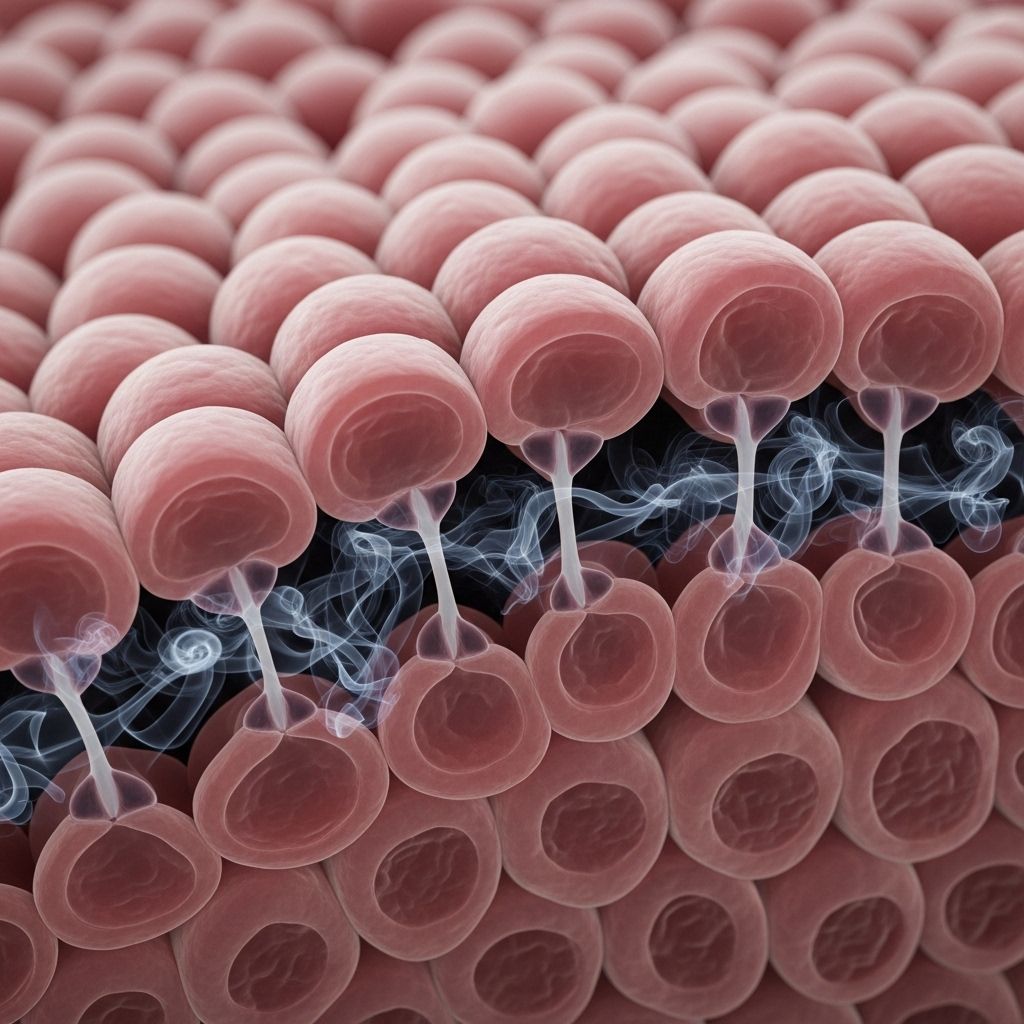
The gut barrier consists of a single layer of epithelial cells joined together by tight junction proteins (TJs; e.g., occludin, claudins, ZO-1), which physically block toxins, bacteria, and antigens from crossing into the bloodstream. Surrounding immune cells and a protective mucus layer further bolster this defense. This barrier’s integrity is essential for healthy digestion, nutrient absorption, and prevention of uncontrolled immune activation.
- Tight junction proteins regulate paracellular permeability, selectively enabling or restricting molecule passage.
- A healthy barrier prevents entry of luminal pathogens, undigested food particles, and bacterial products such as lipopolysaccharide (LPS).
- Disruption of tight junctions results in increased permeability or “leaky gut”.
The Stress Response: HPA Axis and Cortisol Release
When the brain perceives stress, the HPA axis is activated, involving three key steps:
- Hypothalamus releases corticotropin-releasing factor (CRF).
- Pituitary gland releases adrenocorticotropic hormone (ACTH).
- Adrenal cortex secretes cortisol into the bloodstream.
This orchestrated hormone cascade prepares the body for “fight or flight”, modifying central and peripheral systems including the gastrointestinal tract.
| HPA Axis Component | Hormone Produced | Effect on GI System |
|---|---|---|
| Hypothalamus | CRF | Stimulates stress signaling, alters gut motility and permeability |
| Pituitary | ACTH | Triggers cortisol release |
| Adrenal Cortex | Cortisol | Directly disrupts tight junctions, increases permeability, modulates immunity |
Mechanisms: How Stress and Cortisol Damage the Gut Barrier
Cortisol Effects on Tight Junctions
Cortisol profoundly influences the gut’s epithelial barrier, both acutely and chronically:
- Cortisol binds to glucocorticoid receptors present in gut epithelial cells, initiating transcriptional changes.
- Elevated cortisol suppresses the expression of key tight junction proteins, notably occludin and claudin-1, reducing the firmness of cellular junctions and increasing paracellular permeability.
- Animal studies show blocking glucocorticoid receptors prevents stress-induced gut permeability increase, confirming cortisol’s central role.
- Exposure to synthetic corticosteroids such as dexamethasone also increases permeability, demonstrating the effect is not limited to natural stress responses.
CRF and Mast Cell Activation
The relationship between stress, CRF, and gut permeability expands beyond cortisol:
- CRF triggers mast cell activation in the intestinal mucosa.
- Mast cells release mediators: histamine, cytokines (e.g., TNF-α, IL-6), and tryptase—all of which disrupt tight junctions.
- Animal studies with mast cell stabilizers show reduced permeability after stress, highlighting the critical link between CRF, mast cells, and barrier function.
Cytokines and Proteases: Amplifying Damage
- Pro-inflammatory cytokines (TNF-α, IFN-γ, IL-1β, IL-6) phosphorylate or downregulate tight junction proteins via kinase pathways.
- Proteases such as tryptase interact with protease-activated receptors, further loosening cellular contacts.
- An imbalance between inflammatory and anti-inflammatory responses drives sustained barrier dysfunction.
| Disruptive Agent | Source | Mechanism |
|---|---|---|
| Cortisol | Adrenal Cortex | Downregulates occludin, claudins |
| CRF | Hypothalamus | Triggers mast cell release |
| Mast Cell Mediators | Mast Cells | Histamine and tryptase damage TJs |
| Cytokines | Immune cells | Disrupt TJ distribution and function |
| Proteases | Immune cells, mast cells | Activate PARs to increase permeability |
Consequences of Increased Intestinal Permeability
Damage to the gut barrier yields local and systemic impacts:
- Translocation of antigens and bacteria: Bacterial endotoxins, food antigens, and pathogens migrate across the compromised intestinal lining into the bloodstream.
- Activation of immune responses: This triggers mucosal inflammation, often resulting in tissue damage and chronic immune activity.
- Systemic inflammation: Heightened permeability may contribute to low-grade systemic inflammation linked to diverse conditions including autoimmune and metabolic diseases.
- Development of visceral hypersensitivity: Increased permeability is associated with heightened sensitivity and pain, a hallmark of functional gut disorders.
Stress, Cortisol, and the Gut Microbiome
Beyond direct effects on barrier integrity, stress and cortisol adversely alter the gut microbiota:
- Elevated cortisol changes microbial composition, favoring growth of pro-inflammatory strains, reducing protective commensals.
- Gut dysbiosis further heightens permeability, creating a feedback loop of inflammation and barrier dysfunction.
- Studies show that the permeability-increasing effects of stress can begin in early development and are sensitive to interventions with beneficial bacteria.
- Altered microbiota also impact brain signaling, potentially amplifying stress responses and mood symptoms.
Links to Chronic Disease
Research links stress-induced gut barrier breakdown and increased permeability to several health conditions:
- Irritable Bowel Syndrome (IBS): Marked by chronic pain, altered bowel habits, and increased permeability, often worsened by psychological stress.
- Inflammatory Bowel Disease (IBD): Permeability changes may precede and aggravate intestinal inflammation.
- Metabolic Disorders: Systemic inflammation from gut-derived endotoxins is implicated in insulin resistance and obesity.
- Autoimmune Diseases: Excessive antigen crossing may provoke immune activation, increasing risk of autoimmunity.
- Mental Health: Gut-brain axis disruption affects mood, anxiety, and cognitive function.
Mitigating Stress-Induced Gut Barrier Damage
Strategies to reduce risk or repair stress-induced barrier dysfunction focus on both psychological and biological interventions:
- Stress management: Techniques such as mindfulness, meditation, cognitive behavioral therapy, and regular exercise have demonstrated efficacy in lowering cortisol and improving gut function.
- Mast cell stabilizers: Agents like disodium cromoglycate may block the CRF-mast cell axis, limiting permeability increases.
- Probiotics: Specific strains can restore microbiota balance and strengthen barrier integrity.
- Dietary support: Prebiotics, fiber, polyphenols, and nutrients like zinc fortify the mucosal barrier.
- Avoidance of chronic stressors: lifestyle modification and sleep hygiene are essential for long-term gut resilience.
Frequently Asked Questions
Q: How do I know if stress is affecting my gut barrier?
A: Symptoms may include digestive discomfort, increased food sensitivities, fatigue, and heightened inflammation. Diagnosis typically involves clinical assessment and may include tests for gut permeability.
Q: Is the damage caused by cortisol reversible?
A: With reduction of stress and supportive interventions (diet, probiotics, therapy), gut barrier function often improves, though chronic or severe disruption may require specialist care.
Q: Can lowering stress prevent gut-related diseases?
A: Lowering stress and cortisol can protect gut barrier integrity, reducing risk of disorders associated with increased permeability, such as IBS and IBD.
Q: Does the gut microbiome recover after stress?
A: With supportive dietary and probiotic interventions, microbial communities often rebalance following removal of chronic stressors.
Q: Are all types of stress equally damaging?
A: Chronic psychosocial stress tends to have more persistent and severe effects on the barrier than acute or physical stressors.
Conclusion
The evidence clearly links psychological stress and elevated cortisol to disruption of the gut’s epithelial barrier, resulting in increased intestinal permeability and a cascade of inflammatory and disease-promoting changes. Knowledge of these mechanisms empowers targeted interventions to mitigate damage and restore gut health.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10569989/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4288093/
- https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2015.00392/full
- https://www.nature.com/articles/s41598-017-04755-w
- https://physoc.onlinelibrary.wiley.com/doi/full/10.1113/JP281951
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1130689/full
- https://clasado.com/can-gut-bacteria-influence-stress-levels/
Read full bio of Sneha Tete












