Understanding the Intricate Connection Between Sleep Apnea and Metabolic Syndrome for Better Prevention and Care
Interrupted nighttime breathing can affect energy balance and heart health.
Sleep Apnea and Metabolic Syndrome Connection: A Comprehensive Exploration
Obstructive sleep apnea (OSA) and metabolic syndrome are two widespread modern health issues with significant, overlapping impacts on global well-being. Recent research underscores the importance of understanding how these conditions interact, fostering a cycle of risk that can drive the development of diabetes, obesity, cardiovascular diseases, and other metabolic disturbances. This article comprehensively examines their relationship, underlying mechanisms, implications for health, and future pathways toward effective prevention and treatment.
Table of Contents
- Overview of Sleep Apnea
- Understanding Metabolic Syndrome
- Epidemiological Interplay: Prevalence and Risk Factors
- Biological Mechanisms Linking OSA and Metabolic Syndrome
- Bidirectional Nature of the Relationship
- Clinical Implications and Cardiometabolic Risk
- Diagnosis and Assessment Strategies
- Management and Prevention Approaches
- Future Directions and Research
- Frequently Asked Questions (FAQs)
Overview of Sleep Apnea
Obstructive sleep apnea is a chronic disorder characterized by repeated episodes of partial (hypopnea) or complete (apnea) airway blockage during sleep, causing intermittent drops in oxygen saturation and frequent arousals. This results in poor sleep quality, daytime fatigue, and significant physiological stress on various organ systems.
- Prevalence: Estimates suggest that OSA affects about 17% of the general population, rising to 40–70% among obese individuals.
- Key Features: Loud snoring, waking episodes of choking or gasping, excessive daytime sleepiness, morning headaches, impaired cognitive and metabolic function.
- Main Risk Factors: Obesity, male gender, older age, craniofacial abnormalities, family history, alcohol or sedative use, and certain endocrine disorders.
Understanding Metabolic Syndrome
Metabolic syndrome (MetS) refers to a cluster of interconnected risk factors that significantly increase the likelihood of developing type 2 diabetes, cardiovascular disease, and stroke. A diagnosis is typically made when three or more of the following are present:
- Central (abdominal) obesity
- Elevated blood pressure (hypertension)
- High fasting blood glucose levels or diagnosed diabetes
- Increased triglycerides
- Low high-density lipoprotein (HDL) cholesterol
The accumulation of these risk factors contributes substantially to inflammation, insulin resistance, atherosclerosis, and subsequent chronic diseases.
Epidemiological Interplay: Prevalence and Risk Factors
A growing pool of research confirms a strong association between OSA and metabolic syndrome. Studies reveal:
- A significantly higher prevalence of metabolic syndrome among those with OSA compared to those without.
- In one study, 60% of patients with OSA met criteria for metabolic syndrome — versus 40% of those without significant OSA (p = .004).
- The proportion with hypertension was markedly higher in OSA patients (77% vs 51%).
- Traits such as BMI, waist circumference, triglycerides, hypertension, and type 2 diabetes are all found to be causally linked to both OSA and metabolic syndrome.
Key Risk Factors Shared by OSA and MetS:
- Obesity (particularly central adiposity)
- Advanced age
- Male sex (especially in those over 50)
- Physical inactivity
- Poor glycemic control and insulin resistance
- Chronic inflammation and oxidative stress
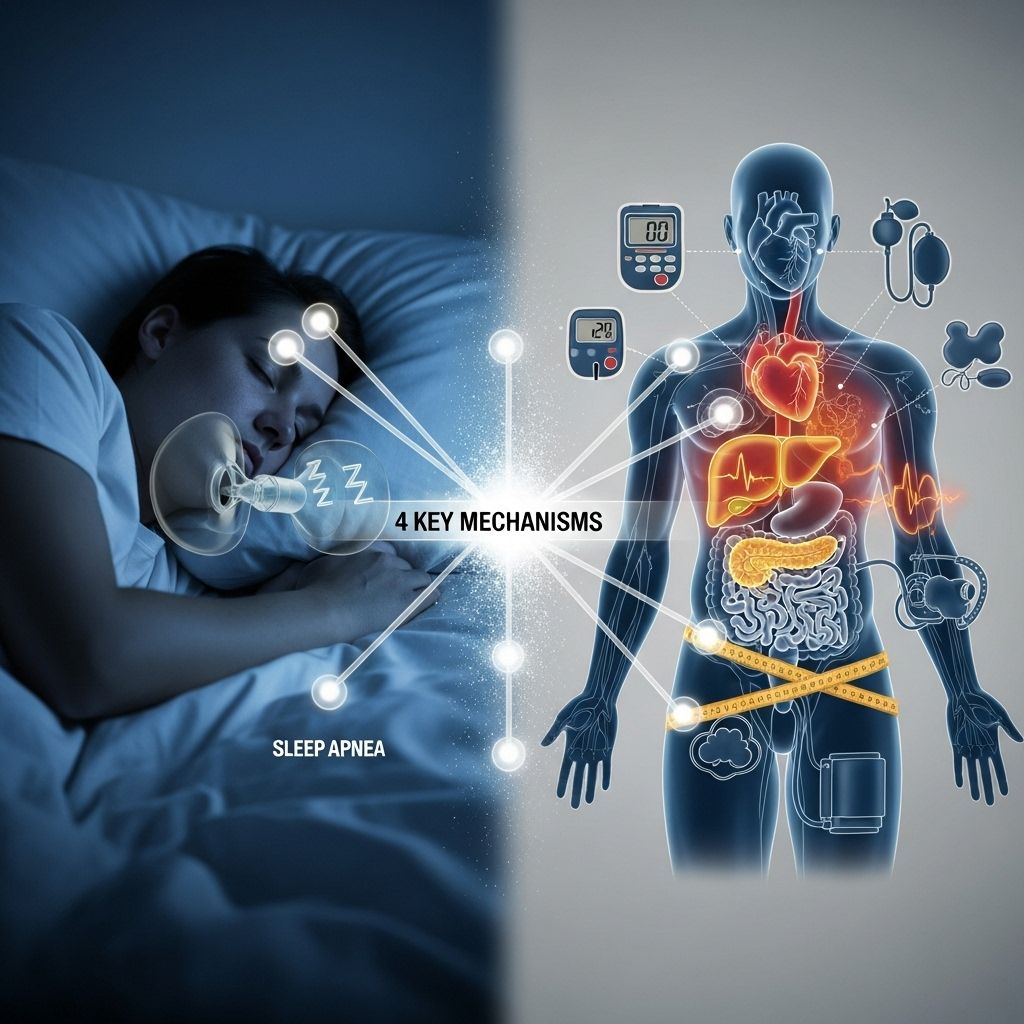
Biological Mechanisms Linking OSA and Metabolic Syndrome
The OSA–MetS relationship is multifactorial and complex. Central to this connection are several overlapping pathways:
1. Intermittent Hypoxia and Sleep Fragmentation
OSA causes repeated oxygen deprivation and sleep disruption, triggering:
- Increased sympathetic nervous system activity (“fight or flight” hormones)
- Oxidative stress damaging tissues and blood vessels
- Systemic inflammation
- Hormonal changes affecting appetite and metabolism
These effects contribute to hypertension, glucose intolerance, and lipid abnormalities — core features of metabolic syndrome.
2. Insulin Resistance and Glucose Metabolism
OSA is a key driver of insulin resistance, impairing the ability of tissues to use glucose efficiently. This is due to:
- Stress hormones (cortisol, catecholamines) rising at night and disrupting normal insulin action
- Adipokine imbalances (such as abnormal leptin and adiponectin production)
- Direct impact of fragmented sleep on glucose homeostasis
3. Dyslipidemia and Lipid Profile Changes
Intermittent hypoxia in OSA may alter lipid metabolism, increasing triglycerides and reducing HDL cholesterol, thus raising atherosclerotic risk.
4. Appetite Regulation and Weight Gain
Sleep fragmentation disrupts appetite-regulating hormones:
- Elevated ghrelin (increases hunger)
- Reduced leptin sensitivity (reduces satiety)
This hormonal environment promotes weight gain—a major driver for both OSA and MetS.
Bidirectional Nature of the Relationship
Research now supports the notion that the OSA–MetS connection is bidirectional:
- OSA contributes to metabolic dysfunction by worsening insulin resistance, promoting hypertension, and fostering dyslipidemia.
- Metabolic syndrome and its components can worsen OSA: Obesity, especially central fat accumulation, can mechanically narrow the airway, while physiology-dependent mechanisms (i.e., altered chemosensitivity, increased inflammation) further destabilize breathing during sleep.
- Metabolic diseases (diabetes, obesity) can exacerbate OSA, possibly through both mechanical (weight-dependent) and biological (weight-independent) means.
| OSA Effect on MetS | MetS Effect on OSA |
|---|---|
| Promotes insulin resistance | Obesity increases airway obstruction |
| Raises blood pressure (hypertension) | Hyperglycemia affects ventilatory control |
| Disrupts lipid metabolism | Lipid abnormalities may alter airway structure |
| Increases systemic inflammation | Inflammation worsens airway collapsibility |
| Drives increased fat accumulation | Weight gain increases OSA severity |
Clinical Implications and Cardiometabolic Risk
The co-existence of OSA and metabolic syndrome—notably in older men—amplifies the risk for cardiovascular morbidity and mortality. Noteworthy points include:
- OSA is more strongly related to hypertension than to diabetes or dyslipidemia within metabolic syndrome.
- Severity of OSA correlates with the likelihood of metabolic syndrome presence; i.e., more severe OSA, more likely to have MetS.
- People with both OSA and MetS have a heightened likelihood for heart attack, stroke, arrhythmias, and nonalcoholic fatty liver disease.
Sex and Age Effects:
- OSA–MetS association is strongest in males over 50 years old, particularly regarding hypertension.
- In women and younger men, the relationship is less consistent, possibly due to differences in body fat distribution, hormonal milieu, and lifestyle.
Diagnosis and Assessment Strategies
Timely recognition of both OSA and metabolic syndrome is critical for effective risk mitigation.
Diagnosis of OSA:
- Polysomnography (overnight sleep study; gold standard for diagnosis)
- Home sleep apnea testing (in selected cases)
- Clinical assessment (snoring history, questionnaires such as STOP-Bang or Epworth Sleepiness Scale)
Diagnosis of Metabolic Syndrome:
- Measurement of central obesity (waist circumference)
- Blood pressure assessment
- Fasting glucose and oral glucose tolerance test
- Lipid panel (triglycerides and HDL)
Management and Prevention Approaches
Addressing both OSA and metabolic syndrome often requires a multidisciplinary, personalized approach targeting lifestyle, physical, and metabolic risk factors.
1. Weight Loss and Lifestyle Modification
- Caloric restriction, balanced diet, and regular physical activity are effective in reducing both OSA severity and metabolic syndrome components.
- Behavioral therapies, nutritional counseling, and structured weight-loss programs can substantially improve outcomes.
2. Positive Airway Pressure (PAP) Therapy
- Continuous positive airway pressure (CPAP) is the first-line treatment for moderate-to-severe OSA.
- CPAP not only reduces apneic episodes but may also improve insulin sensitivity, blood pressure, and lipid profiles, though effects vary per individual.
3. Pharmacologic Interventions
- Antihypertensive, lipid-lowering, and antidiabetic drugs may be necessary for metabolic syndrome management.
- No medications specifically cure OSA, but addressing metabolic risk factors can have indirect benefits.
4. Addressing Behavioral and Environmental Factors
- Sleep hygiene education (consistent sleep schedule, sleep environment optimization)
- Avoidance of alcohol and sedatives before bedtime
- Management of comorbid depression or anxiety
Interventional and Surgical Options may be appropriate for select OSA patients, particularly with craniofacial or airway anomalies.
Future Directions and Research
Ongoing research strives to untangle the complex biochemical and genetic pathways linking OSA and metabolic syndrome. Key directions include:
- Deepening understanding of genetic determinants of OSA and metabolic dysfunction.
- Identifying molecular mediators that could serve as therapeutic targets.
- Exploring novel anti-inflammatory or metabolic therapies that also benefit sleep-disordered breathing.
- Clarifying how sex differences and age-specific factors modulate risk and response to treatment.
Ultimately, breaking the OSA–MetS cycle may require interventions that simultaneously address sleep, metabolism, weight, and cardiovascular health.
Frequently Asked Questions (FAQs)
Q: Can treating sleep apnea help reverse metabolic syndrome?
A: While treating OSA (e.g., with CPAP) has been shown to improve some metabolic parameters like blood pressure and insulin sensitivity, a comprehensive approach—including weight loss and management of all metabolic risk factors—is necessary to effectively address metabolic syndrome as a whole.
Q: Does everyone with metabolic syndrome develop sleep apnea?
A: Not all individuals with metabolic syndrome have OSA. However, the conditions share many risk factors, particularly obesity and central fat accumulation, increasing the likelihood of comorbidity.
Q: What is the best way to assess the risk of both conditions?
A: Regular medical check-ups that include sleep assessments (for OSA symptoms) and screening for metabolic syndrome components (waist circumference, blood pressure, glucose, lipids) are key to early detection and prevention.
Q: Are the risks different for men and women?
A: The OSA–metabolic syndrome connection is strongest in older men, likely due to differences in fat distribution and hormonal status. However, both men and women are at risk, especially with advancing age and increasing obesity.
Q: Besides obesity, what other factors link sleep apnea and metabolic syndrome?
A: Inflammation, oxidative stress, disordered breathing, alterations in appetite hormones (such as leptin and ghrelin), and disruptions in circadian rhythm all contribute to the connection between OSA and metabolic syndrome, independent of body weight.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1978322/
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2018.00440/full
- https://www.nature.com/articles/s41598-024-77471-x
- https://www.dovepress.com/evaluate-the-relationship-between-obstructive-sleep-apnea-and-metaboli-peer-reviewed-fulltext-article-NSS
- https://www.nature.com/articles/s41598-021-88233-4
Read full bio of Sneha Tete












