Skin Barrier Dysfunction in Psoriasis: Unraveling Its Pathogenetic Role and Immune Crosstalk Explained
Discover why skin defenses fade and which innovations help reinforce epidermal health.
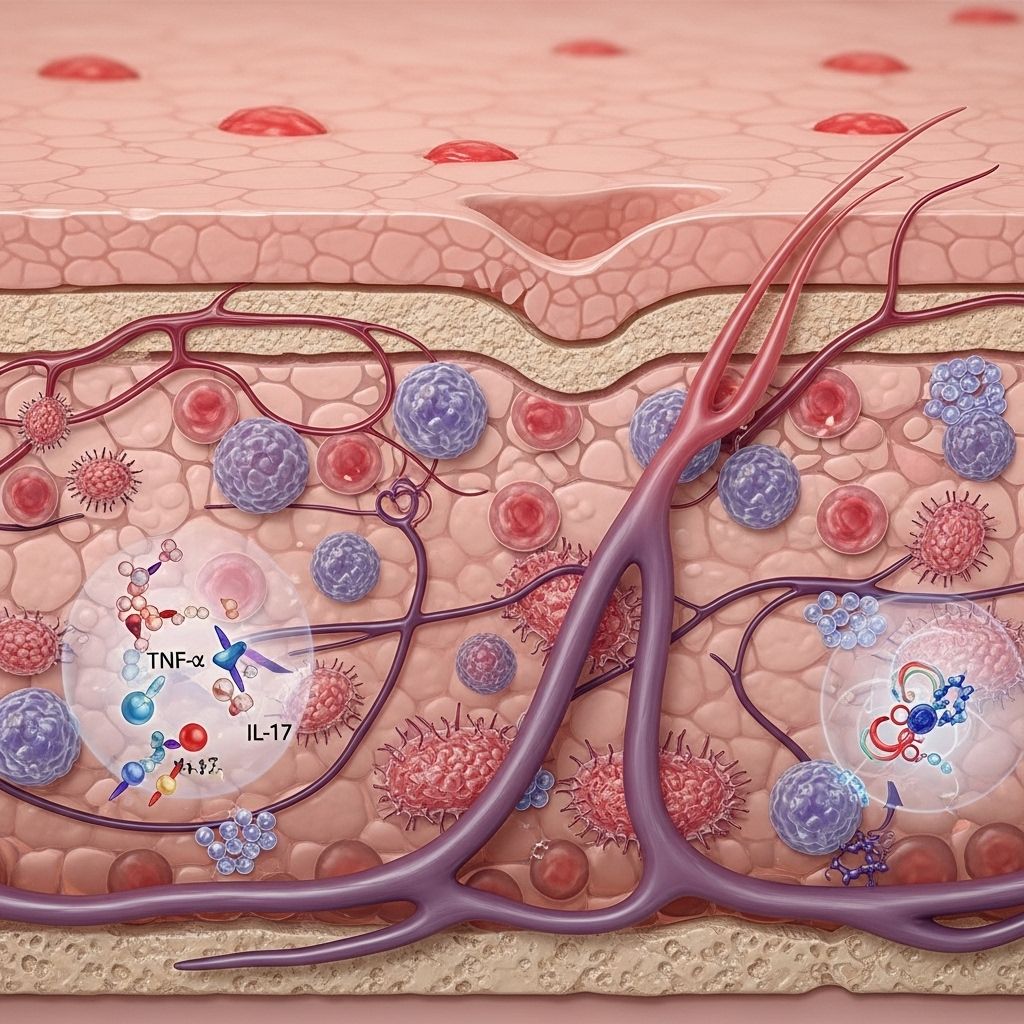
Table of Contents
- Introduction
- Overview of Psoriasis Pathogenesis
- The Skin Barrier: Structure and Function
- Genetic and Environmental Contributors to Skin Barrier Disruption
- Keratinocyte Dysfunction in Psoriasis
- Immune Crosstalk and the Barrier-Inflammatory Loop
- Key Molecular Pathways in Skin Barrier Impairment
- Autoimmunity, Molecular Mimicry, and Skin Barrier Dysfunction
- Clinical Manifestations and Implications
- Therapeutic Perspectives
- Frequently Asked Questions
- Conclusion
Introduction
Psoriasis is a chronic, immune-mediated inflammatory skin disease characterized by well-demarcated erythematous plaques, scaling, and variable degrees of pruritus. Far beyond being just a superficial dermatosis, psoriasis pathogenesis involves a complex interplay between genetic predisposition, environmental factors, systemic inflammation, and, critically, skin barrier dysfunction. Emerging evidence highlights the pivotal role of the epidermal barrier in initiating and perpetuating psoriatic inflammation, suggesting that therapeutic strategies targeting barrier restoration may provide disease-modifying benefits.
Overview of Psoriasis Pathogenesis
Psoriasis development is multifactorial. Historically, aberrant immune activation, particularly involving Th1 and Th17 cells, was thought to be the central driver. Current understanding, however, places keratinocytes and skin barrier disruption at the heart of disease initiation and perpetuation. Psoriatic lesions are sustained by a positive feedback loop in which immune-derived cytokines (such as IL-17, IL-22, IFN-γ, and TNF-α) stimulate keratinocyte proliferation and abnormal differentiation, while keratinocytes amplify inflammation by producing cytokines, chemokines, and antimicrobial peptides.
The Skin Barrier: Structure and Function
The skin barrier resides in the outermost layer of the epidermis, primarily the stratum corneum. It serves several essential functions:
- Physical Protection: Prevents excessive water loss and shields against mechanical, microbial, and chemical insults.
- Immunological Defense: Limits entry of allergens, pathogens, and irritants, and orchestrates local immune regulation through resident and recruited immune cells.
- Biochemical Regulation: Maintains surface pH, lipid composition, and ensures proper enzymatic activity essential for cell renewal and repair.
- Structural Integrity: Mediated by proteins such as filaggrin, loricrin, involucrin, and tight junctions that connect keratinocytes.
In healthy individuals, the barrier is a self-renewing, resilient shield. In psoriasis, however, this system is compromised due to genetic and inflammatory influences, exposing the skin to external triggers and fueling chronic inflammation.
Genetic and Environmental Contributors to Skin Barrier Disruption
Multiple factors contribute to the breakdown of the skin barrier in psoriasis:
- Genetic Mutations: Variants affecting epidermal integrity—such as mutations in genes related to barrier proteins, including filaggrin and card14—predispose individuals to epidermal leakiness and aberrant immune activation.
- Mechanical Stimuli: Intense scratching or trauma (the “Koebner phenomenon”) disrupts the barrier, promoting inflammation.
- Environmental Triggers: Infections (notably with Streptococcus), chemical irritants, and climate factors may exacerbate barrier compromise, precipitating or worsening psoriatic flares.
- Mutual Conversion: The frequent coexistence and overlap with atopic dermatitis (AD) points to shared pathogenic mechanisms rooted in barrier dysfunction, with both disorders involving increased epithelial susceptibility to allergens and activation of systemic Th2/Th17 inflammation.
Keratinocyte Dysfunction in Psoriasis
Keratinocytes, the main cellular component of the epidermis, play a dual role as structural elements and immune mediators. Their contribution to the psoriatic skin barrier defect includes:
- Abnormal Differentiation: Psoriatic keratinocytes show disturbed maturation, leading to parakeratosis, defective cornified envelope, and barrier disruption.
- Hyperproliferation: Driven by T cell cytokines, keratinocytes abnormally proliferate, thickening the epidermis and undermining normal barrier function.
- Cytokine Amplification: Upon activation, keratinocytes produce large amounts of chemokines (e.g., CXCL1, CXCL10, CCL20), antimicrobial peptides, and pro-inflammatory cytokines, further recruiting immune cells and escalating inflammation.
| Keratinocyte Function | Normal Skin | Psoriatic Skin |
|---|---|---|
| Differentiation | Orderly, forms intact barrier | Aberrant, leads to parakeratosis and barrier defects |
| Proliferation | Controlled renewal | Excessive, causes thickened, leaky barrier |
| Cytokine Production | Basal, regulated | Amplified, recruits immune cells, perpetuates inflammation |
Immune Crosstalk and the Barrier-Inflammatory Loop
Disruption of the skin barrier is both a cause and a consequence of immune activation in psoriasis:
- Cytokine-Induced Barrier Breakdown: Immune cells, notably Th17 and Th22 subsets, secrete cytokines (IL-17A, IL-22, IFN-γ, TNF-α) that suppress barrier protein expression, fueling further leakiness.
- The K17–T Cell–Cytokine Loop: K17 upregulation in keratinocytes (triggered by cytokines and downstream signaling such as ERK1/2, STAT3, AP-1) leads to production of IL-1β, chemokines (CXCL1, CXCL10, CXCL11, CCL20), and attracts T cells and neutrophils.
- Positive Feedback: Keratinocytes perpetuate inflammation by further releasing chemokines and antimicrobial peptides, recruiting more immune cells, thus sustaining and amplifying the cycle.
These complex interactions establish a self-sustaining inflammatory loop, with the compromised skin barrier at its root.
Key Molecular Pathways in Skin Barrier Impairment
Several molecular signaling mechanisms drive both the barrier defect and immune activation:
- Nrf2, STAT1/3, AP-1, and ERK1/2: Transcription factors activated in keratinocytes upon external stimuli and cytokine presence, leading to upregulation of K17 and other pro-inflammatory mediators.
- NF-κB Pathway: Canonical and non-canonical NF-κB signaling regulate both keratinocyte inflammation and barrier protein expression, shaping disease severity.
- Cytokine-driven Suppression: IL-22, via STAT3, inhibits expression of key barrier proteins such as K1, K10, impairing epidermal structure and function.
- Genetic Mutations: CARD14 mutations in keratinocytes amplify IL-17A signaling, increasing susceptibility to psoriatic inflammation.
Autoimmunity, Molecular Mimicry, and Skin Barrier Dysfunction
Barrier impairment enhances antigen penetration and autoimmune responses:
- Molecular Mimicry: Peptides derived from K17 in psoriatic lesions mimic M protein from Streptococcus, acting as autoantigens that polarize naive T cells toward Th1, Th17, and Th22 lineages, compounding immune activation.
- Autoimmunity Loop: The subsequent release of IFN-γ, IL-17A, IL-22, and TNF-α activates further keratinocyte proliferation and cytokine production, deepening barrier compromise and inflammation.
- Exacerbation and Spread: Augmented immune responses not only worsen local barrier defects but can drive systemic inflammation and extra-cutaneous disease manifestations.
Clinical Manifestations and Implications
The direct effects of skin barrier dysfunction are visible in the characteristic features of psoriasis:
- Plaque Formation: Hyperproliferative, poorly differentiated keratinocytes form thick, scaly plaques with defective barriers.
- Increased Susceptibility: Compromised barrier heightens vulnerability to trauma, secondary infection, and exposure to allergens.
- Systemic Effects: Resultant chronic skin inflammation may contribute to systemic comorbidities, including psoriatic arthritis and metabolic syndrome.
- Shared Pathogenesis: Overlap with atopic dermatitis due to mutual barrier defects underscores the importance of epidermal health in diverse diseases.
Therapeutic Perspectives
Targeting skin barrier impairment offers promising avenues for disease control:
- Barrier Restoration: Use of emollients, lipid-replenishing agents, and physical barrier enhancers may reduce disease severity and prevent flares in responsive groups.
- Molecular Therapy: Agents targeting keratinocyte signaling pathways—NF-κB inhibitors, cytokine blockers, and modulators of Nrf2 or STAT3 signaling—can address both barrier function and immune cycles.
- Biologics: Monoclonal antibodies targeting IL-17A, IL-22, TNF-α, and related molecules disrupt the keratinocyte-immune cell feedback loop, leading to symptom improvement and barrier restoration.
- Preventive Approaches: Early intervention in individuals with genetic risk factors, or those with sensorily positive family histories, may attenuate barrier breakdown and avert clinical onset.
Frequently Asked Questions
Q: Why does the skin barrier break down in psoriasis?
A: The skin barrier is disrupted in psoriasis due to genetic mutations affecting epidermal integrity, cytokine-driven suppression of barrier proteins, mechanical trauma, and chronic inflammatory signaling between keratinocytes and immune cells.
Q: How does skin barrier dysfunction contribute to immune activation?
A: A compromised barrier allows entry of environmental antigens and microbial components, triggering keratinocyte activation and recruitment of T cells and other inflammatory cells. This perpetuates a cycle of chronic inflammation and tissue repair failure.
Q: Can skin barrier restoration therapies improve psoriasis?
A: Yes, therapies aimed at restoring barrier function, along with those targeting immune signaling, show clinical benefit by interrupting the pathogenic feedback loop and improving symptoms.
Q: Is skin barrier dysfunction unique to psoriasis?
A: While not exclusive, barrier dysfunction is central to several inflammatory skin diseases, including atopic dermatitis. Overlapping mechanisms highlight the broader relevance of epidermal health in dermatology.
Q: What genes are implicated in keratinocyte/barrier dysfunction?
A: Mutations in filaggrin and card14 are among those linked to barrier impairment and inflammatory amplification in psoriasis.
Conclusion
Psoriasis exemplifies the profound impact of skin barrier disruption in triggering and sustaining chronic cutaneous inflammation. Genetic, environmental, and immunological factors converge to break down epidermal integrity, amplify keratinocyte dysfunction, and perpetuate immune activation. Understanding these mechanisms not only widens our perspective on the pathogenesis of psoriasis but also paves the way for targeted therapeutic interventions that restore barrier function, control inflammation, and improve patient outcomes.
References
Read full bio of Sneha Tete












