Skin Barrier Function: Definition, Role, Essential Structure, and Significance in Health
A resilient outer layer locks in moisture and shields skin from environmental damage.
The skin barrier is pivotal for human health, serving as the body’s primary shield against environmental threats and maintaining internal homeostasis. Its complex structure, crucial protective roles, and vulnerability to damage make understanding the skin barrier essential for anyone seeking optimal skin health. This comprehensive guide outlines the definition, role, mechanisms, factors affecting, and methods to protect the skin barrier.
Table of Contents
- Definition of Skin Barrier
- Structure of the Skin Barrier
- Functions and Roles of the Skin Barrier
- Mechanisms of Skin Barrier Protection
- Factors Affecting Skin Barrier Function
- Signs and Consequences of Barrier Dysfunction
- Strategies to Protect and Restore the Skin Barrier
- Frequently Asked Questions
Definition of Skin Barrier
The skin barrier refers to the outermost layer of the skin—primarily the stratum corneum of the epidermis—responsible for protecting the body from the external environment while preventing excessive loss of moisture and electrolytes from within. This ‘barrier function’ is essential for survival, as it maintains a controlled exchange between the body’s internal and external environments by limiting permeability.
The skin barrier:
- Restricts the entry of pathogens, toxins, and irritants
- Prevents water and electrolyte loss through evaporation
- Acts as a physical, chemical, immune, and microbiological shield
Without this function, the body would be highly susceptible to infection, dehydration, and environmental injury.
Structure of the Skin Barrier
The skin is composed of three main layers:
- Epidermis: The thin, outermost layer, which includes the stratum corneum
- Dermis: The thicker, middle layer containing collagen, elastin, blood vessels, nerve endings, and glands
- Subcutaneous tissue (Subcutis): The innermost, predominantly fatty layer responsible for insulation and shock absorption
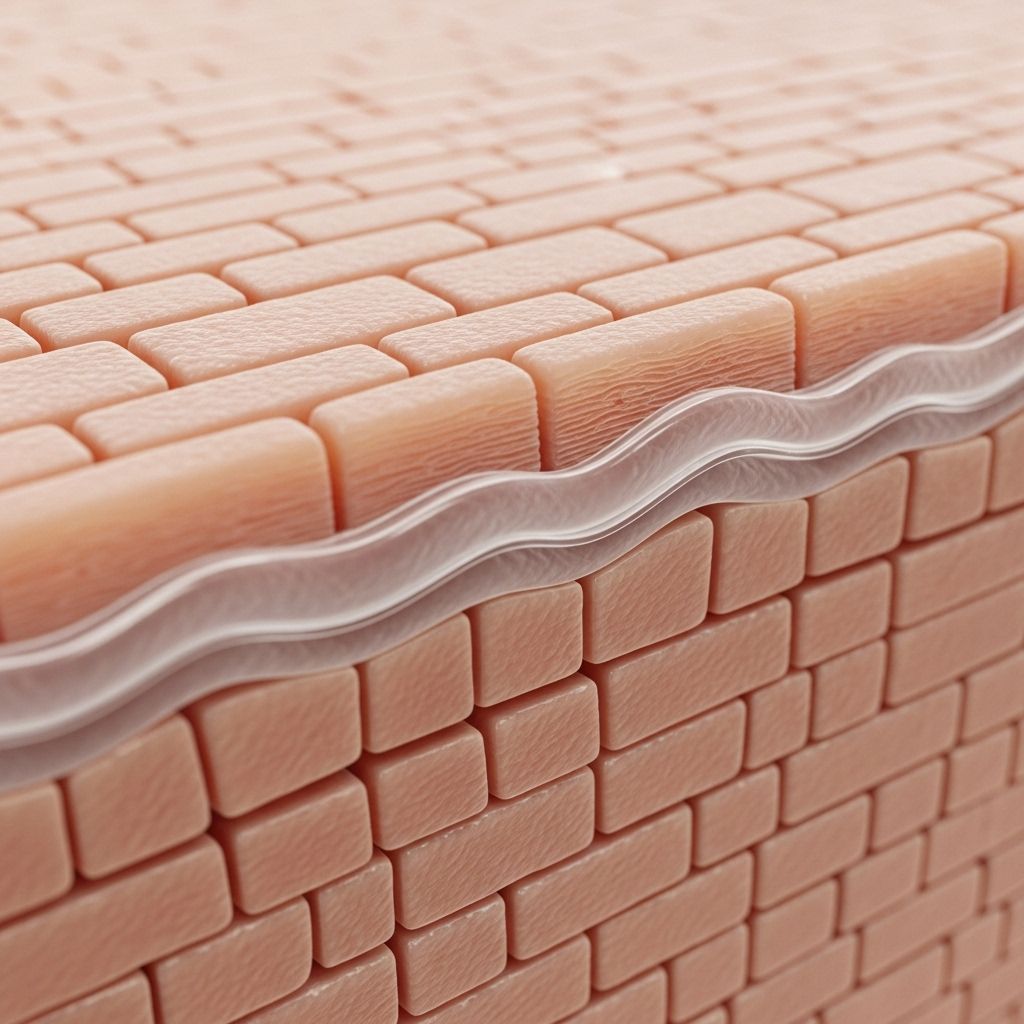
The epidermal stratum corneum is central to the skin barrier. Its structure is often likened to a brick-and-mortar wall:
- Bricks: Flattened, dead cells called corneocytes
- Mortar: Intercellular lipids, mainly ceramides, cholesterol, and fatty acids
Other structural features:
- Filaggrin: A protein in the skin that helps produce natural moisturizing factors (NMFs)
- Lipid matrix: Holds cells together, regulates permeability, and retains moisture
- Acid mantle: The slightly acidic surface film (pH 4.5-5.5) that supports enzymes and the skin microbiome
| Component | Description | Main Functions |
|---|---|---|
| Corneocytes (Bricks) | Flattened, dead epidermal cells rich in keratin | Provide mechanical strength and carry NMFs |
| Lipids (Mortar) | Ceramides, cholesterol, fatty acids | Bind cells, reduce permeability, prevent water loss |
| Filaggrin | Intracellular protein producing NMFs | Maintains hydration, supports barrier repair |
| Acid Mantle | Slightly acidic surface layer | Enables enzymatic activity, deters pathogens |
Functions and Roles of the Skin Barrier
The skin barrier performs several lifesaving and health-promoting functions:
- Physical barrier: Protects against mechanical injury, chemicals, particles, and microorganisms
- Preventing pathogenic entry: Stops bacteria, viruses, and fungi from penetrating the skin
- Regulating water loss: Minimizes transepidermal water loss (TEWL) to prevent dehydration
- Immune barrier: Hosts immune cells (e.g., Langerhans cells) that alert the immune system to danger
- Chemical barrier: Maintains the acid mantle to deter pathogens and optimize enzymatic reactions
- Microbiological barrier: Supports a beneficial microbiome that competes with harmful invaders
- Photoprotection: Partially absorbs and scatters ultraviolet (UV) radiation
- Regulating absorption: Controls which substances are allowed or blocked from systemic absorption
If the barrier fails, results can include infection, inflammation, and loss of vital fluids.
Mechanisms of Skin Barrier Protection
The effectiveness of the skin barrier is derived from multiple, interlocking mechanisms:
- Brick-and-mortar architecture: Corneocytes and lipid matrix form a dense, water-resistant wall
- Acid mantle: Low skin pH (4.5 – 5.5) inhibits harmful enzymes and pathogen colonization
- Moisturizing factors: Components like urea, lactic acid, and hyaluronic acid retain water in the stratum corneum
- Lipid metabolism: Enzymatic action maintains an optimal lipid composition for permeability regulation
- Immune surveillance: Specialized dendritic cells and antimicrobial peptides patrol the barrier
- Microbiota: Symbiotic skin microorganisms create competition for pathogens, supporting defense
Factors Affecting Skin Barrier Function
The skin barrier is prone to disruption by both internal and external factors, which can compromise its structure and function:
- Age: Lipid production decreases with age, especially after 40, leading to drier, less protective skin
- Environment: Cold, dry weather, wind, and air pollution can dehydrate or damage the barrier
- Harsh skincare: Over-washing, especially with hot water or strong soaps, strips protective lipids
- Chemical exposure: Detergents, solvents, certain cosmetics, and excessive exfoliation impair the barrier
- Medical conditions:
- Atopic dermatitis (eczema): Has impaired barrier function as a core defect
- Psoriasis: Disrupted cell turnover and lipid composition compromise strength
- Nutritional deficiencies: Lack of essential fatty acids, vitamins, or proteins impairs repair and maintenance
- Stress and hormones: Can alter immune regulation and barrier repair processes
Signs and Consequences of Barrier Dysfunction
When the skin barrier is damaged or weakened, typical symptoms and skin problems emerge:
- Dryness and flaking: Due to increased loss of water
- Irritation and sensitivity: Greater penetration of allergens and irritants
- Redness and inflammation: Resulting from immune activation and injury
- Itching: A common sign of compromised barrier function
- Infections: Bacteria, fungi, or viruses can invade more easily
- Slow healing: Impaired repair mechanisms
Chronic barrier dysfunction is implicated in skin diseases such as:
- Atopic dermatitis
- Psoriasis
- Contact dermatitis
- Ichthyosis
Strategies to Protect and Restore the Skin Barrier
Maintaining a healthy skin barrier requires both prevention and targeted interventions:
- Use mild, gentle cleansers: Avoid over-cleansing to preserve natural oils
- Moisturizers with ceramides and fatty acids: Restore lipids and aid repair
- Limit exfoliation: Avoid harsh scrubs and acids if the skin is sensitive or compromised
- Protect against environment: Use broad-spectrum sunscreen, and wear protective clothing in harsh weather
- Keep showers lukewarm: Hot water can strip the skin barrier
- Avoid irritating ingredients: Fragrances, alcohols, and unnecessary preservatives can weaken the barrier
- Support with diet: Ensure adequate intake of healthy fats, vitamins A, C, D, E, and hydration
- Promptly treat inflammation or infection: Use appropriate therapy as directed by dermatologists
Long-term barrier recovery often requires diligence and a gentle routine—sometimes, medical treatment may be necessary for persistent or severe dysfunction.
Frequently Asked Questions (FAQs)
Q: What exactly is the ‘skin barrier’?
The skin barrier refers to the outermost layer of the epidermis, known as the stratum corneum. It serves as the body’s first defense against environmental insults and prevents excessive loss of water and vital nutrients .
Q: Why is the skin barrier crucial for overall skin health?
A healthy skin barrier protects against infections, irritation, and dehydration, while supporting optimal skin appearance and comfort. Dysfunction is at the heart of many chronic skin conditions .
Q: What are the warning signs that my skin barrier is damaged?
Common symptoms of barrier dysfunction include dryness, flakiness, redness, sensitivity, itching, and a tendency to develop rashes or infections .
Q: Can the skin barrier repair itself if damaged?
Yes, the skin barrier has remarkable capacity for self-repair, especially with supportive care such as moisturizers containing ceramides and by avoiding irritants. However, severe or chronic damage may require medical intervention .
Q: Which skincare ingredients help restore the barrier?
- Ceramides
- Cholesterol
- Fatty acids
- Natural moisturizing factors
- Hyaluronic acid
- Colloidal oatmeal (for calming inflammation)
Key Takeaways
- The skin barrier is fundamental for health, acting as both a shield and regulator for the body
- Its ‘brick-and-mortar’ structure relies on both cellular components and a complex mixture of lipids
- Various factors can impair this barrier, but most damage is preventable or reversible with the right care
- Understanding and supporting the skin barrier is vital—not just cosmetically, but for overall wellbeing
For optimal skin health, focus on gentle cleansing, adequate moisturization, and the avoidance of irritants and harsh environmental exposures. Seek professional guidance if you experience persistent symptoms of barrier dysfunction.
References
- https://www.webmd.com/skin-problems-and-treatments/skin-barrier-what-to-know
- https://fiveable.me/key-terms/anatomy-physiology/barrier-function
- https://www.healthline.com/health/skin-barrier
- https://dermnetnz.org/topics/skin-barrier-function
- https://www.herrondermatology.com/understanding-your-skin-barrier/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2843412/
- https://www.codif-tn.com/en/news/24-the-barrier-function
- https://jcadonline.com/fundamentals-of-skin-barrier-physiology/
Read full bio of medha deb












