Secretory IgA (sIgA): Defending Gut Immunity and Preventing Leaky Gut Syndrome
An antibody shield that blocks harmful microbes while nurturing a balanced microbiome.
Secretory Immunoglobulin A (sIgA) is the most abundant antibody found at mucosal surfaces, acting as the immune system’s first responder within the intestines. Its pivotal function in gut immunity and role in preventing leaky gut syndrome is now at the forefront of mucosal immunology research.
Table of Contents
- Introduction: The Gut Immune System
- What is Secretory IgA (sIgA)?
- sIgA Production and Regulation
- Mechanisms of sIgA in Gut Immunity
- sIgA and Microbiota Balance
- When sIgA Fails: Leaky Gut and Chronic Disease
- Supporting Healthy sIgA Levels
- Frequently Asked Questions (FAQs)
Introduction: The Gut Immune System
The human gastrointestinal tract is a bustling ecosystem, housing trillions of microbes and processing a constant influx of dietary and environmental antigens. Maintaining a delicate balance between tolerance and defense is essential. The mucosal immune system—particularly the layer that lines the intestines—acts as a sentinel, preventing the entry of pathogens while preserving peaceful coexistence with beneficial microbes. Secretory IgA is a cornerstone of this defense strategy, shaping immune responses and maintaining epithelial integrity.
What is Secretory IgA (sIgA)?
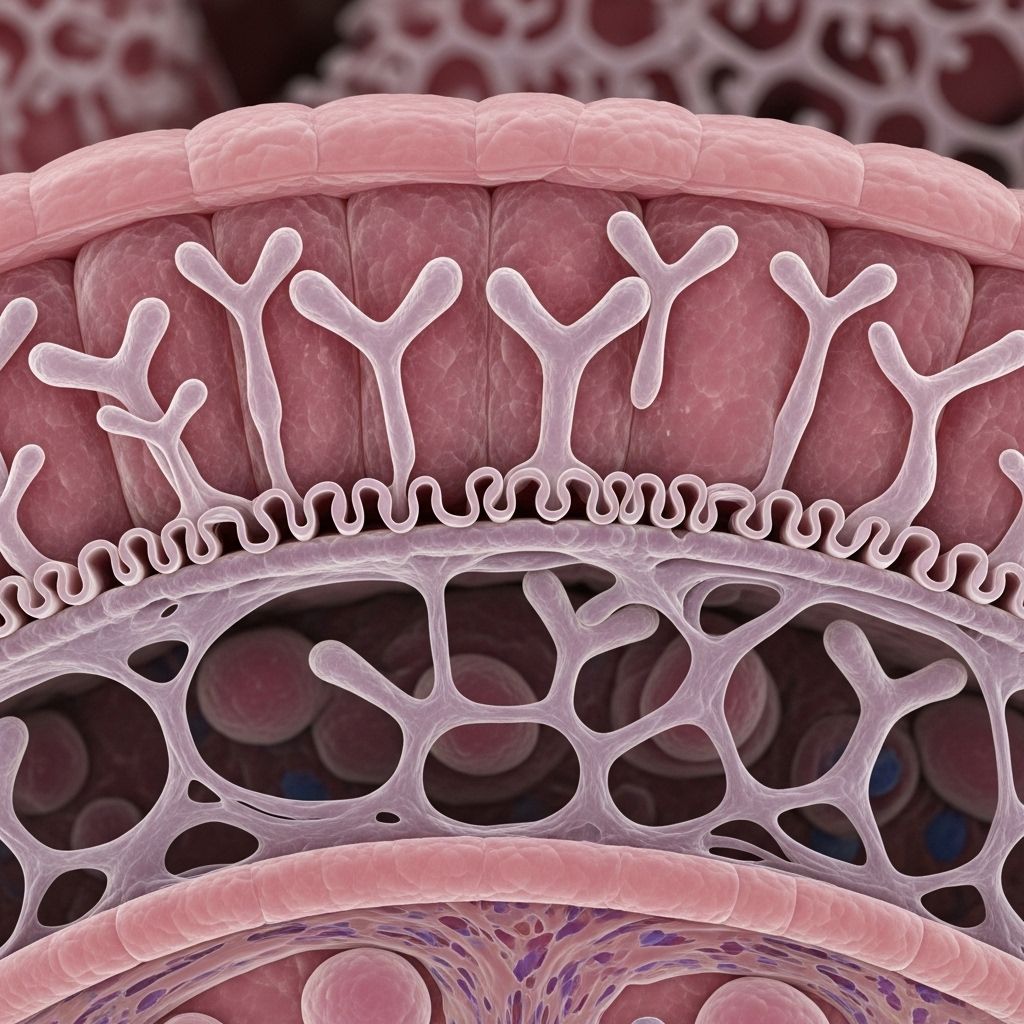
Immunoglobulin A (IgA) is one of several antibody classes produced by B cells, but what sets sIgA apart is its specialized movement to mucosal surfaces such as the gut, respiratory, and urogenital tracts. Structurally, sIgA mainly exists as a dimer—two IgA molecules joined by a J (joining) chain and protected by a secretory component. This design enables sIgA to be transported across the epithelium and to function optimally within the gut lumen.
Main Functions of sIgA at Mucosal Surfaces
- Blocks pathogens: Prevents microbes and toxins from attaching to epithelial cells.
- Immune exclusion: Binds to antigens and pathogens, aggregating and entrapping them in mucus for removal by peristalsis.
- Shapes microbiota: Helps select and foster a beneficial microbial community.
- Modulates inflammation: Downregulates pro-inflammatory responses to non-threatening materials.
sIgA Production and Regulation
Main production sites for sIgA are the gut-associated lymphoid tissue (GALT) and Peyer’s patches. Specialized M cells sample antigens from the gut lumen and present them to underlying dendritic cells. These, in turn, activate T cells and B cells, specifically inducing B cells to undergo class-switching to produce IgA antibodies. Several cytokines, including Transforming Growth Factor-beta (TGF-β) and Interleukin-10 (IL-10), are pivotal for sIgA production and for maintaining mucosal tolerance.
Key Regulators of sIgA Synthesis
- Cytokines: IL-4, IL-5, IL-6, IL-10, TGF-β
- Antigen-presenting cells: Dendritic cells within GALT and Peyer’s patches
- B cells: Class-switch recombination to IgA-producing plasma cells
- Microbiota: Commensal bacteria stimulate sIgA responses
Transport of sIgA
sIgA-producing plasma cells reside in the intestinal lamina propria. After synthesis, sIgA binds to the polymeric immunoglobulin receptor (pIgR) on intestinal epithelial cells, which shuttles it across the epithelial layer into the gut lumen. During this journey, the secretory component is added, enhancing sIgA’s resistance to gastrointestinal proteases.
| Property | sIgA | IgG |
|---|---|---|
| Location | Mucosal surfaces (gut, saliva, lungs) | Blood, tissues |
| Form | Dimeric with secretory component | Monomeric |
| Function | Immune exclusion, microbial balance | Complement activation, phagocytosis |
| Inflammation | Non-inflammatory | Pro-inflammatory |
Mechanisms of sIgA in Gut Immunity
The gut is perpetually exposed to a myriad of antigens. sIgA prevents harmful invaders from breaching the epithelial barrier while fostering immunological tolerance to food antigens and commensal microbes.
1. Immune Exclusion
sIgA binds to viruses, toxins, and pathogenic bacteria, preventing their attachment to and penetration of the intestinal epithelium. Aggregated pathogens become immobilized in mucus and are excreted from the body.
2. Entrapment and Mucociliary Clearance
By cross-linking microbial antigens and entrapping pathogens in mucus, sIgA helps clear them via peristalsis and mucociliary activity.
3. Downregulation of Inflammation
sIgA plays an essential role in downregulating excessive immune responses, especially those that might damage the delicate epithelial barrier. By binding to food and microbial antigens, sIgA prevents their interaction with the immune system, thus averting unnecessary inflammation.
4. Facilitation of Antigen Sampling
sIgA can facilitate the controlled sampling and retro-transport of antigens to dendritic cells in GALT, promoting mucosal tolerance rather than inflammatory responses.
sIgA and Microbiota Balance
One of sIgA’s recently appreciated roles is its ability to shape and stabilize the gut microbiota composition. sIgA recognizes patterns on both pathogenic and commensal bacteria:
- Promotes diversity: Selectively coats and fosters retention of beneficial bacteria, aiding their colonization.
- Prevents pathogen overgrowth: Restricts outgrowth of potential pathobionts.
- Maintains tolerance: Interacts polyreactively with multiple antigens, limiting unnecessary immune activation.
Deficiency in sIgA can result in significant microbiota alterations, with loss of commensal species that are normally sIgA-coated and increased susceptibility to opportunistic infections.
When sIgA Fails: Leaky Gut and Chronic Disease
“Leaky gut” describes increased intestinal permeability, where the barrier function of the gut lining breaks down, allowing bacteria, toxins, and other antigens to enter the bloodstream unchecked. This can promote local and systemic chronic inflammation, underpinning conditions like allergies, autoimmune disorders, metabolic syndrome, and even neurological problems.
How sIgA Protects Against Leaky Gut
- Maintains epithelial barrier integrity by blocking pathogen entry and neutralizing toxins before they reach the epithelial layer.
- Regulates immune responses, preventing excessive inflammatory signaling that can weaken tight junctions between epithelial cells.
- Shapes a healthy microbiota that inherently supports barrier health.
Consequences of Low sIgA
- Increased gut permeability: Reduced immune exclusion allows more antigens to contact and disrupt epithelial cells.
- Altered microbiota: Pathogen overgrowth and reduction in beneficial commensals exacerbate barrier dysfunction.
- Chronic inflammation: Enhanced antigen and microbe translocation drives persistent low-grade inflammation within the gut and body.
Clinical Conditions Linked to Impaired sIgA Function
- Recurrent gastrointestinal infections
- Inflammatory bowel diseases (IBD)
- Food sensitivities and allergies
- Autoimmune conditions (e.g., celiac disease, type 1 diabetes)
- Metabolic and neuroinflammatory disorders
Supporting Healthy sIgA Levels
Strategies to support optimal sIgA production and mucosal immunity:
- Balanced, nutrient-rich diet: Adequate levels of vitamins A, D, and zinc support mucosal immunity.
- Prebiotics and probiotics: Foster a balanced microbiota that stimulates robust sIgA production.
- Stress management: Chronic psychological stress is linked to sIgA reduction; techniques such as mindfulness, exercise, and sleep hygiene are beneficial.
- Avoidance of unnecessary antibiotics: Overuse can disrupt the microbiota and impair sIgA induction.
Identifying and addressing underlying causes—such as food intolerances, chronic infection, or dysbiosis—may also restore sIgA balance and strengthen barrier integrity.
Frequently Asked Questions (FAQs)
Q: What is the main role of Secretory IgA in the gut?
A: Secretory IgA’s chief role is preventing pathogens and toxins from crossing the gut barrier while supporting a balanced microbiota and suppressing non-threatening inflammatory reactions.
Q: How is sIgA measured and what are normal levels?
A: sIgA can be measured in stool or saliva. Reference ranges vary by laboratory, but persistently low levels may indicate compromised mucosal immunity.
Q: Does low sIgA cause leaky gut?
A: Low sIgA itself does not directly cause leaky gut but increases susceptibility to microbial imbalance and inflammation that contribute to the breakdown of the gut barrier.
Q: Can you increase sIgA levels naturally?
A: Yes. Supporting overall gut health through diet, stress reduction, and microbiota-supporting interventions can improve sIgA responses in many cases.
Q: Are there specific diseases caused by sIgA deficiency?
A: Selective IgA deficiency is associated with increased risk for recurrent mucosal infections, autoimmune conditions, and possibly allergies and gut disorders.
Summary Table: Key Functions of Secretory IgA
| Function | Description |
|---|---|
| Immune Exclusion | Prevents attachment and penetration of microbes and toxins. |
| Microbial Balance | Shapes gut microbiota by coating and supporting beneficial bacteria. |
| Modulation of Inflammation | Downregulates unnecessary immune responses to non-threatening antigens. |
| Barrier Integrity | Protects epithelial junctions and promotes mucosal healing. |
References
- PMC3774538 – “Secretory IgA’s Complex Roles in Immunity and Mucosal Homeostasis”
- Frontiers in Microbiology, 2022 – “SIgA in Host-Microbiota Interactions”
- Nature, 2011 – “Secretory IgA’s complex roles in immunity”
- Invivo Healthcare, 2022 – “How Secretory IgA Supports Immune Resilience”
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3774538/
- https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.880484/full
- https://www.nature.com/articles/mi201141
- https://invivohealthcare.com/education/articles/immune-resilience-secretory-iga/
- https://www.rupahealth.com/post/secretory-iga-understanding-high-and-low-levels-causes-and-treatment-options
- https://rupress.org/jem/article/215/8/2019/46045/IgA-regulates-the-composition-and-metabolic
Read full bio of medha deb












