Sebaceous Cyst vs. Epidermoid Cyst: Comprehensive Differences, Diagnosis, and Treatment Explained
Identifying skin lumps accurately supports better care and eases unnecessary worry.
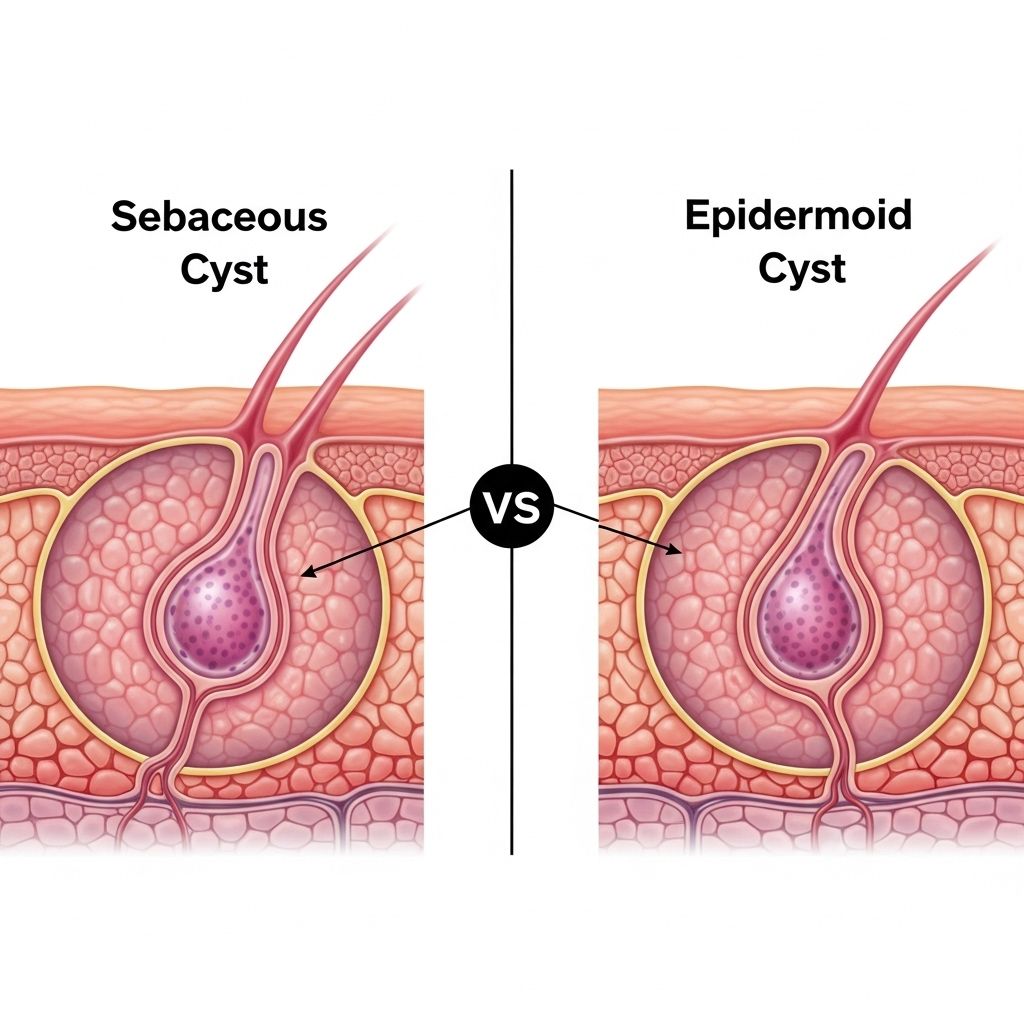
Skin cysts are a common concern in clinical and cosmetic dermatology. The terms sebaceous cyst and epidermoid cyst are frequently used interchangeably, but they represent distinct entities with important differences in origin, structure, clinical behavior, and management. Accurate identification is essential for optimal treatment and patient education. This article provides an in-depth, evidence-based comparison of sebaceous and epidermoid cysts, highlighting their distinguishing features, insights from dermatology practice, and current best practices for care.
Table of Contents
- Overview of Skin Cysts
- Definitions and Nomenclature
- Origins and Pathogenesis
- Epidemiology and Common Locations
- Clinical Presentation and Appearance
- Direct Comparison Table
- Diagnosis and Differential Diagnosis
- Treatment Options
- Recurrence & Risks
- When to Seek Medical Care
- Frequently Asked Questions (FAQs)
- Summary
Overview of Skin Cysts
Skin cysts are closed sacs or cavities filled with semi-solid or liquid material, usually arising from structures in the skin such as glands or hair follicles. Most are benign, but their cosmetic appearance, potential for inflammation, or tendency to rupture can cause discomfort or functional issues.
Definitions and Nomenclature
The term “sebaceous cyst” has been used in both lay and medical contexts to describe various skin lumps, but modern dermatology makes a key distinction:
- True Sebaceous Cyst: Originates from the sebaceous (oil) gland and contains sebum.
- Epidermoid Cyst: Arises from the superficial layer of skin (epidermis) or the upper portion of hair follicles; contains keratin. These are much more common.
Current clinical guidelines discourage using “sebaceous cyst” as a blanket term since most skin cysts previously labeled this way are actually epidermoid cysts. Accurate terminology improves diagnosis, guides surgical planning, and helps manage patient expectations.
Origins and Pathogenesis
Sebaceous Cysts
- Originate from sebaceous glands, which are responsible for producing sebum (the skin’s natural oil).
- Formation involves blockage of the gland’s duct, leading to accumulation of sebum within the gland and subsequent cyst formation.
- Much less common than often believed; true sebaceous cysts are rare.
Epidermoid Cysts
- Result from epidermal cells (outer skin cells) becoming trapped within the dermis instead of being shed normally .
- Cells continue to divide and produce keratin, a cheese-like protein that accumulates as the cyst fills.
- Often linked to trauma (such as a scratch or injury) or blockage of hair follicles.
Epidemiology and Common Locations
| Cyst Type | Common Sites | Relative Frequency |
|---|---|---|
| Sebaceous | Scalp, face (especially behind ears), neck, back | Rare |
| Epidermoid | Face, trunk, neck, upper back, groin, post-trauma scars | Most common cutaneous cyst |
Sebaceous cysts can theoretically occur anywhere except palms and soles, as sebaceous glands are absent in those areas. Epidermoid cysts occur anywhere, but favor areas with more hair follicles or regions of previous skin injury.
Clinical Presentation and Appearance
Common Features of Both Cyst Types
- Slow-growing, movable, dome-shaped lumps under the skin
- Generally painless, but may become tender or inflamed if infected or ruptured
- Surface may show a small central pore (punctum)
Distinguishing Characteristics
- Sebaceous Cyst:
- Usually has a larger, prominent central pore clogged with waxy sebum
- Contents are oily, yellow, or white sebum (skin oil)
- May be associated with overlying hair growth
- Tends to grow slowly
- Rupture is less frequent, but possible if cyst wall is compromised
- Epidermoid Cyst:
- Central punctum may be smaller, sometimes described as a “blackhead” appearance
- Contents are thick, cheesy, foul-smelling keratin (toothpaste-like)
- Feels rubbery to the touch
- Growth rate varies; can enlarge rapidly after trauma
- More prone to rupture and acute inflammation (resembles acne cysts or abscesses)
Direct Comparison Table: Sebaceous vs. Epidermoid Cyst
| Feature | Sebaceous Cyst | Epidermoid Cyst |
|---|---|---|
| Origin | Blocked sebaceous (oil) gland | Trapped epidermal cells in hair-follicle infundibulum |
| Contents | Oily sebum (yellowish) | Cheesy-white keratin debris |
| Common Sites | Scalp, face, back, behind ears | Face, trunk, neck, post-injury scars |
| Growth Speed | Generally slower | Variable; can enlarge quickly |
| Rupture Risk | Lower | Higher, leading to inflamed flare-ups |
| Recurrence Risk | Low with complete excision | Higher if cyst wall not removed |
| Best Treatment | Surgical excision including the gland | Minimal-incision or punch excision |
Diagnosis and Differential Diagnosis
Diagnosis primarily relies on clinical examination, but sometimes cyst type can only be confirmed by surgery or microscopic analysis. Key steps include:
- Assessment of location, consistency, growth pattern, and contents (if drained or ruptured)
- Inspection for a central punctum
- Evaluation for inflammation, infection, or rapid enlargement (which may require urgent care)
Other cyst-like lesions to consider in the differential diagnosis:
- Pilar (trichilemmal) cysts (often on scalp, similar to epidermoid but derived from outer root sheath of hair)
- Lipoma (benign fat tumor)
- Abscess (collection of pus due to infection)
- Dermoid cyst (congenital, contains various tissue types)
- Malignant skin lesions (rare; rapid growth or atypical features warrant biopsy)
Treatment Options
Most cysts are benign and asymptomatic; treatment may be elective unless there is pain, infection, or cosmetic concern. Key options include:
- Observation: If small and not bothersome, watchful waiting is reasonable; many cysts remain stable for years.
- Warm Compresses: Used for minor discomfort or to encourage spontaneous drainage if a cyst is close to the surface.
- Intralesional Steroids: (e.g., triamcinolone) injected to calm mild inflammation or reduce swelling without scarring.
- Surgical Excision: The gold standard for both cyst types, especially if recurrent, painful, infected, or cosmetically concerning. Complete removal of the cyst wall is necessary to prevent recurrence.
- For sebaceous cysts: excision typically includes removal of the whole gland and sac.
- For epidermoid cysts: options include minimal-incision, punch, or laser techniques with delayed wall removal—these aim to minimize scarring, especially on the face.
- Drainage (aspiration): Not recommended as a sole treatment; leaves cyst wall behind, thus high rates of relapse.
- Incision & Drainage + Antibiotics: Appropriate for acutely infected cysts; definitive excision after infection has resolved.
Home “popping” is strongly discouraged due to high recurrence, infection risk, and possible scarring.
Recurrence & Risks
- Incomplete removal of the cyst wall or gland increases recurrence risk for both types.
- Sebaceous cysts rarely recur if excised completely with the gland.
- Epidermoid cysts are more likely to recur, especially if the cyst wall is disrupted during removal or if treated only with drainage.
- Inflamed or previously ruptured cysts are harder to fully excise and thus have greater recurrence rates.
When to Seek Medical Care
- Rapid enlargement, pain, redness, or pus, which may indicate infection or abscess formation
- Persistent or recurrent cysts
- Cysts in cosmetically sensitive locations (face, neck)
- Uncertain diagnosis, rapid change in appearance, or atypical features (to rule out malignancy)
Consultation with a dermatology or surgical provider is recommended for management and to minimize cosmetic impact.
Frequently Asked Questions (FAQs)
What is the main difference between a sebaceous cyst and an epidermoid cyst?
A sebaceous cyst originates from blocked oil glands and contains sebum, while an epidermoid cyst arises from trapped skin cells and contains keratin debris. Most so-called “sebaceous cysts” are truly epidermoid cysts.
Can these cysts become cancerous?
Very rarely, but chronic, long-standing or atypical cysts can potentially undergo malignant transformation. Most cysts are benign, but rapid changes warrant professional evaluation.
Is it safe to pop or drain a cyst at home?
No; home drainage increases infection and recurrence risk. Cyst walls must be completely removed surgically for a true cure.
Will a cyst go away on its own?
Some remain stable for years, but others may enlarge or become inflamed. If the cyst is painless and not bothersome, it can sometimes be left alone under observation.
Can both cyst types occur in the same person?
Yes; individuals may have multiple cysts of either or both types during their lifetime, especially if prone to oily skin or recurrent follicular trauma.
Summary
Understanding the true difference between sebaceous and epidermoid cysts is critical for appropriate diagnosis and effective treatment. While they often appear similar, origins, contents, clinical courses, and management options differ. Epidermoid cysts are far more common and result from trapped skin cells, while true sebaceous cysts are rare and derive from oil glands. Only surgical excision of the entire cyst and, in sebaceous cysts, the gland, provides definitive cure.
Consult a dermatologist for persistent, painful, or changing lumps to ensure accurate diagnosis and prevent complications.
References
- https://www.mountcastleplasticsurgery.com/our-blog/sebaceous-cyst-vs-epidermoid-cyst-spot-the-difference-best-treatments/
- https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=85&contentid=P03392
- https://beflawlessmn.com/2022/02/13/the-difference-between-epidermoid-pilar-sebaceous-cysts/
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/e/epidermoid-cysts-of-the-skin.html
- https://www.theminorsurgerycenter.com/blog/epidermoid-vs-sebaceous-cyst
- https://www.mayoclinic.org/diseases-conditions/epidermoid-cysts/diagnosis-treatment/drc-20352706
- https://www.ncbi.nlm.nih.gov/books/NBK532310/
Read full bio of medha deb












