The Psychological Benefits of Tracking Digestive Symptoms: Enhancing Well-Being and Self-Management
A simple gut journal helps improve mood, boost confidence, and nurture mind-body balance.
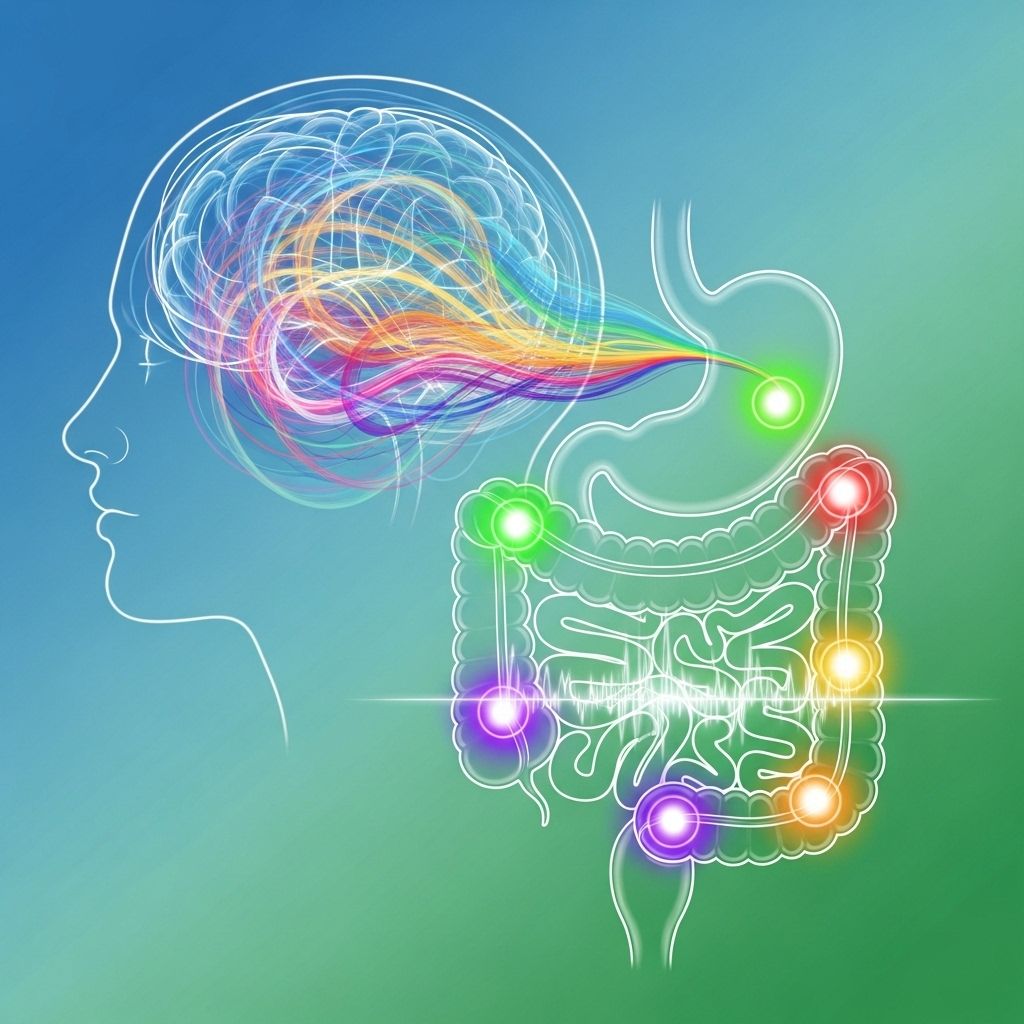
Digestive health is intricately linked to mental well-being, a connection highlighted by growing research into the gut-brain axis. While physical symptoms of digestive disorders like irritable bowel syndrome (IBS), functional dyspepsia, and inflammatory bowel disease are well-documented, the psychological dimensions often receive less attention. However, tracking digestive symptoms—whether through journaling, digital apps, or structured self-report tools—offers a powerful avenue for not only physical symptom management but also psychological benefits that enhance quality of life, build resilience, and improve overall mental health. This article explores the multifaceted psychological benefits derived from regularly tracking digestive symptoms, bridging scientific research, practical techniques, and insights into the lived experience of managing gastrointestinal health.
Table of Contents
- Introduction: The Gut–Mind Connection
- What Is Symptom Tracking?
- Key Psychological Benefits of Tracking Digestive Symptoms
- Psychological Mechanisms: How Tracking Builds Well-Being
- Practical Implementation: Best Practices
- Potential Challenges and How to Address Them
- Evidence from Research
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction: The Gut–Mind Connection
Emerging scientific understanding reveals a dynamic, bidirectional relationship between gut health and psychological well-being—a framework often called the gut-brain axis. Anxiety, depression, and stress can exacerbate gastrointestinal symptoms, while chronic digestive turmoil can negatively affect mood and daily functioning. This cyclical interplay makes management of digestive symptoms a holistic endeavor where tracking plays a pivotal role.
What Is Symptom Tracking?
Symptom tracking refers to systematically recording gastrointestinal signs and events—such as abdominal pain, bloating, bowel movements, and associated factors (diet, stress, sleep)—over time. Methods include:
- Paper journals, calendars, or notebooks
- Spreadsheets and templates
- Mobile apps and digital platforms
- Ecological momentary assessments (EMAs), which capture data frequently in real-time settings
Tracking can be daily, weekly, or incident-based, depending on goals and needs. The core aim is to gain insight by correlating symptoms with behaviors, environmental triggers, and emotional states.
Key Psychological Benefits of Tracking Digestive Symptoms
1. Enhanced Self-Awareness and Emotional Intelligence
Regular symptom tracking increases self-awareness, enabling individuals to recognize patterns between stressors, emotional states, and digestive health. This self-reflection fosters:
- Greater understanding of personal triggers and resilience factors
- Insight into the relationship between mood and gastrointestinal functioning
- Development of emotional intelligence and the ability to articulate internal experiences
Studies show that becoming aware of these connections can facilitate proactive coping and decrease feelings of helplessness or frustration often associated with digestive disorders.
2. Sense of Control and Empowerment
Digestive disorders often make individuals feel powerless. Tracking restores a sense of agency:
- Individuals can identify manageable aspects of their health (diet, activity, stress, sleep)
- Tracking supports data-driven decisions, moving from passive suffering to active engagement
- Feeling of accomplishment and incremental mastery as patterns emerge
This sense of control is associated with higher motivation, hope, and engagement in self-care behaviors.
3. Stress Reduction and Emotional Regulation
Systematically logging symptoms provides emotional outlets and structures for processing anxiety or distress:
- Writing about symptoms or challenges can reduce rumination and cognitive load
- Tracking allows for venting, journaling, and catharsis in a safe, structured way
- Links between stress and flares become clearer, helping target stress-management interventions (mindfulness, relaxation techniques)
Research indicates that psychological interventions—especially those which include stress tracking—reduce both gastrointestinal symptoms and psychological distress.
4. Feeling Understood and Validated
Digestive symptoms are often invisible or stigmatized. Objective tracking helps individuals:
- Document experiences for health professionals, leading to clearer communication and validation
- Demonstrate patterns many clinicians might otherwise miss
- Feel “seen” in sharing precise, objective reports rather than anecdotal, subjective recollections
Being heard and believed reduces isolation and fosters a sense of connection.
5. Motivation for Positive Health Behaviors
Monitoring symptoms often motivates engagement in healthy behaviors, such as exercise, better nutrition, and stress management. Individuals report:
- Positive psychological states—such as joy, contentment, or pride—when tracking leads to improvements
- Greater likelihood of making sustainable lifestyle changes
As one participant described, “I felt great that I could do more… makes you feel great that you can do more”.
6. Facilitates Shared Decision-Making and Personalized Care
Symptom records empower more collaborative, personalized medical care. Benefits include:
- Supporting informed discussions with healthcare providers
- Enabling clearer diagnosis and customized care plans
- Increasing trust and satisfaction with medical encounters
Personal data can also highlight treatment effectiveness, supporting adjustments and increasing patient buy-in.
Psychological Mechanisms: How Tracking Builds Well-Being
The psychological benefits of tracking are explained by several interrelated mechanisms:
- Cognitive restructuring: Tracking helps reframe setbacks as part of a pattern, rather than random or overwhelming crises.
- Behavioral activation: Recording behaviors and symptoms encourages regular engagement in healthy activities, disrupting cycles of avoidance.
- Enhancement of positive emotions: Correlating improvements in symptoms with positive mood reinforces self-efficacy and optimism.
- Real-time feedback: Tracking offers immediate insight and allows timely interventions before problems escalate.
Practical Implementation: Best Practices
For optimal psychological benefit, symptom tracking should be individualized and sustainable. Key recommendations include:
- Start simple: Use easy templates or apps designed for digestive health
- Track consistently, but avoid perfectionism—missed days are acceptable
- Record both physical symptoms and contextual factors (daily mood, stress level, meals, sleep)
- Review data regularly to identify meaningful patterns, not just isolated events
- Discuss records with healthcare providers to optimize care
Sample Table: Example Daily Symptom Tracker Format
| Date | Symptoms | Intensity | Mood | Diet | Stress Level | Notes |
|---|---|---|---|---|---|---|
| 10/01 | Bloating, cramping | 5/10 | Calm | High fiber | 2/10 | Morning walk helped |
Potential Challenges and How to Address Them
While tracking has many benefits, some challenges may arise:
- Obsessive focus: Excessive preoccupation with symptoms can heighten anxiety. Solution: Track at set times rather than constantly, and focus on trends, not every fluctuation.
- Time and effort: Maintaining consistency may be difficult. Solution: Use reminders and user-friendly tools to streamline recording.
- Feeling overwhelmed: If tracking highlights persistent symptoms, it can lead to discouragement. Solution: Emphasize progress, even small improvements, and seek support when needed.
Evidence from Research
Research underscores the intertwined relationship between psychological health and the management of digestive symptoms, as well as the value of self-monitoring:
- Improved Symptom Management: Psychological interventions and behavior changes informed by symptom tracking significantly improve outcomes for conditions like IBS and functional dyspepsia.
- Reduced Negative Mood: Daily monitoring, including mood diaries and EMAs, increases self-awareness and is linked to reductions in anxiety, depression, and negative emotional states.
- Data-driven Insights: Frequent self-reports increase the validity of findings, reduce recall bias, and enhance the reliability of self-observation, making symptom tracking a robust tool not only for clinical care but also for personal development.
- Increased Positive Emotions: Study participants note feeling calm, proud, or enthusiastic when improvements are noted or new healthy routines established.
Frequently Asked Questions (FAQs)
Q: Can tracking digestive symptoms increase anxiety or stress?
A: While some may be initially concerned about focusing on symptoms, most evidence indicates that purposeful, structured tracking reduces anxiety, enhances coping, and provides reassurance—especially when combined with emotional monitoring and supportive therapy.
Q: What is the best way to start symptom tracking?
A: Start with simple tools—a paper journal, calendar, or a specialized mobile app. Record main symptoms, meal details, emotional state, and any notable events or triggers. Consistency is more important than detail.
Q: How does tracking help during medical visits?
A: Symptom logs provide precise, objective information for clinicians, supporting faster diagnosis, tailored treatment plans, and more productive discussions. Sharing data also validates patient concerns and promotes collaborative care.
Q: Are there psychological therapies that combine symptom tracking?
A: Yes. Cognitive-behavioral therapy, mindfulness-based stress reduction, and other interventions frequently encourage self-monitoring to build self-efficacy and track both emotional and physical responses to treatment.
Q: Can tracking symptoms improve my overall happiness or sense of fulfillment?
A: Research consistently shows that positive psychological constructs such as calm, gratitude, pride, and connection increase as individuals gain insight, self-control, and motivation through active symptom management.
Conclusion
Tracking digestive symptoms is much more than a clinical exercise; it offers a pathway to greater psychological well-being, improved emotional regulation, and empowered self-management. By fostering self-awareness, promoting a sense of agency, supporting mental health interventions, and deepening the partnership between patients and providers, tracking transforms digestive health management into an active, hopeful, and fulfilling process. As research continues to support these psychological advantages, incorporating structured symptom tracking should be seen as a core component of both digestive and mental health care strategies.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10033392/
- https://www.frontiersin.org/journals/gastroenterology/articles/10.3389/fgstr.2024.1342888/full
- https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2022.827220/full
- https://www.nature.com/articles/s44184-025-00123-z
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10237074/
- https://oshihealth.com/the-inextricable-link-between-mental-health-and-gi-symptoms/
- https://cdhf.ca/en/gut-health-and-mental-health-alleviating-anxiety-symptoms/
Read full bio of medha deb












