Probiotic Strains for Helicobacter pylori (H. pylori): Efficacy, Mechanisms, and Clinical Perspectives
Selected live cultures can ease digestive discomfort and help restore gut balance.
Helicobacter pylori (H. pylori) remains one of the most prevalent chronic bacterial infections worldwide, implicated in gastritis, peptic ulcer disease, and even gastric cancer. With conventional triple or quadruple antibiotic therapies being challenged by growing resistance and adverse gastrointestinal effects, probiotics have garnered increasing attention as a potential adjunct or alternative.
Table of Contents
- Understanding Helicobacter pylori Infection
- Role of Probiotics in H. pylori Management
- Mechanisms of Action: How Probiotics Affect H. pylori
- Key Probiotic Strains Used Against H. pylori
- Clinical Evidence: Efficacy and Limitations
- Advantages and Disadvantages of Probiotic Therapy
- Optimal Usage: Strain Selection, Dosage, and Duration
- Future Directions and Unresolved Questions
- Frequently Asked Questions (FAQs)
Understanding Helicobacter pylori Infection
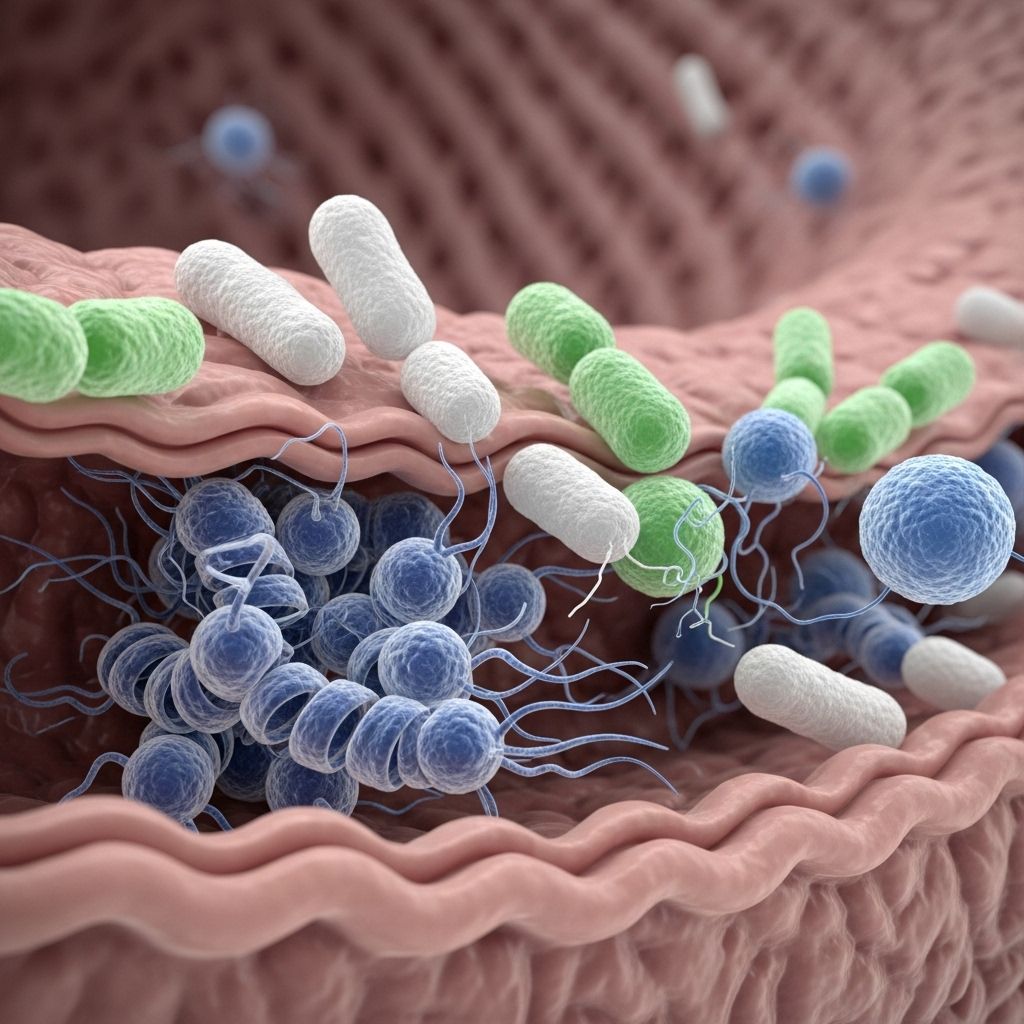
Helicobacter pylori is a spiral-shaped, Gram-negative bacterium that colonizes the gastric mucosa of over 50% of the world population. Its presence is strongly associated with chronic gastritis, peptic ulcers, mucosa-associated lymphoid tissue (MALT) lymphoma, and gastric adenocarcinoma.
- Transmission: Oral-oral or fecal-oral routes, often during childhood.
- Pathogenesis: H. pyloris urease breaks down urea to ammonia, neutralizing stomach acid and allowing bacterial survival and colonization. Chronic inflammation ensues, damaging the mucosa.
- Standard Treatment: Triple/quadruple antibiotic regimens, usually including a proton pump inhibitor (PPI) plus two or more antibiotics.
- Challenges: Rising antibiotic resistance, frequent relapse, and adverse side effects such as diarrhea and dysbiosis.
Role of Probiotics in H. pylori Management
Probiotics are live microorganisms that, when administered in adequate amounts, confer health benefits to the host. Their evolving use in H. pylori management focuses on disrupting infection, bolstering gut health, and mitigating therapy-related side effects.
- Probiotics modulate the gastrointestinal microbiome, potentially restoring balance disrupted by infection or antibiotics.
- Clinical evidence suggests certain strains can reduce H. pylori colonization, decrease infection severity, and improve eradication rates when combined with standard therapy.
- Additional benefits include the alleviation of therapy-associated adverse effects such as antibiotic-associated diarrhea.
Mechanisms of Action: How Probiotics Affect H. pylori
Several mechanisms underpin the anti-H. pylori effects of specific probiotic strains:
- Competition for adhesion sites: Probiotics compete with H. pylori for mucosal epithelial binding, effectively displacing the pathogen.
- Secretion of antimicrobial substances: Certain lactobacilli and bifidobacteria produce organic acids, bacteriocins, and hydrogen peroxide that inhibit H. pylori growth.
- Immune modulation: Probiotics modulate mucosal and systemic immunity, promoting anti-inflammatory responses and strengthening the gastric mucosal barrier.
- Restoration of microbial diversity: Supplementation restores and maintains a healthy, diverse intestinal microbiota, which is otherwise perturbed during infection and antibiotic therapy.
- Suppression of urease activity: Evidence shows that selected probiotics can reduce H. pylori urease activity, lowering its pathogenic potential.
Key Probiotic Strains Used Against H. pylori
Not all probiotics are equally effective against H. pylori. The following strains have demonstrated the most promise in clinical and preclinical studies:
| Probiotic Strain | Mechanism | Clinical Benefit Noted |
|---|---|---|
| Lactobacillus reuteri | Produces antimicrobial reuterin; strengthens mucosal barrier; reduces urease activity | Reduced H. pylori colonization and improved GI symptoms in clinical trials |
| Lactobacillus casei | Competes for adhesion sites; modulates immune responses | Enhances eradication rates, decreases adverse drug reactions |
| Lactobacillus rhamnosus GG | Promotes mucosal integrity; antagonizes pathogen binding | Alleviates gastrointestinal symptoms, supports gut flora |
| Bifidobacterium bifidum & B. lactis | Protects against mucosal damage; anti-inflammatory | Reduces infection-associated inflammation, possibly lowers colonization |
| Saccharomyces boulardii | Non-pathogenic yeast; restores microbiota following antibiotics | Reduces diarrhea and gut dysbiosis during eradication therapy |
Combination formulations containing two or more genera (e.g., Lactobacillus plus Bifidobacterium) are under investigation for synergistic effects.
Clinical Evidence: Efficacy and Limitations
Clinical trials and meta-analyses provide a growing, though still mixed, body of evidence regarding the value of probiotics for H. pylori infection management.
- Randomized studies confirm that probiotics, when added to antibiotic regimens, raise eradication rates by 5-10% compared with antibiotics alone.
- Gastrointestinal side effects—notably diarrhea, nausea, and bloating—are significantly reduced in patients receiving probiotics as adjuvant therapy.
- In a major multicenter study, a regimen with four different probiotic strains combined with standard therapy achieved a 92% eradication rate versus 86.8% with standard treatment alone. New-onset side effects were also markedly lower (17% versus 50.7%).
- Some studies do not show a significant difference in eradication rates, but most report symptomatic relief and better tolerance to medication.
- The choice of strain, dosing, patient demographic, and geographic variation all play critical roles in probiotic efficacy.
Summary Table: Probiotics as Adjuvant in H. pylori Eradication Therapy
| Outcome | With Probiotics | Without Probiotics |
|---|---|---|
| H. pylori Eradication Rate | Up to 92% | Up to 87% |
| Incidence of Side Effects | 17% | 51% |
| Antibiotic-Associated Diarrhea | Significantly decreased | Typical |
Limitations of the Evidence
- Most studies lack standardization of probiotic strains, doses, and duration.
- Many clinical trials include limited sample sizes, often in Asian populations, requiring caution with generalization.
- Some conflicting results in meta-analyses regarding eradication efficacy; consensus statements (e.g., Maastricht VI/Florence) do not currently endorse routine use in all patients.
- Side effects are rare, but severe infections such as fungemia and bacterial sepsis have been reported in immunocompromised patients.
Advantages and Disadvantages of Probiotic Therapy
| Advantages | Disadvantages |
|---|---|
|
|
Optimal Usage: Strain Selection, Dosage, and Duration
Key considerations for effective probiotic use against H. pylori:
- Strain Selection: Not all probiotics are created equal. Lactobacillus reuteri, L. casei, L. rhamnosus GG, Bifidobacterium bifidum, and S. boulardii are the most researched and effective options.
- Dosage: Dosages employed in studies range widely (from 108 to 1010 CFU/day); optimal doses may vary based on the specific strain and formulation.
- Duration: Most protocols suggest starting probiotics alongside eradication therapy and continuing for at least 4–6 weeks to optimize benefits.
- Formulations: Both single-strain and multi-strain products are used, though combination therapies may offer added efficacy.
Future Directions and Unresolved Questions
Research into probiotics for H. pylori treatment is ongoing, with several key areas requiring further study:
- Identification and validation of gastric-acid-resistant probiotic strains capable of sustained colonization and inhibition in the stomach.
- Large-scale, multicenter, randomized controlled trials across diverse populations to confirm efficacy and safety.
- Defining the optimal combination and duration of probiotic use for differing patient risk profiles (children, elderly, immunocompromised).
- Development of engineered or autologous probiotics customized to the patient’s own gastric microbiome.
- Clarification of precise molecular mechanisms by which probiotics modulate H. pylori and the human host.
Current expert consensus does not recommend routine probiotic therapy for all patients with H. pylori, though use is favored in those at high risk for antibiotic-associated side effects or relapse.
Frequently Asked Questions (FAQs)
Q: What are the most effective probiotic strains for H. pylori eradication?
A: Lactobacillus reuteri, L. casei, L. rhamnosus GG, Bifidobacterium bifidum, and Saccharomyces boulardii have shown the most clinical promise in improving eradication rates and reducing side effects.
Q: Can probiotics replace antibiotics for H. pylori infection?
A: No. Probiotics are adjuncts and cannot replace antibiotics as primary therapy for H. pylori infection. They are most effective when used in combination with standard eradication regimens.
Q: Are probiotics safe in all patients?
A: Probiotics have a strong safety profile in the general population but may pose risks in immunocompromised individuals or those with severe underlying diseases. Consultation with a healthcare provider is recommended.
Q: Do all probiotics work the same for H. pylori?
A: No. Only specific strains demonstrate anti-H. pylori activity. Product labels should be checked for strain specificity (e.g., L. reuteri DSM 17938).
Q: What is the best way to take probiotics for H. pylori?
A: As part of a daily regimen begun with H. pylori eradication therapy and continued for at least 4–6 weeks, using strains and doses shown to have clinical efficacy.
References
Read full bio of medha deb












