Prebiotic Fiber Applications in SIBO: Enhancing Gut Barrier Support and Microbiota Health
Gentle, personalized dietary strategies pave the way to stronger gut barrier function.
Prebiotic Fiber Applications in SIBO for Barrier Support
Small Intestinal Bacterial Overgrowth (SIBO) presents unique challenges in clinical management, particularly concerning the delicate balance required to restore intestinal health without worsening symptoms. This comprehensive article examines the science and practical approaches to prebiotic fiber use for barrier support in SIBO, integrating insights from clinical studies, expert commentary, and novel nutritional strategies.
- Table of Contents
- Introduction: SIBO and the Gut Barrier
- The Role of Prebiotic Fiber in Gut Health
- Challenges of Using Prebiotics in SIBO
- Types of Prebiotic Fiber and Their Impact in SIBO
- Novel Non-Fiber Prebiotics for SIBO
- Clinical Strategies for Safe Use of Prebiotics
- Current Research Evidence
- Dietary Approaches and Gradual Microbiota Restoration
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction: SIBO and the Gut Barrier
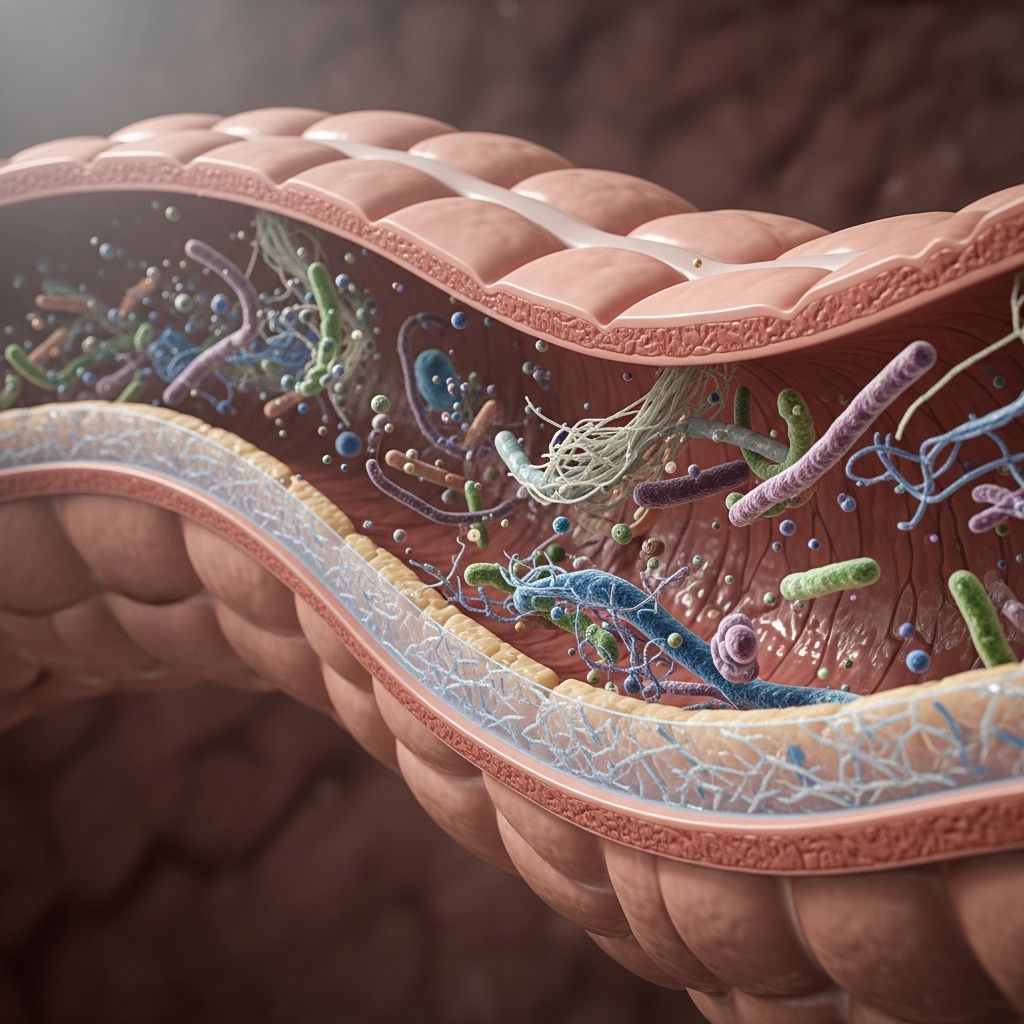
SIBO is characterized by excessive or altered bacterial populations in the small intestine, often resulting in symptoms such as bloating, gas, abdominal discomfort, diarrhea, and nutrient malabsorption. The integrity of the intestinal barrier, maintained by the mucosal lining and tight junctions between epithelial cells, is critical for preventing the passage of pathogens and toxins, supporting immune defense, and facilitating nutrient absorption. Disruptions to the barrier due to inflammation or bacterial overgrowth can exacerbate digestive symptoms and long-term health risks.
The Role of Prebiotic Fiber in Gut Health
Prebiotic fibers are nondigestible food components—most commonly specific carbohydrates and fibers—which selectively promote the growth of beneficial gut bacteria, such as Bifidobacterium and Lactobacillus. Their fermentation in the colon produces short-chain fatty acids (SCFAs), including butyrate, which play essential roles in nourishing colonocytes, regulating immune functions, and strengthening the intestinal barrier.
- Promotion of Diverse Microbiota: Prebiotics foster a diverse milieu of bacterial species, enhancing resilience against pathogens and supporting metabolic functions.
- Barrier Integrity Enhancement: By feeding beneficial microbes and stimulating SCFA production, prebiotics directly strengthen the epithelial layer and tight junction proteins.
- Anti-inflammatory Effects: Butyrate and other SCFAs modulate inflammation and immune signaling both locally and systemically.
Challenges of Using Prebiotics in SIBO
Despite these benefits, the application of prebiotic fibers in SIBO is complicated by several risks and mechanisms unique to the condition:
- Symptom Exacerbation: The fermentation of fiber by both beneficial and pathogenic bacteria can lead to increased gas, bloating, and discomfort.
- Bacterial Overfeeding: Traditional fermentable fibers may “overfeed” resident bacteria—beneficial and otherwise—potentially worsening bacterial overgrowth.
- Acute Flare Risk: In active SIBO, introducing prebiotics can trigger acute symptom flares if not managed properly.
- Diminished Barrier Support: Paradoxically, fear of fiber leads many SIBO patients to avoid prebiotics altogether, which can compromise gut barrier integrity and nutrient intake in the long term.
Types of Prebiotic Fiber and Their Impact in SIBO
Not all prebiotics are nutritionally or clinically equivalent, especially in the context of SIBO. Selection depends on fiber type, fermentability, and individual tolerance:
| Type | Fermentation Properties | Gut Barrier Impact | SIBO Tolerance |
|---|---|---|---|
| Inulin | Highly fermentable | Strong SCFA producer | Poor; may worsen symptoms if introduced too early |
| Fructo-oligosaccharides (FOS) | Moderately fermentable | Supports bifidobacteria; moderate SCFA output | Variable; caution required, better post-eradication |
| Guar gum | Fermentable but slow | Promotes barrier integrity, anti-inflammatory | Potentially tolerable in small doses |
| Polyphenols (e.g. citrus, pomegranate extract) | Non-fiber, non-gas producing | Protects mucosal barrier, modulates immunity | High; less risk of bloating/flare |
| Low-FODMAP fibers | Minimally fermentable | Reduced SCFA but greater tolerability | Good for initial gut support |
Key Insights
- Even low doses of fermentable fibers can trigger symptoms during active SIBO and should only be considered after bacterial overgrowth is controlled.
- Non-fiber prebiotics (flavonoid-rich polyphenols) provide a promising avenue to support barrier integrity without provoking excessive gas.
- Gradual and individualized introduction is vital for safe gut restoration.
Novel Non-Fiber Prebiotics for SIBO
Recent clinical interest has focused on citrus-based polyphenolic prebiotics and similar non-fiber options. These compounds:
- Promote healthy gut microbiota composition by selectively stimulating beneficial bacteria.
- Protect and repair the gut mucosal barrier via antioxidant and immunomodulatory effects.
- Minimize fermentation-induced gas production, reducing SIBO symptoms.
- Support epithelial cell nourishment and increase host resilience to bacterial translocation and local inflammation.
- Biofilm disruption: Pomegranate extract, for example, is recognized for breaking down bacterial biofilms, contributing to bacterial clearance and improved barrier function.
This approach is especially valuable for patients who cannot tolerate standard fiber-based prebiotics.
Clinical Strategies for Safe Use of Prebiotics
- Phased Introduction: Begin with eradication (antibiotics/probiotics), then slowly reintroduce selected prebiotic fibers.
- Professional Supervision: Individual tolerance, medical history, and symptom tracking should guide prebiotic therapy. Self-experimentation is discouraged.
- Low-FODMAP Prebiotic Guidance: Using fibers with minimal fermentability is safer for initial support. Guar gum and low-FODMAP carbohydrates are often recommended.
- Synergy with Probiotics: Combining select prebiotics with probiotics (i.e. synbiotics) improves outcomes, particularly in restoring microbiota balance post-antibiotic treatment.
- Polyphenol-Based Supplements: Consider non-fiber alternatives for high-risk or sensitive patients (citrus, pomegranate extracts).
- Symptom-Based Dosing: Dose titration should correlate with symptom relief, not standards for healthy individuals.
Current Research Evidence
- A randomized, controlled study found that combining a synbiotic (probiotic plus prebiotic FOS) with standard antibiotic therapy resulted in greater symptom reduction and improvements in hydrogen breath test markers compared to antibiotics alone, although eradication rates were not significantly different.
- Comprehensive reviews highlight the importance of strain selection in probiotic supplementation and the potential for prebiotics, postbiotics, and synbiotics in clinical management.
- A meta-analysis of clinical trials showed that probiotics are generally beneficial for SIBO management, suggesting a similar rationale for safe, targeted prebiotic use.
- Conflicting evidence remains, especially regarding the timing and choice of prebiotic fibers. Some sources advocate stricter avoidance in the initial eradication phase, while others favor cautious, phased inclusion during the recovery period.
Dietary Approaches and Gradual Microbiota Restoration
Many SIBO patients extensively restrict fiber and prebiotic foods, risking long-term depletion of the healthy gut microbiota and nutritional deficiencies. A sustainable recovery strategy involves:
- Low-FODMAP Dietary Patterns: Initially limiting highly fermentable fibers while incorporating tolerated prebiotics and slowly increasing diversity post-eradication.
- Targeted Foods: Amazonian superfoods such as açaí, cupuaçu, Brazil nuts, and selected inulin sources (used at low doses post-eradication) may safely promote microbiota regeneration, motility, and barrier support.
- Essential Nutrient Supplementation: L-glutamine and micronutrients are frequently used alongside limited prebiotics for epithelial repair.
- Monitoring and Adjustment: Diet should be regularly evaluated with professional input, adapting strategies according to symptoms, functional tests, and microbiota profile.
Frequently Asked Questions (FAQs)
Q: Should fiber and prebiotics always be avoided during SIBO treatment?
A: Not always. While fermentable fibers can worsen symptoms during active bacterial overgrowth, safe, gradual reintroduction of certain prebiotics—under medical supervision—helps restore microbiota and barrier function after initial eradication.
Q: What kind of prebiotic is best tolerated during SIBO?
A: Non-fiber prebiotics, such as polyphenol-rich citrus extracts and pomegranate, are generally better tolerated, supporting barrier integrity while minimizing gas and bloating. Guar gum and low-FODMAP fibers may be cautiously used post-eradication.
Q: Can prebiotics replace antibiotics or probiotics in SIBO management?
A: No, prebiotics do not eradicate bacterial overgrowth. Antibiotics remain the mainstay for active SIBO, with probiotics and selected prebiotics playing supportive roles during recovery and barrier re-establishment.
Q: Are there risks to avoiding all prebiotics and fiber in SIBO?
A: Yes. Extended avoidance leads to microbiota depletion, impaired barrier integrity, and increased risk of nutrient deficiencies. Gradual, individualized introduction of safe prebiotic sources is critical for long-term recovery.
Q: How should I introduce prebiotic fiber if I have SIBO?
A: Only after controlling bacterial overgrowth. Start with non-fiber or low-FODMAP options in low doses and increase slowly while monitoring symptoms. Always seek professional guidance.
Conclusion
Prebiotic fiber applications in SIBO require evidence-based, individualized strategies balancing symptom avoidance and long-term barrier support. Carefully selected prebiotics—including novel polyphenol-based compounds—combined with phased dietary introduction, professional supervision, and synergy with probiotics, deliver promising outcomes for restoration of microbiota, nutritional status, and gut barrier integrity. Avoidance is rarely sustainable; instead, a gradual, science-guided approach is key to resilient, recovered intestinal health.
References
- https://www.mahta.bio/en/blogs/mahta/uso-de-probioticos-e-prebioticos-no-sibo-quando-como-e-por-que
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4311309/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11768010/
- https://www.drhagmeyer.com/which-prebiotics-are-best-for-sibo/
- https://seed.com/cultured/probiotics-sibo-treatment-research-guide/
- https://www.usenourish.com/blog/sibo-natural-treatment
- https://www.gutmicrobiotaforhealth.com/certainties-and-uncertainties-of-sibo/
Read full bio of Sneha Tete












