Poor Dental Health & Facial Circulation Connection: Risks, Mechanisms, and Prevention
Healthy gums help prevent inflammation and support better blood flow from face to heart.
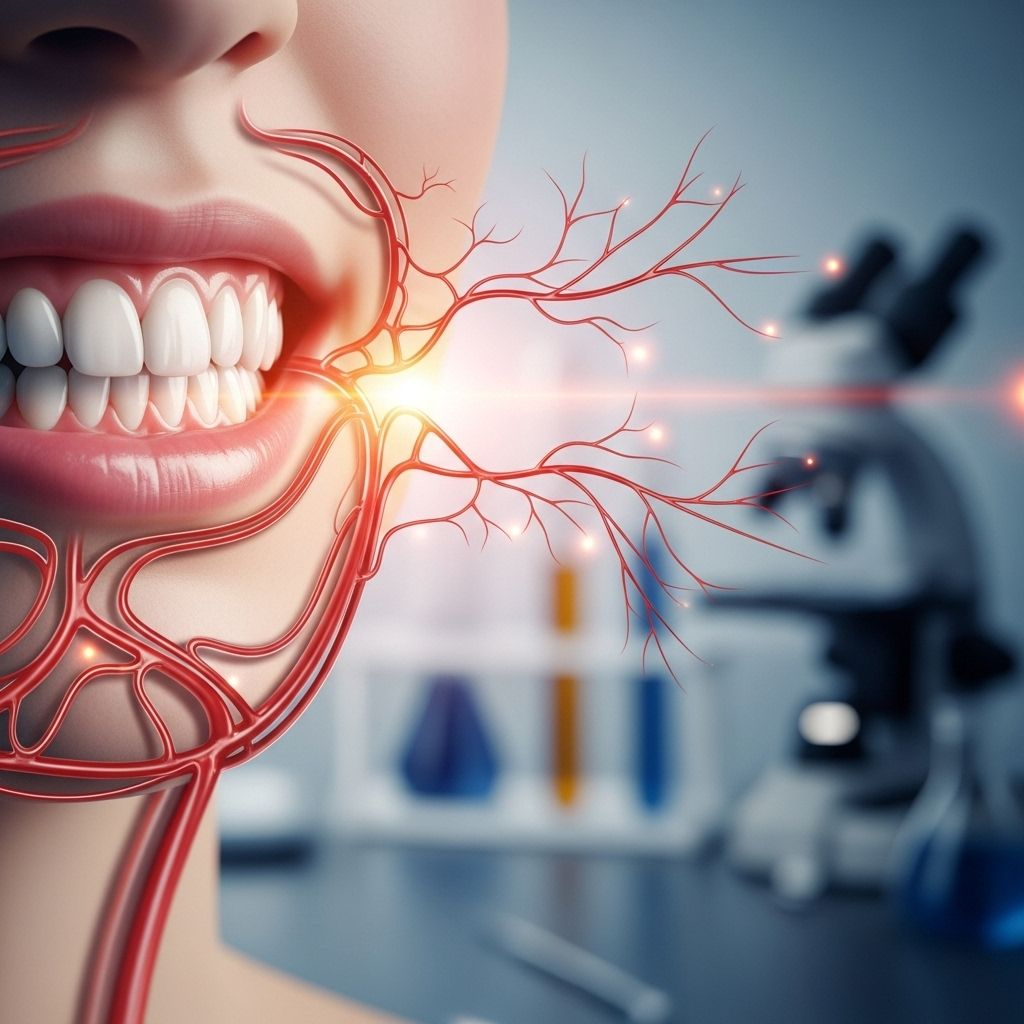
Table of Contents
- Introduction
- The Mouth-Body Connection: An Overview
- Oral Health and Its Influence on Facial Circulation
- Mechanisms: How Poor Oral Health Affects Circulation
- Periodontal Disease and Cardiovascular Risk
- Tooth Loss and Its Systemic Impact
- Clinical Evidence Supporting the Dental-Circulatory Link
- Risk Factors and Vulnerable Populations
- Prevention and Management Strategies
- Frequently Asked Questions
- Conclusion
Introduction
Oral health is more than just cavities and gum disease—it is a window to your overall well-being. Recent research highlights a significant connection between poor dental health and compromised facial, as well as systemic, circulation, with profound implications for cardiovascular health and general longevity. This article delves into the scientific evidence, mechanisms, risk factors, and preventive measures surrounding the relationship between dental health and circulation, particularly focusing on the face and cardiovascular system.
The Mouth-Body Connection: An Overview
The mouth is the gateway to the body, and its health reflects and influences systemic conditions. Poor oral hygiene can lead to periodontitis (gum disease), tooth decay, and tooth loss—each of which has been linked to increased inflammation, infection, and a higher risk of chronic diseases, especially cardiovascular diseases (CVD).
Inflammation and bacteria from gum infections can enter the bloodstream, traveling to distant organs and tissues, including the heart and blood vessels. This systemic spread of oral pathogens and inflammatory mediators can contribute to the development and progression of atherosclerosis (hardening and narrowing of the arteries), increasing the risk of heart attacks, strokes, and other circulatory complications.
Oral Health and Its Influence on Facial Circulation
The face is richly vascularized, with a complex network of arteries and veins supplying oxygen and nutrients to facial tissues. Healthy circulation in the face is essential for tissue vitality, wound healing, and overall appearance. However, chronic oral infections and inflammation can impair local blood flow in facial tissues, leading to delayed healing, tissue breakdown, and increased susceptibility to infection and disease.
- Local Effects: Oral infections can cause localized swelling, pain, and redness, all signs of compromised circulation and increased vascular permeability.
- Systemic Effects: The inflammation and bacteria from oral diseases can enter the systemic circulation, affecting distant blood vessels and organs.
- Visible Signs: Over time, chronic poor oral health may manifest as pallor, delayed wound healing, or even necrosis in severe cases.
Mechanisms: How Poor Oral Health Affects Circulation
Several mechanisms have been proposed to explain how poor dental health impacts both facial and systemic circulation:
- Bacteremia and Inflammation: Periodontal pathogens can enter the bloodstream, especially during chewing, brushing, or dental procedures, leading to bacteremia. These bacteria and their byproducts trigger systemic inflammation, which can damage blood vessel linings and promote atherosclerosis.
- Inflammatory Mediators: Cytokines and other inflammatory molecules released during chronic gum disease can circulate throughout the body, causing endothelial dysfunction, oxidative stress, and arterial stiffness.
- Plaque Formation: Oral bacteria may directly contribute to the formation of arterial plaques, narrowing blood vessels and reducing blood flow to facial and other tissues.
- Thrombus Formation: Chronic oral inflammation can increase the risk of blood clot formation, further compromising circulation.
Periodontal Disease and Cardiovascular Risk
Periodontal disease, a chronic inflammatory condition of the gums and supporting structures of the teeth, has been consistently associated with an increased risk of cardiovascular diseases. The table below summarizes key findings from recent studies:
| Study/Country | Intervention | Outcome |
|---|---|---|
| Pakistan RCT | Non-surgical periodontal therapy | Reduced C-reactive protein, fibrinogen, white blood cells |
| Brazil RCT | Non-surgical periodontal therapy | Reduced inflammatory markers, total cholesterol, triglycerides |
| India Case-Control | Surgical periodontal therapy | Decreased C-reactive proteins |
| Netherlands, China, Brazil | Surgical & non-surgical therapy | Improved blood pressure, lipid profile, inflammatory markers |
Periodontal therapy—whether surgical or non-surgical—has shown to reduce cardiovascular risk markers, suggesting that managing gum disease can have systemic benefits beyond the mouth. However, while the evidence is promising, more extensive and long-term studies are needed to establish causality and define optimal treatment protocols.
Tooth Loss and Its Systemic Impact
Tooth loss is often the end result of untreated dental caries and periodontal disease. Studies have found that both partial and complete tooth loss are associated with increased all-cause, cardiovascular, and respiratory mortality. Potential pathways include:
- Dietary Compromise: Missing teeth can lead to chewing difficulties, resulting in poor nutrition and further health decline.
- Chronic Inflammation: Tooth loss is a marker of chronic oral inflammation, which can perpetuate systemic inflammation and vascular damage.
- Biofilm and Infection: Dental biofilm from infected teeth can release bacteria and inflammatory mediators into the bloodstream, affecting distant organs.
In large cohort studies, periodontal disease has been independently associated with increased cardiovascular mortality, even after adjusting for other risk factors. This underscores the importance of preserving natural teeth and maintaining good oral hygiene throughout life.
Clinical Evidence Supporting the Dental-Circulatory Link
A systematic review of 2,154 studies identified 12 that met rigorous inclusion criteria, all demonstrating that periodontal therapy and regular oral hygiene (brushing, flossing, professional cleanings) significantly reduce cardiovascular risk markers and mortality. Improvements in inflammatory markers (e.g., C-reactive protein), lipid profiles, and blood pressure were consistently observed following oral health interventions.
However, the evidence regarding the direct therapeutic effect of oral health promotion on cardiovascular disease outcomes remains limited, pointing to the need for further research. Nevertheless, the underlying biological mechanisms—chronic inflammation, bacteremia, endothelial dysfunction—provide a plausible explanation for the observed associations.
Risk Factors and Vulnerable Populations
Not everyone with poor oral health will develop circulatory problems. Individual susceptibility depends on a combination of factors:
- Overall Health: People with underlying chronic diseases (e.g., diabetes, hypertension) are more vulnerable to the systemic effects of oral infections.
- Immune Status: Those with weakened immune systems are at higher risk for complications from oral bacteria entering the bloodstream.
- Genetics and Lifestyle: Genetic predisposition, smoking, poor diet, and lack of exercise can exacerbate the risks associated with poor oral health.
- Age: Older adults, who often experience cumulative oral health problems and tooth loss, face higher risks of circulatory and mortality outcomes.
Prevention and Management Strategies
Maintaining good oral health is a cornerstone of circulatory and overall health. Key strategies include:
- Regular Oral Hygiene: Brush twice daily, floss, and use antimicrobial mouthwash to reduce bacterial load and inflammation.
- Professional Dental Care: Schedule regular dental check-ups and cleanings to detect and treat gum disease early.
- Periodontal Therapy: For those with gum disease, non-surgical or surgical treatments can reduce systemic inflammation and cardiovascular risk.
- Healthy Lifestyle: Avoid smoking, eat a balanced diet, exercise regularly, and manage chronic diseases to mitigate overall risk.
- Education and Awareness: Public health campaigns should emphasize the mouth-body connection to encourage preventive behaviors.
Frequently Asked Questions
Q: How does gum disease affect heart health?
A: Gum disease causes chronic inflammation and allows harmful bacteria to enter the bloodstream, contributing to atherosclerosis, arterial stiffness, and increased risk of heart attack and stroke.
Q: Can improving my oral hygiene reduce my risk of cardiovascular disease?
A: Yes, regular brushing, flossing, and professional dental care can lower inflammation and cardiovascular risk markers, potentially reducing the likelihood of heart disease.
Q: Is tooth loss linked to higher mortality?
A: Studies show that both partial and complete tooth loss are associated with increased all-cause and cardiovascular mortality, likely due to chronic inflammation and dietary compromise.
Q: Who is most at risk for circulatory problems due to poor oral health?
A: Individuals with chronic diseases, weakened immune systems, poor lifestyle habits, and older adults are at higher risk.
Q: What are the signs that poor oral health is affecting my circulation?
A: Look for persistent gum inflammation, bleeding, tooth mobility, delayed healing, and systemic symptoms like unexplained fatigue or chest pain.
Conclusion
The connection between poor dental health and compromised facial and systemic circulation is supported by growing scientific evidence. Chronic oral infections, particularly periodontal disease, can lead to systemic inflammation, endothelial dysfunction, and increased cardiovascular risk. Tooth loss further amplifies these risks through dietary and inflammatory pathways. While more research is needed to establish direct causality and optimal interventions, the current evidence strongly supports the importance of maintaining good oral hygiene as part of a comprehensive approach to circulatory and overall health. Regular dental care, healthy lifestyle choices, and increased public awareness are essential to breaking the cycle of oral-systemic disease and promoting longevity and well-being.
References
- https://www.frontiersin.org/journals/oral-health/articles/10.3389/froh.2024.1364765/full
- https://www.starbritedentalrockville.com/the-mouth-body-connection-the-importance-of-better-dental-health
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8361186/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11731113/
- https://www.docseducation.com/blog/new-study-shows-link-between-oral-health-fibromyalgia-and-migraines
- https://www.bumrungrad.com/en/health-blog/september-2023/the-link-between-oral-hygiene-and-heart-health
Read full bio of Sneha Tete












