Pharmaceuticals Affecting Cutaneous Blood Flow: Comprehensive Mechanisms and Clinical Implications
In-depth look at how drugs influence skin circulation and impact therapeutic strategies.
Pharmaceuticals Affecting Cutaneous Blood Flow: A Review
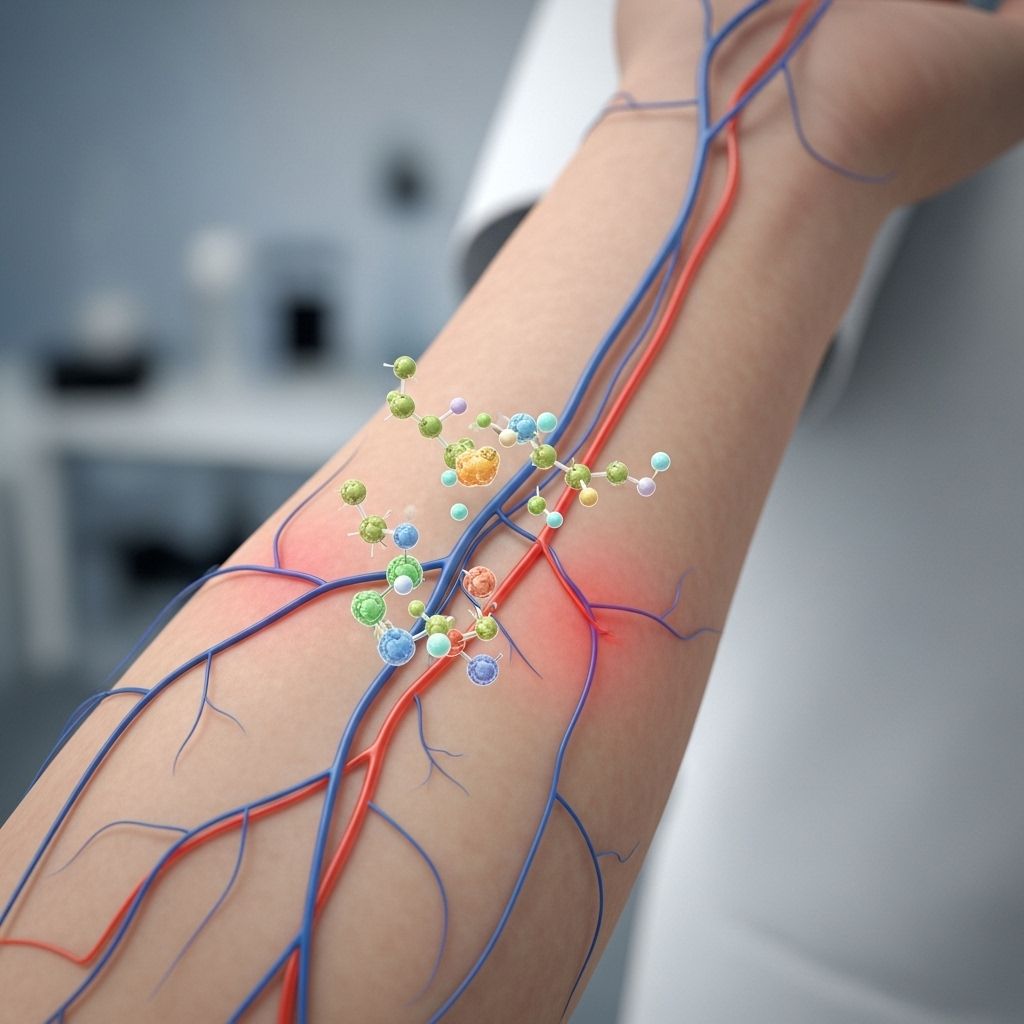
Cutaneous blood flow plays a vital role in thermoregulation, drug delivery, immune responses, and overall skin health. Pharmaceutical agents can profoundly modulate the skin’s microcirculation through direct and indirect mechanisms, influencing therapeutic outcomes, side effects, and clinical decisions. This comprehensive review examines the principal classes of drugs affecting cutaneous blood flow, underlying biological mechanisms, clinical implications, and current research directions.
Table of Contents
- Introduction to Cutaneous Blood Flow Regulation
- Physiological and Pharmacological Mechanisms
- Pharmaceutical Vasodilators
- Pharmaceutical Vasoconstrictors
- Neurotransmitter Mediation and Central Modulation
- Drugs with Predominant Local Effects
- Implications for Transdermal Drug Delivery
- Clinical Implications of Drug-Induced Cutaneous Blood Flow Changes
- Future Directions in Research
- Frequently Asked Questions (FAQs)
Introduction to Cutaneous Blood Flow Regulation
The skin’s microvascular circulation represents 5-10% of total cardiac output and is essential for maintaining thermal balance, nourishing tissues, and supporting immune function. Cutaneous blood flow is dynamically regulated by the sympathetic nervous system, local metabolic factors, temperature, and circulating substances such as hormones and drugs. Disruptions in this balance may lead to clinical phenomena like erythema, pallor, altered wound healing, or enhanced or reduced drug absorption through the skin.
Physiological and Pharmacological Mechanisms
- Sympathetic Nervous System: Most cutaneous vessels receive dense sympathetic innervation, which mediates vasoconstriction via norepinephrine and alpha-adrenergic receptor activation. Parasympathetic influence is limited.
- Endothelial Mediators: Nitric oxide (NO), prostacyclin, and endothelin-1 locally regulate vasomotor tone, often as a response to shear stress or circulating chemicals.
- Neurotransmitters and Neuropeptides: Serotonin (5-HT), acetylcholine, substance P, and others can modulate vascular tone through direct receptor interactions on smooth muscle or endothelium.
- Indirect Modulators: Systemic diseases, temperature changes, and psychological stimuli (stress, fear) can secondarily alter cutaneous blood flow via neurohormonal pathways.
Pharmaceutical Vasodilators
Various drug classes promote vasodilation (widening of blood vessels) within the skin, enhancing blood flow and modulating physiological or therapeutic effects. Key vasodilators include:
- Nicotinates and Alkyl Nicotinates: Topical agents like benzyl nicotinate induce local erythema and warming by promoting vasodilation. These are commonly used in topical rubefacients and for diagnostic skin testing. Application leads to a rapid and significant increase in cutaneous blood flow, as measured by laser Doppler velocimetry, often accompanied by increased skin temperature and redness.
- Nitrates and Nitroglycerin: Act as nitric oxide donors, causing smooth muscle relaxation in arterial and venous vessels. Used in transdermal patches for angina pectoris, they can cause local flushing at the patch site due to microvascular dilation.
- Alpha-Adrenergic Antagonists: Drugs blocking alpha receptors (e.g., prazosin, phentolamine) reduce baseline sympathetic vasoconstrictor tone, producing net vasodilation and increased skin blood flow.
- Calcium Channel Blockers: Systemic agents (e.g., nifedipine, amlodipine) reduce intracellular calcium in vascular smooth muscle, resulting in relaxation and cutaneous flushing, especially with dihydropyridines.
- Phosphodiesterase Inhibitors: By preventing cyclic AMP/cGMP degradation, drugs like sildenafil and topical PDE4 inhibitors increase NO-mediated vasodilation.
Some commonly used vasodilators and their application modes:
| Drug/Class | Mode of Administration | Clinical/Cosmetic Indication |
|---|---|---|
| Benzyl nicotinate | Topical | Rubefacient, microcirculation assessment |
| Nitroglycerin | Transdermal | Angina, heart failure |
| Nifedipine | Oral/topical | Raynaud’s, hypertension |
| Prazosin | Oral | Hypertension, PTSD |
Pharmaceutical Vasoconstrictors
Some drugs decrease cutaneous blood flow by causing vasoconstriction, leading to pallor, reduced temperature, or prevention of local inflammation. Major classes include:
- Alpha-Adrenergic Agonists: Phenylephrine, topical oxymetazoline, and norepinephrine enhance alpha-mediated vasoconstriction, reducing skin blood flow. These are used to shrink mucosal tissues (in nasal decongestants), decrease bleeding, or treat rosacea-induced erythema.
- Vasopressors: Systemically administered agents (e.g., epinephrine, dopamine at high doses) can reduce cutaneous circulation as part of their global vasoconstrictive and pressor effects.
- Corticosteroids: Topical glucocorticoids cause skin blanching by constricting cutaneous microvasculature; this property is often employed to assess steroid potency.
- Ergot Alkaloids: Used for migraine or postpartum hemorrhage, these cause intense vasoconstriction, including in skin vessels, and may rarely cause ischemic complications.
- Serotonin (5-HT2A) Agonists: Systemic serotonin receptor agonists (e.g., some triptans, DOI) centrally elicit sympathetically-mediated vasoconstriction. These effects involve spinal 5-HT2A receptors and may reduce cutaneous blood flow during psychological stress, fever, or alerting stimuli.
Neurotransmitter Mediation and Central Modulation
Central neurotransmitters profoundly influence cutaneous vascular tone through modulation of sympathetic output and direct receptor activity:
- 5-HT (Serotonin) Receptors: Serotonin 5-HT2A activation causes cutaneous vasoconstriction even after interruption of some central connections, revealing a key spinal mechanism. Blockade of 5-HT2A or use of 5-HT1A agonists reverses this effect, potentially useful in conditions with pathological vasoconstriction.
- Dopamine: Central dopamine D2 agonists can suppress cutaneous vasoconstriction induced by stress, highlighting a role for dopamine in neurogenic skin microcirculation control.
- Norepinephrine: The primary neurotransmitter inducing sympathetically-driven vasoconstriction, subject to modulation by centrally-acting drugs such as reserpine and clonidine (alpha-2 agonist).
Drugs with Predominant Local Effects
- Caffeine: When topically administered, caffeine’s effect on skin blood flow depends on both the compound’s properties and the state of the skin’s barrier. Caffeine and other amphiphilic or lipophilic drugs accumulate more when blood flow is reduced, potentially intensifying local effects or toxicity.
- Urea: A hydrophilic compound like urea shows little dependence on blood flow unless the barrier is artificially disrupted (e.g., via tape-stripping), in which case reduced flow leads to much higher local levels.
- Progesterone: Demonstrates an intermediate sensitivity to blood flow alterations, with mild increases in local concentration if cutaneous perfusion is decreased.
- Steroid Creams and Ointments: Can generate blanching, particularly those with higher potency, reflecting marked constriction of superficial dermal vessels.
Implications for Transdermal Drug Delivery
Cutaneous blood flow is a key determinant of percutaneous (through the skin) absorption and thus the effectiveness of transdermally administered pharmaceuticals. The effectiveness of drug delivery through the skin involves interplay between:
- Drug Lipophilicity: Lipophilic and amphiphilic drugs (e.g., caffeine, progesterone) are more affected by reductions in cutaneous blood flow, resulting in increased local retention within the skin while absorption of hydrophilic compounds is less affected unless the barrier is compromised.
- Passive vs. Active Processes: Passive diffusion limits the role of blood flow with poorly absorbed molecules, but active enhancement (e.g., by promoting local vasodilation) increases penetration and systemic availability.
- Application Site and Condition: Stripped or damaged skin (as achieved experimentally or as in diseases compromising the barrier) significantly alters drug dynamics with changes in perfusion being particularly crucial for hydrophilic agents.
Clinical strategies sometimes incorporate vasodilatory additives or physical methods (heat, massage) to increase local blood flow and thus drug flux, while vasoconstrictors can delay or localize effects.
Clinical Implications of Drug-Induced Cutaneous Blood Flow Changes
Alterations in cutaneous blood flow have broad relevance across dermatology, general medicine, and pharmacotherapy:
- Diagnostic and Therapeutic Monitoring: Changes in skin redness (erythema), pallor, or warmth following drug application are often used as indicators of local or systemic pharmacologic response.
- Drug Side Effects: Unintended vasodilation (e.g., facial flushing from calcium channel blockers) or vasoconstriction (e.g., pallor from topical steroids or ergot alkaloids) are important clinical considerations.
- Thermal Regulation and Safety: Medications interfering with cutaneous circulation can predispose patients to heat stress, hypothermia, or compromised wound healing, especially in the elderly or those with vascular disease.
- Local Accumulation and Toxicity: Impaired cutaneous blood flow can cause high local concentrations of topical drugs, increasing the risk of irritation, sensitization, or toxicity.
- Influence on Disease States: In Raynaud’s phenomenon, scleroderma, or diabetes, drug-induced changes in skin blood flow can modulate symptoms or exacerbate complications.
Future Directions in Research
Ongoing investigations aim to further elucidate:
- Genetic polymorphisms affecting microvascular drug responses.
- Innovative delivery platforms (e.g., microneedle patches) and their interactions with local perfusion.
- Non-invasive imaging and biomarker development for real-time monitoring of cutaneous blood flow and pharmacodynamic responses.
- Greater understanding of skin immune and barrier responses as mediated by changes in microcirculation.
Frequently Asked Questions (FAQs)
Q: How do topical corticosteroids change the appearance of the skin?
A: Topical corticosteroids constrict cutaneous vessels, often producing visible blanching (whitening) of the skin due to reduced blood flow.
Q: Are all drugs equally influenced by changes in skin blood flow?
A: No. Highly lipophilic or amphiphilic drugs (e.g., caffeine, progesterone) accumulate more in the skin when blood flow is reduced, while hydrophilic drugs like urea show less sensitivity unless the skin barrier is disrupted.
Q: Which medications are most likely to cause skin flushing?
A: Nitrates, nicotinates, and certain calcium channel blockers often cause vasodilation with associated erythema (skin redness) and warmth.
Q: How does stress or psychological state affect skin blood flow?
A: Psychological stress can trigger central nervous system responses that result in cutaneous vasoconstriction (reduced blood flow), mediated by neurotransmitter systems such as serotonin and dopamine.
Q: Why does skin temperature sometimes decrease after applying certain topical gels?
A: Volatile substances (e.g., isopropyl alcohol in gels) cool the skin through evaporation, temporarily decreasing temperature even if microcirculation is increased by an active ingredient.
References
- “Importance of Blood Flow to the Local Distribution of Drugs after Percutaneous Application.” (Karger, 1992)
- “Control of Cutaneous Blood Flow by Central Nervous System.” (PMC, 2016)
- “Comparison of Blood Flow to the Cutaneous Temperature and Redness…” (Journal of Biomedical Optics, 2006)
References
- https://karger.com/spp/article/4/1/1/819417/Importance-of-Blood-Flow-to-the-Local-Distribution
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4843916/
- https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-11/issue-1/014025/Comparison-of-blood-flow-to-the-cutaneous-temperature-and-redness/10.1117/1.2166370.full
- https://bpspubs.onlinelibrary.wiley.com/doi/10.1111/bcp.15490
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3230259/
- https://www.cochrane.org/evidence/CD003229_drugs-improve-blood-flow-people-who-have-poor-blood-circulation-veins-their-legs
Read full bio of medha deb












