Persistent Itching With No Visible Rash: Comprehensive Diagnostic Guide for Patients and Clinicians
Explore unknown triggers and tailored treatments for unexplained skin irritation.
Persistent Itching With No Visible Rash: Diagnostic Guide
Persistent itching—also known as pruritus—without any visible rash poses a diagnostic challenge for both patients and clinicians. This troubling symptom can significantly impact quality of life, yet its underlying causes are often difficult to pinpoint without comprehensive risk evaluation and clinical investigation. This article provides an extensive review of the causes, diagnostic methods, and clinical strategies when approaching persistent itching in the absence of overt skin changes.
Table of Contents
- Introduction
- Understanding Pruritus
- Common Causes of Itching With No Rash
- Systemic Conditions and Itching
- Medication-Related Itch
- Neuropathic and Psychogenic Itch
- Clinical Assessment and History Taking
- Diagnostic Tests and Investigations
- Special Populations
- Management Strategies
- Frequently Asked Questions
- Conclusion
Introduction
Chronic itching without a visible rash—referred to as pruritus sine materia—can arise from dermatological, systemic, neurological, or psychogenic causes. Diagnosing this condition requires careful clinical reasoning, as the absence of visible skin changes means physical examination alone may be insufficient for identifying the root cause. Persistent itch often affects older adults but may occur at any age, and can signal underlying pathologies ranging from dry skin to immune system dysfunction and chronic disease.
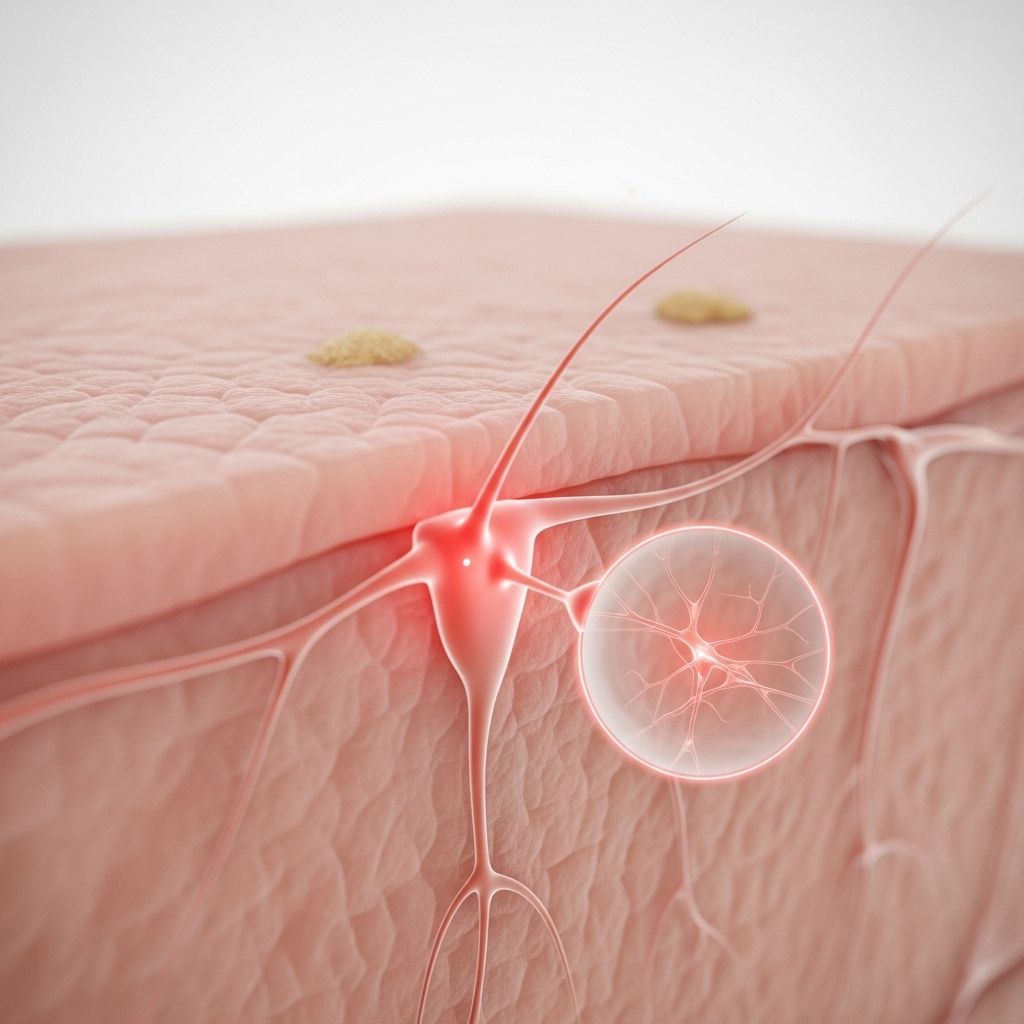
Understanding Pruritus
Pruritus is an uncomfortable sensation leading to the urge to scratch. While itch is most commonly associated with dermatological conditions, systemic illnesses and neurologic disorders can manifest with pruritus even when no rash is present. Classification is essential:
- Pruritus with skin lesions: Itch associated with visible rash or primary dermatological disease.
- Pruritus sine materia: Chronic itch with no detectable skin changes or lesions.
Patients may experience a wide range of symptoms:
- Localized or generalized itch
- Intermittent or constant sensation
- Worsening at night (nocturnal pruritus)
Common Causes of Itching With No Rash
Multiple factors, both external and internal, can lead to chronic itch without visible skin lesions. A systematic consideration includes:
- Dry Skin (Xerosis): The most frequent cause, especially in older adults, often due to environmental factors, excessive bathing, or diminished skin barrier function. Symptoms typically improve with regular use of moisturizing creams and emollients.
Source: AAAAI - Medication Side Effects: Common culprits include NSAIDs, opioids, antihypertensive drugs, and many others. The itching may arise within days to weeks of drug initiation.
- Immunological Dysfunction: Some individuals may have previously unrecognized immune system abnormalities, such as elevated IgE, low IgG, altered CD8 T-cell counts, or increased eosinophils, even without a rash.
Source: Washington University School of Medicine - Nerve Disorders: Neuropathic itch can result from diabetes (diabetic neuropathy), post-stroke sequelae, shingles (herpes zoster before blisters develop), or other nerve damage conditions.
Source: Healthline - Systemic Diseases: Kidney disease (especially advanced renal insufficiency), liver disease (e.g., cholestasis), hematologic malignancies (such as lymphoma), iron deficiency anemia, and thyroid dysfunction can cause pruritus.
- Mental Health Factors: Anxiety, depression, stress, OCD, and psychosis are all linked to itching sensations that are unrelated to skin pathology.
Source: Healthline - HIV/AIDS: Immune suppression is associated with higher rates of pruritus, sometimes preceding overt skin conditions.
Systemic Conditions and Itching
| Systemic Cause | Associated Features | Evaluation Tips |
|---|---|---|
| Renal Disease | Fatigue, swelling, abnormal urinalysis | Check renal function, creatinine, urea |
| Liver Disease | Jaundice, dark urine, pale stools | Liver panel, hepatitis serology |
| Thyroid Dysfunction | Weight change, palpitations, heat intolerance | TSH, T3, T4 |
| Iron Deficiency | Pallor, fatigue, restless legs | CBC, ferritin, iron studies |
| Hematologic Malignancy (Lymphoma) | Night sweats, lymphadenopathy | CBC, imaging, specialist referral |
Medication-Related Itch
Many medications can trigger itching as a side effect in the absence of a rash. Key drug classes to suspect include:
- NSAIDs (non-steroidal anti-inflammatory drugs)
- Opiates (morphine, codeine)
- Angiotensin-converting enzyme (ACE) inhibitors
- Antimalarials
- Statins and anti-hypertensives
- Cancer therapies
Assess the temporal relationship between drug initiation and onset of itching. For some patients, withdrawal or dose adjustment may alleviate symptoms.
Neuropathic and Psychogenic Itch
Neuropathic Itch
Neurological causes warrant consideration when itching is localized, accompanied by sensations such as tingling, burning, or numbness, or occurs after events such as stroke, shingles, or diabetic complications. Diagnosis often requires exclusion of other causes and may involve referral to neurology.
Psychogenic Itch
Psychological disorders can influence the skin through brain-skin interaction. Itching is common in anxiety and depression and may be exacerbated by stress or emotional states. Treatment may involve psychological support, behavioral therapy, or psychiatric intervention.
Clinical Assessment and History Taking
A thorough history and physical examination is critical in elucidating the cause of persistent itch.
- Duration and Onset: Chronic (>6 weeks) vs. acute
- Pattern: Localized or generalized
- Associated Symptoms: Night sweats, weight changes, fever, fatigue
- Triggers: Heat, cold, water contact, stress
- Medication History: Prescription, over-the-counter, herbal products
- Systemic Review: Organ-specific symptoms, exposure history
- Family History: Dermatologic or systemic illnesses
Physical examination should assess the skin for subtle changes (e.g., dryness, excoriations from scratching, subtle pigmentary changes). Evaluate lymph nodes, liver, and neurological signs as needed.
Diagnostic Tests and Investigations
Testing is guided by clinical suspicion but commonly includes:
- Blood Tests:
- Complete blood count (CBC)
- Liver and renal function panels
- Thyroid function tests
- Iron studies
- HIV testing
- Serum immunoglobulins (IgE, IgG)
- Urine Sample: Renal function, proteinuria
- Imaging: Chest X-ray, abdominal ultrasound in select cases
- Skin Biopsy: Rarely indicated unless subtle skin pathology is suspected
Additional testing may be tailored to suspected diagnoses (e.g., cancer screening, neurologic assessment).
Special Populations
Older Adults
Aging diminishes skin barrier function and increases susceptibility to both dry skin and immune changes, making unexplained itching more likely in the elderly population.
Immunosuppressed Patients
Individuals with HIV/AIDS, cancer, or who are on immunosuppressant medications may experience pruritus as a manifestation of underlying immune dysfunction even without skin lesions.
Children
Chronic itch without rash is uncommon in children, though differentials include atopic conditions, infestations (such as scabies before rash appears), and psychological factors.
Management Strategies
Management depends on the underlying cause. Empirical treatment may be required for idiopathic cases pending diagnosis.
- Moisturizer Therapy: Daily application of fragrance-free moisturizers for dry skin
- Removing Triggers: Discontinuation or substitution of causative medications
- Systemic Treatment: Treating underlying systemic condition (kidney, liver, thyroid disorders)
- Antihistamines: Used primarily for symptomatic relief, but efficacy may be limited in non-allergic pruritus
- Topical Therapies: Non-steroidal creams, menthol-containing lotions for localized relief
- Phototherapy: Ultraviolet light treatment for refractory cases
- Psychological Intervention: Cognitive-behavioral therapy, psychiatric medications for psychogenic itch
Interdisciplinary referrals may be necessary—for example, to neurology for neuropathic itch, oncology for suspected malignancy, or psychiatry for mental health evaluation.
Frequently Asked Questions (FAQs)
Q: If there is no rash, does itching mean I have a serious disease?
A: Itching without a rash is commonly due to dry skin, medication side effects, or mild systemic conditions. However, persistent or severe symptoms warrant evaluation for serious underlying diseases.
Q: How is chronic itch without a rash diagnosed?
A: Through detailed history-taking, physical examination, and targeted blood and urine tests. Imaging and referral to specialists may be required if systemic illness is suspected.
Q: What treatments are available for unexplained itching?
A: Options include moisturizers, modifying medications, treating underlying disease, antihistamines, phototherapy, and psychological support. In many cases, management is focused on treating the root cause and symptomatic relief.
Q: Can mental health issues cause itching with no rash?
A: Yes, psychological conditions like anxiety or depression may present with itch as a physical symptom. Treating the underlying mental health disorder often relieves symptoms.
Q: Is itchy skin with no rash a sign of cancer?
A: Some cancers, notably lymphoma, can present with generalized itch before other symptoms appear. However, most cases have benign causes. Persistent, unexplained pruritus warrants further investigation.
Conclusion
Persistent itching without a visible rash is a complex symptom with multiple potential causes. While dry skin is the most common culprit, a careful and methodical approach is essential to identify systemic, neurologic, immune, or psychological contributors and to direct appropriate management. For patients, early consultation with a healthcare provider can ensure timely diagnosis and treatment, minimizing discomfort and improving quality of life.
References
- https://www.aaaai.org/allergist-resources/ask-the-expert/answers/2023/itch
- https://medicine.washu.edu/news/itching-no-reason-immune-system-may-fault/
- https://www.healthline.com/health/skin/itchy-skin-no-rash
- https://www.medicalnewstoday.com/articles/325706
- https://www.pcds.org.uk/clinical-guidance/pruritus-without-a-rash
- https://www.mdanderson.org/cancerwise/what-types-of-cancer-can-cause-itchy-skin.h00-159774867.html
- https://my.clevelandclinic.org/health/diseases/11879-pruritus
- https://www.aad.org/public/everyday-care/itchy-skin/itch-relief/relieve-uncontrollably-itchy-skin
Read full bio of medha deb












