Persistent Dull Ache in Left Upper Quadrant After Eating: Causes, Diagnosis, and Management
Explains what organs and conditions may trigger abdominal discomfort following a meal.
The upper left section of the abdomen, known medically known as the left upper quadrant (LUQ), houses multiple organs, and pain localized to this area—especially after eating—can be indicative of a wide array of underlying medical conditions. This article aims to provide a comprehensive overview of persistent dull ache in the LUQ after meals, covering common causes, differential diagnoses, alarming symptoms, and approaches to management and prevention.
Table of Contents
- What Is Left Upper Quadrant Pain?
- Anatomy of the Left Upper Quadrant
- Common Symptoms Associated With LUQ Pain After Eating
- Common Causes of Persistent Dull Ache in LUQ After Eating
- Differential Diagnosis and Related Conditions
- Warning Signs: When to Seek Immediate Medical Attention
- How Persistent LUQ Pain Is Diagnosed
- Management and Treatment Options
- Prevention Strategies and Lifestyle Modifications
- Frequently Asked Questions (FAQs)
What Is Left Upper Quadrant Pain?
Left upper quadrant (LUQ) pain refers to discomfort or aching sensations located in the upper left region of the abdomen, beneath the rib cage. When this sensation is described as “dull” and persistent—especially after meals—it often points to issues related to the digestive, vascular, or genitourinary systems, but can also arise from other organs or referred pain.
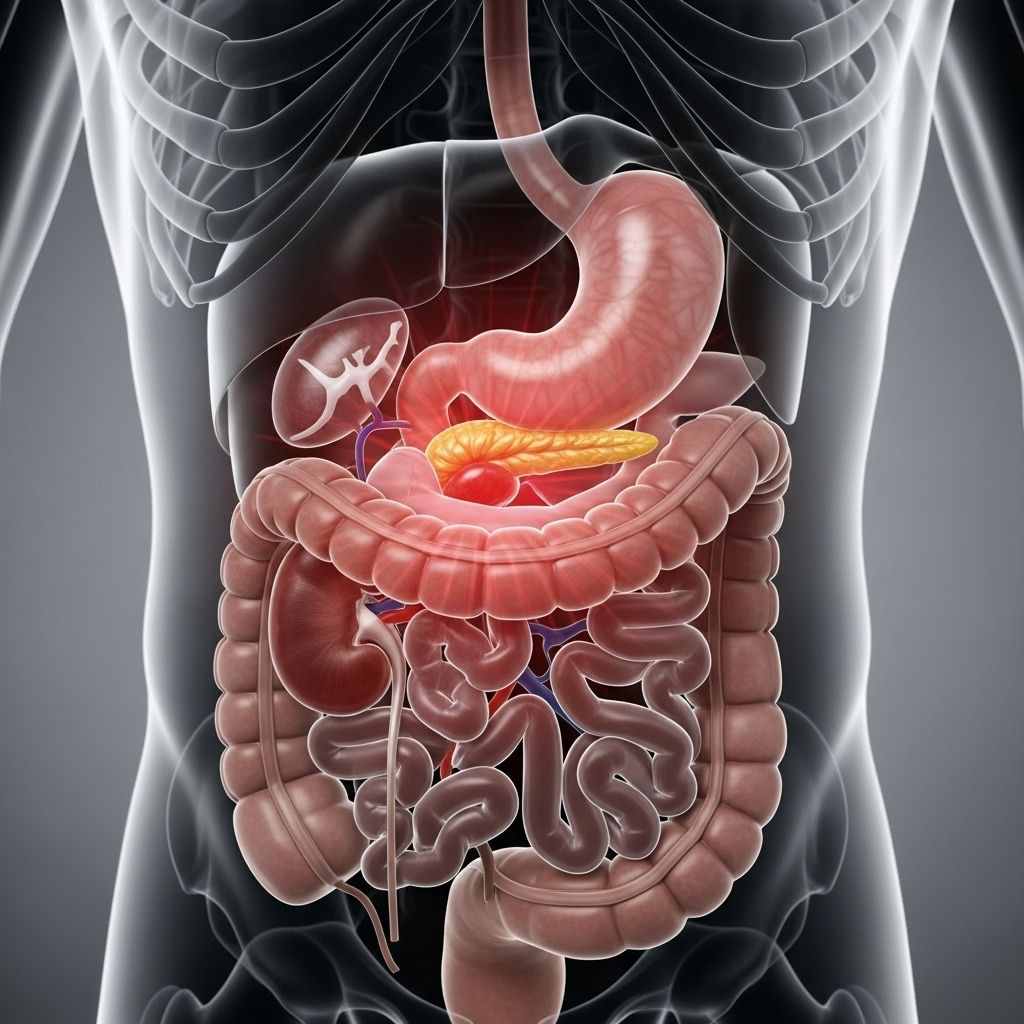
Anatomy of the Left Upper Quadrant
A clear understanding of the structures located in the LUQ is crucial to identifying potential sources of pain:
- Stomach: Primary site for food digestion; susceptible to gastritis, ulcers, and tumors.
- Spleen: Involved in blood filtration and immune response; can become enlarged or rupture.
- Tail of the Pancreas: Insulin and enzyme production; vulnerable to inflammation or pancreatic pathology.
- Left Kidney (Upper Portion): Can develop infections or stones that might radiate pain upward.
- Colon (Splenic Flexure): The bend where the transverse colon becomes the descending colon.
- Diaphragm (Left Crus): The muscular structure separating chest from abdomen.
- Heart and Left Lung (Inferior Edge): Pathology in these organs can cause referred pain to the LUQ.
- Blood Vessels: Including the aorta and its branches.
Common Symptoms Associated With LUQ Pain After Eating
While a persistent, dull ache is the main symptom, it often presents alongside other features, particularly when it is postprandial (after meals):
- Bloating or fullness
- Nausea or indigestion
- Early satiety (feeling full quickly)
- Belching or acid reflux
- Change in bowel habits (constipation or diarrhea)
- Loss of appetite or unintended weight loss
- Fatigue or general malaise
Careful correlation of these accompanying symptoms helps clinicians tailor diagnosis and management.
Common Causes of Persistent Dull Ache in LUQ After Eating
The LUQ encompasses multiple organ systems, and pain after eating can result from a variety of conditions involving these structures:
Digestive Tract Disorders
- Gastritis: Inflammation of the stomach lining, often resulting from infection with Helicobacter pylori, chronic NSAID use, or excessive alcohol. Typical features include gnawing pain in the LUQ worse with meals, nausea, and bloating.
- Peptic Ulcer Disease: Stomach or duodenal ulcers may cause LUQ pain, especially if on the lesser curvature or toward the stomach’s fundus. Pain may persist or worsen after eating, and can be accompanied by heartburn.
- Indigestion (Dyspepsia): Functional upper abdominal discomfort, worsened after eating heavy, fatty, or spicy foods. May overlap with gastritis or gastroesophageal reflux disease (GERD).
- Gastroenteritis: Infections of the gut lining can irritate the upper left abdomen and cause diffuse pain with additional symptoms such as diarrhea, nausea, and vomiting.
Pancreas-Related Causes
- Pancreatitis: Inflammation of the pancreas (especially the tail) can cause persistent LUQ or central upper abdominal pain radiating to the back, frequently aggravated by fatty meals. Associated features may include nausea, vomiting, fever, and malaise.
- Pancreatic Tumors: Tumors, especially in the tail of the pancreas, can lead to chronic dull ache in the LUQ, if large enough to compress adjacent structures. Weight loss, jaundice, and steatorrhea (fatty stool) may accompany.
Spleen-Related Causes
- Splenomegaly (Enlarged Spleen): Conditions such as blood disorders (lymphoma/leukemia), mononucleosis, or infections can cause the spleen to enlarge, resulting in a dull ache that is classically persistent and may gradually worsen. Early satiety (feeling full quickly) and mild fevers are common accompanying symptoms.
- Splenic Infarct: Rarely, the spleen may lose blood supply, causing dull LUQ pain, often with underlying sickle cell disease or clotting disorders.
Colon-Related Disorders
- Constipation: Fewer bowel movements can lead to distension of the colon near the splenic flexure, causing dull persistent ache worsened after eating or with straining.
- Diverticulitis: Inflammation or infection of pouches in the colon. While more common on the left lower abdomen, severe or complicated cases may cause radiating or referred LUQ pain, especially after meals.
- Irritable Bowel Syndrome (IBS): May cause intermittent LUQ discomfort and bloating, worsened by eating or stress, often accompanied by diarrhea or constipation.
Referred and Miscellaneous Causes
- Kidney Diseases: Infections or stones in the upper portion of the left kidney can radiate pain to the LUQ, especially after movement or eating causes increased kidney activity.
- Heart and Lung Problems: Conditions near the diaphragm, such as lower lobe pneumonia or myocardial infarction, may infrequently cause referred LUQ pain.
- Musculoskeletal Strain: Injury to abdominal wall muscles can mimic internal organ pain but typically is made worse by certain postures or activity and is generally unrelated to food intake.
Differential Diagnosis and Related Conditions
A wide spectrum of systemic, gynecological, and even psychological conditions can present with LUQ pain. Important related diagnoses to consider in persistent cases include:
- Stomach cancer: Progressive, persistent ache with weight loss and early satiety.
- Chronic pancreatitis or pancreatic cancer: Association with greasy stools, new-onset diabetes, and unexplained fatigue.
- Endometriosis or ovarian pathology (in females): Pain may be cyclic, related to menses, and can sometimes be referred upward from the pelvis.
- Autoimmune and hematologic conditions: Such as lupus or hemolytic anemias, often with systemic symptoms.
- Herpes zoster (shingles): Dull pain preceding skin rash in a band-like distribution across the LUQ.
Warning Signs: When to Seek Immediate Medical Attention
While many cases of LUQ pain after eating are benign, seek emergency care if you experience:
- Severe, sudden onset pain (especially after trauma)
- Shortness of breath, chest pain, or pain radiating to the jaw/left arm
- Vomiting blood or black, tarry stools
- Fever with chills, jaundice, or severe nausea
- Loss of consciousness or confusion
These may signal life-threatening conditions such as spleen rupture, heart attack, gastrointestinal bleeding, or overwhelming infection.
How Persistent LUQ Pain Is Diagnosed
Accurate diagnosis requires a thorough clinical evaluation, often involving multiple steps:
- Detailed history and physical examination focusing on location, intensity, triggers (such as eating), duration, associated symptoms, and prior medical conditions.
- Laboratory tests: Complete blood count (CBC) for infection or anemia, liver and pancreatic enzymes, metabolic panels, inflammatory markers.
- Urine analysis to check for renal or urinary tract sources.
- Non-invasive imaging:
- Abdominal ultrasound (spleen, pancreas, kidney, gallbladder, and other structures)
- CT scan or MRI for complex or unclear cases
- Endoscopy if peptic ulcer or gastric pathology is suspected
- Specialized tests (if indicated): Colonoscopy, cardiac evaluation, or gynecological assessment.
It is important to communicate the specific relationship of pain with meals, duration, and any associated systemic symptoms to your healthcare provider for proper diagnosis.
Management and Treatment Options
Management depends on the underlying cause identified, ranging from conservative to invasive approaches:
General Supportive Measures
- Eating smaller, more frequent meals
- Avoiding foods that trigger discomfort (e.g., fatty, spicy, or acidic foods)
- Staying well-hydrated and avoiding excess alcohol
- Engaging in stress-reducing techniques
Medical Management
- Antacids or proton pump inhibitors: For acid-related disorders such as gastritis or peptic ulcers (prescribed by a physician)
- Antibiotics: For infections such as gastroenteritis, diverticulitis, or urinary tract infection (if indicated)
- Enzyme replacement: In cases of pancreatic insufficiency
- Pain relievers: Avoid NSAIDs unless directed, as they may worsen gastrointestinal mucosal injury
- Laxatives or dietary fiber: For constipation, under medical supervision
- Treatment of underlying systemic or hematologic diseases as needed
Surgical and Advanced Treatment
- Endoscopic procedures: For persistent peptic ulcers or suspected cancer
- Surgical intervention: May be required for splenic rupture, complicated diverticulitis, or tumor excision
Prevention Strategies and Lifestyle Modifications
While not all causes are preventable, adopting healthy habits can reduce risks of developing LUQ pain after eating:
- Maintain a balanced diet rich in fiber, low in saturated fat and processed foods
- Regular physical activity to promote optimal digestion and bowel regularity
- Limit alcohol consumption and quit smoking
- Manage stress and anxiety, as these can exacerbate symptoms of IBS and dyspepsia
- Seek medical evaluation for persistent or worsening symptoms, especially with concerning signs
Frequently Asked Questions (FAQs)
What are the most common digestive causes of a dull LUQ ache after eating?
Common digestive causes include gastritis, peptic ulcers, dyspepsia, and occasionally pancreatitis. These conditions often present with pain worsening after meals, bloating, or indigestion symptoms.
Could this pain be a sign of something serious like cancer?
While most causes are benign, persistent or worsening LUQ pain, especially with weight loss or bleeding, warrants urgent investigation for serious conditions like pancreatic or stomach cancer.
Does persistent LUQ pain after eating always indicate a digestive problem?
No; while digestive disorders are common, LUQ pain can also stem from spleen, pancreas, kidney, heart, and even musculoskeletal causes. Other symptoms and associated history help determine the most likely source.
When should I see a doctor for LUQ pain after eating?
Consult a healthcare provider if your pain is persistent, severe, or associated with red flag symptoms such as fever, vomiting, unexplained weight loss, blood in the stool, or difficulty breathing.
What tests might my doctor order for persistent LUQ pain?
Depending on your symptoms, tests may include blood work, urine analysis, abdominal ultrasound, CT or MRI, and possibly endoscopy or colonoscopy to find a diagnosis.
Summary Table: Common Causes of Persistent LUQ Ache After Eating
| Category | Examples | Key Features |
|---|---|---|
| Digestive Disorders | Gastritis, Peptic Ulcer, Indigestion, Gastroenteritis | Pain after meals, bloating, heartburn, nausea |
| Pancreas Disorders | Pancreatitis, Pancreatic tumor/cyst | LUS pain radiating to back, worsened by food, weight changes |
| Spleen-Related | Splenomegaly, Splenic infarct | Persistent dull ache, early satiety, fatigue |
| Colon Disorders | Constipation, Diverticulitis, IBS | Bloating, altered bowel habits, intermittent pain |
| Referred/Miscellaneous | Kidney, heart, lung, muscle strain | Urinary symptoms, respiratory, trauma history |
If you or a loved one are experiencing persistent LUQ pain after eating, do not ignore the symptoms. Early assessment and management are key to preventing complications and ensuring optimal digestive health.
References
- https://patient.info/signs-symptoms/left-upper-quadrant-pain-leaflet
- https://www.vinmec.com/eng/blog/note-when-you-have-abdominal-pain-above-the-navel-on-the-left-side-en
- https://www.medparkhospital.com/en-US/lifestyles/left-sided-abdominal-pain
- https://www.premiermedicalhv.com/divisions/services/pancreatitis/
- https://my.clevelandclinic.org/health/symptoms/24736-upper-abdominal-pain
- https://www.medicalnewstoday.com/articles/325815
- https://www.cancertherapyadvisor.com/home/decision-support-in-medicine/hospital-medicine/left-upper-quadrant-abdominal-pain/
- https://www.mayoclinic.org/symptom-checker/abdominal-pain-in-adults-adult/related-factors/itt-20009075
Read full bio of medha deb












