Periodontal Disease and Heart Disease Link: Understanding the Connection
Reducing gum inflammation can ease bodily stress and improve your heart’s resilience.
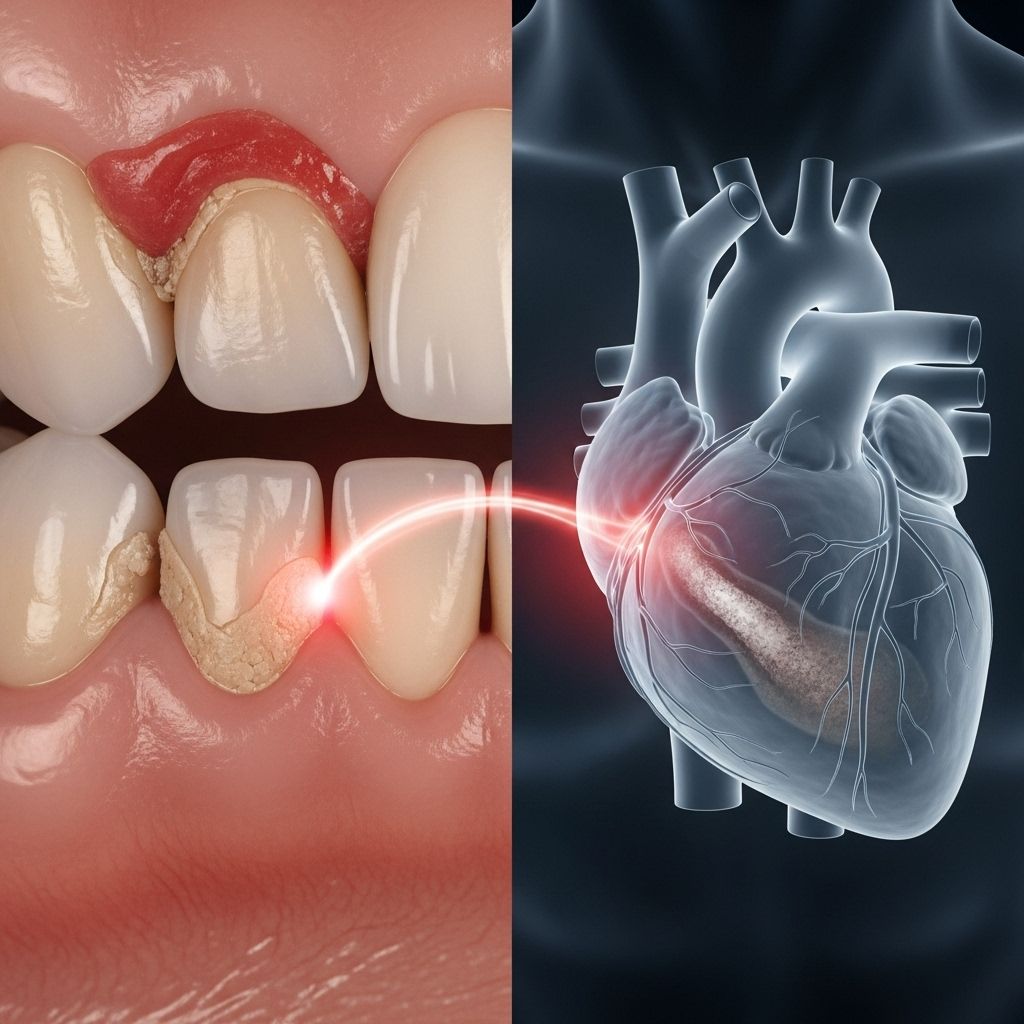
Table of Contents
- Understanding Periodontal Disease
- Cardiovascular Disease Overview
- Scientific Evidence Linking Periodontal and Heart Disease
- Mechanisms Behind the Connection
- Risk Factors and Demographics
- Treatment Benefits for Cardiovascular Health
- Prevention Strategies
- Clinical Implications and Healthcare Integration
- Frequently Asked Questions
Understanding Periodontal Disease
Periodontal disease represents a chronic bacterial infection that affects the supporting structures of teeth, including the gums, periodontal ligament, and alveolar bone. This progressive condition begins with the accumulation of bacterial plaque on tooth surfaces, leading to inflammation and eventual destruction of periodontal tissues if left untreated.
Stages of Periodontal Disease
Gingivitis marks the initial stage, characterized by inflammation of the gum tissues. At this reversible stage, patients may notice red, swollen gums that bleed during brushing or flossing. The infection remains confined to the gum tissue without affecting the underlying bone structure.
Periodontitis represents the advanced stage where inflammation extends beyond the gums to affect the bone and supporting structures. This irreversible condition can lead to tooth mobility, bone loss, and ultimately tooth loss if not properly managed.
Common Symptoms and Warning Signs
Recognizing periodontal disease symptoms enables early intervention and treatment. Key indicators include persistent bad breath, bleeding gums during oral hygiene routines, gum recession exposing tooth roots, loose or shifting teeth, and changes in bite alignment. Patients may also experience gum tenderness, swelling, and the formation of deep pockets between teeth and gums.
Cardiovascular Disease Overview
Cardiovascular disease encompasses a broad spectrum of conditions affecting the heart and blood vessels, representing the leading cause of mortality worldwide. These conditions include coronary heart disease, myocardial infarction, stroke, heart failure, and peripheral arterial disease.
The development of cardiovascular disease typically involves atherosclerosis, a process where fatty deposits accumulate in arterial walls, causing narrowing and reduced blood flow. Inflammation plays a crucial role in this process, making the connection to periodontal disease particularly significant from a mechanistic perspective.
Scientific Evidence Linking Periodontal and Heart Disease
Extensive research over recent decades has established a compelling association between periodontal disease and cardiovascular health outcomes. Multiple longitudinal studies and systematic reviews have demonstrated that individuals with periodontal disease face significantly elevated risks for various cardiovascular events.
Epidemiological Findings
Large-scale epidemiological studies reveal that patients with periodontal disease have a two to three times higher risk of experiencing heart attacks, strokes, or other serious cardiovascular events compared to individuals with healthy gums. Meta-analyses examining thousands of participants consistently demonstrate this association across diverse populations and geographical regions.
Research indicates that among patients with periodontal disease, the prevalence of cardiovascular disease reaches approximately 7.2%, while specific conditions show varying rates: coronary heart disease affects 6.6% of patients, hypertension occurs in 25.3%, stroke affects 1%, and heart failure impacts 1.1% of individuals with periodontal disease.
Gender Considerations
Comprehensive analyses reveal that the association between periodontal disease and cardiovascular risk exists independently of gender. Both men and women with periodontal disease demonstrate increased cardiovascular risk, with odds ratios of 1.22 for men and 1.11 for women, indicating no significant sex-based difference in this relationship.
Mechanisms Behind the Connection
Understanding the biological mechanisms linking periodontal disease to cardiovascular health provides crucial insights into this complex relationship. Multiple pathways contribute to the increased cardiovascular risk observed in patients with periodontal disease.
Systemic Inflammation Pathway
C-reactive protein (CRP) serves as a key biomarker linking periodontal disease to cardiovascular risk. Patients with periodontal disease consistently demonstrate elevated CRP levels, indicating systemic inflammation that contributes to atherosclerosis development and cardiovascular event risk.
The inflammatory response triggered by periodontal bacteria extends beyond the oral cavity, creating a systemic inflammatory state that promotes endothelial dysfunction, arterial inflammation, and accelerated atherosclerosis progression.
Bacterial Translocation
Periodontal pathogens, particularly Porphyromonas gingivalis, can breach the gingival epithelial barrier and enter the bloodstream. These bacteria have been detected in atherosclerotic plaques, suggesting direct bacterial involvement in cardiovascular pathogenesis.
Once in circulation, these oral pathogens can:
- Directly invade arterial walls and contribute to plaque formation
- Trigger inflammatory responses in vascular endothelial cells
- Enhance expression of inflammatory mediators like HMGB1
- Accelerate programmed cell death in cardiac tissues
Molecular Mechanisms
Research has identified specific molecular pathways through which periodontal disease influences cardiovascular health. P. gingivalis infection can enhance high mobility group box 1 (HMGB1) expression, a nuclear protein that induces inflammation and may increase myocardial infarction risk.
Additionally, periodontal pathogens can accelerate matrix metalloproteinase 9 activity, potentially compromising myocardial recovery processes and increasing the risk of cardiac complications following heart attacks.
Risk Factors and Demographics
Several factors influence the strength of the association between periodontal disease and cardiovascular health, creating varying risk profiles across different populations and clinical presentations.
Shared Risk Factors
Periodontal disease and cardiovascular disease share numerous common risk factors, which may partially explain their association:
| Risk Factor | Impact on Periodontal Disease | Impact on Cardiovascular Disease |
|---|---|---|
| Smoking | Impairs immune response, reduces healing | Promotes atherosclerosis, increases clotting risk |
| Diabetes | Compromises gum healing, increases infection risk | Accelerates atherosclerosis, damages blood vessels |
| Age | Cumulative tissue damage, reduced immunity | Age-related vascular changes, increased risk |
| Stress | Suppresses immune function | Increases blood pressure, promotes inflammation |
| Poor nutrition | Inadequate nutrients for tissue repair | Contributes to atherosclerosis risk factors |
Independent Risk Assessment
While shared risk factors contribute to the association, research demonstrates that periodontal disease represents an independent risk factor for cardiovascular disease, even after controlling for traditional cardiovascular risk factors such as smoking, diabetes, hypertension, and cholesterol levels.
Treatment Benefits for Cardiovascular Health
Emerging evidence suggests that periodontal treatment may provide cardiovascular benefits beyond oral health improvements, offering potential strategies for comprehensive cardiovascular risk management.
Inflammatory Marker Reduction
Multiple studies demonstrate that periodontal treatment consistently reduces C-reactive protein levels, indicating decreased systemic inflammation following gum disease management. This reduction in inflammatory markers correlates with potential cardiovascular risk reduction.
Treatment Modalities and Outcomes
Non-surgical periodontal treatment represents the most common intervention, including scaling and root planing procedures that remove bacterial deposits from tooth and root surfaces. These treatments effectively reduce periodontal inflammation and associated systemic inflammatory responses.
Surgical periodontal interventions may be necessary for advanced cases, involving procedures to regenerate lost periodontal tissues and eliminate deep bacterial infections.
Maintenance therapy ensures long-term success through regular professional cleanings and ongoing oral hygiene optimization.
Cardiovascular Outcome Improvements
Research indicates that comprehensive periodontal treatment may:
- Reduce systemic inflammation markers
- Improve endothelial function
- Decrease bacterial load in circulation
- Lower cardiovascular event risk over time
Prevention Strategies
Preventing periodontal disease represents a cost-effective approach to potentially reducing cardiovascular risk while maintaining optimal oral health.
Daily Oral Hygiene Practices
Brushing technique involves using fluoride toothpaste twice daily with proper brushing duration of at least two minutes. Electric toothbrushes may provide superior plaque removal compared to manual brushing.
Interdental cleaning through daily flossing or interdental brushes removes bacterial plaque from areas inaccessible to toothbrushes, preventing gingivitis development.
Antimicrobial mouth rinses can provide adjunctive benefits by reducing bacterial populations and maintaining optimal oral pH levels.
Professional Dental Care
Regular dental examinations enable early detection and intervention for periodontal disease. Professional cleanings remove calcified deposits that cannot be eliminated through home care alone.
Periodontal risk assessment during routine dental visits allows for personalized prevention strategies based on individual risk factors and oral health status.
Lifestyle Modifications
Smoking cessation represents the most impactful lifestyle change for both periodontal and cardiovascular health. Tobacco use significantly impairs gum healing and increases infection risk while simultaneously promoting cardiovascular disease development.
Nutritional optimization through balanced diets rich in antioxidants, omega-3 fatty acids, and essential vitamins supports both periodontal tissue health and cardiovascular function.
Clinical Implications and Healthcare Integration
The established connection between periodontal disease and cardiovascular health necessitates integrated healthcare approaches that address both oral and systemic health considerations.
Interdisciplinary Care Models
Collaboration between dental professionals and cardiovascular specialists enables comprehensive risk assessment and management strategies. Patients with existing cardiovascular disease may benefit from enhanced periodontal monitoring and treatment.
Healthcare providers should consider periodontal health when evaluating cardiovascular risk profiles, particularly in patients with multiple traditional risk factors.
Healthcare Policy Implications
The evidence linking periodontal disease to cardiovascular outcomes supports policy initiatives that integrate dental care into overall health management strategies. Preventive dental services may represent cost-effective interventions for cardiovascular disease prevention.
Insurance coverage expansion for periodontal treatments could potentially reduce long-term healthcare costs through cardiovascular event prevention.
Frequently Asked Questions
Q: Does gum disease directly cause heart disease?
A: While gum disease doesn’t directly cause heart disease, research shows a strong association between the two conditions. The relationship likely involves shared risk factors and inflammatory pathways rather than direct causation.
Q: Can treating gum disease reduce my heart attack risk?
A: Studies suggest that periodontal treatment may reduce systemic inflammation markers associated with cardiovascular risk. However, more research is needed to definitively establish whether treating gum disease directly prevents heart attacks.
Q: How often should I see a dentist if I have heart disease?
A: Patients with cardiovascular disease should maintain regular dental checkups every 3-6 months, depending on their periodontal health status. Your dentist and physician can coordinate to determine the optimal frequency.
Q: Are certain heart medications affected by gum disease?
A: Some cardiovascular medications may affect oral health, and severe gum infections could potentially impact drug absorption. Always inform both your dentist and physician about all medications you’re taking.
Q: What are the warning signs I should watch for?
A: Key warning signs include bleeding gums, persistent bad breath, loose teeth, gum recession, and changes in bite. If you have heart disease and notice these symptoms, consult your dentist promptly.
Q: Is the connection between gum disease and heart disease the same for men and women?
A: Research indicates that the association between periodontal disease and cardiovascular risk exists for both men and women without significant gender-based differences in risk levels.
References
- https://jdc.jefferson.edu/mphcapstone_presentation/540/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10010192/
- https://mypenndentist.org/dental-tips/2023/07/13/oral-health-and-heart-disease/
- https://www.health.harvard.edu/heart-health/gum-disease-and-heart-disease-the-common-thread
- https://www.health.harvard.edu/diseases-and-conditions/gum-disease-and-the-connection-to-heart-disease
- https://www.bhf.org.uk/informationsupport/heart-matters-magazine/research/gum-disease-heart-health
Read full bio of Sneha Tete












