Pelvic Pain in Women: Causes, Symptoms, Diagnoses & Treatments
Recognizing root causes is key to more effective treatment and better daily comfort.
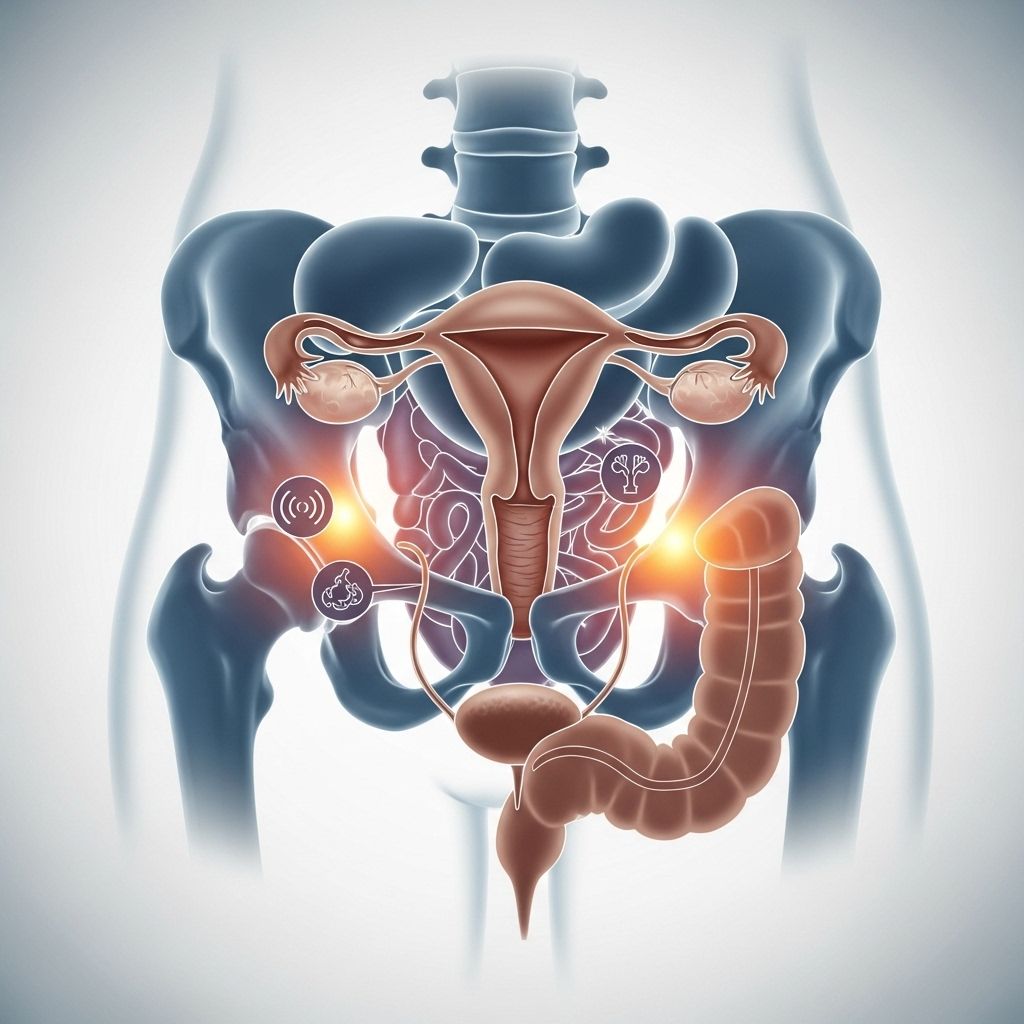
Pelvic pain is a common yet complex condition affecting many women at various stages of life. Understanding the potential underlying causes, recognizing the symptoms, and knowing when to seek medical help are critical in achieving timely relief and effective treatment. This comprehensive guide explores the prevalent causes, diagnostic strategies, and available treatments for pelvic pain in women.
What Is Pelvic Pain?
Pelvic pain refers to discomfort felt in the lower abdomen area, below the belly button and between the hips. The pain may be sudden or chronic, sharp or dull, and can range from mild discomfort to severe, debilitating cramps. Pelvic pain often signals a problem with one or more organs in the pelvic region, including the uterus, ovaries, bladder, or intestines.
6 Common Causes of Pelvic Pain in Women
Pelvic pain in women can arise from a range of sources, many of which require distinct approaches to diagnosis and treatment. Here are six of the most common causes that should not be ignored:
- Urinary tract infection (UTI)
- Fibroids
- Endometriosis
- Interstitial cystitis
- Pelvic inflammatory disease (PID)
- Other non-reproductive causes
1. Urinary Tract Infection (UTI)
A UTI is particularly common among women due to their anatomy, as the urethra is shorter, making it easier for bacteria to reach the bladder. Urinary tract infections often manifest as:
- Burning sensation during urination
- Frequent urge to urinate
- Pelvic pain or pressure
Antibiotics are usually effective in treating UTIs, but if the pain intensifies or is accompanied by fever or nausea, medical attention is needed urgently to rule out kidney infection.
2. Fibroids
Fibroids are benign (noncancerous) growths that develop in or on the uterus. Although many women have fibroids without symptoms, problems can arise when fibroids:
- Grow large or numerous, causing pelvic pressure
- Lead to painful or heavy menstruation
- Cause constipation, urinary issues, or long periods
Sometimes, fibroids degenerate if they outgrow their blood supply, which can result in intense, acute pain. Treatment options range from medications to surgical procedures, depending on fibroid size, number, and location.
3. Endometriosis
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, attaching to organs in the pelvic cavity and sometimes beyond. Endometriosis can cause:
- Severe, deep cramping and pelvic pain that may flare at any point in the menstrual cycle
- Gastrointestinal issues (bloating, constipation, diarrhea)
- Heavy periods, back pain, chronic fatigue
Treatment is often a combination of medication and surgery, and the severity of pain does not always correlate with the amount of tissue present.
4. Interstitial Cystitis
Interstitial cystitis, also known as painful bladder syndrome, is a chronic condition characterized by:
- Frequent and urgent need to urinate
- Pain or pressure in the bladder area
- Difficulty passing urine or feeling incomplete emptying
Symptoms are ongoing and may mimic those of a UTI but persist without infection. A urologist or urogynecologist can advise on the best treatment approaches, which may vary for each individual.
5. Pelvic Inflammatory Disease (PID)
PID is an infection of the female reproductive organs (uterus, fallopian tubes, or ovaries), often resulting from sexually transmitted infections (STIs), but not always. Symptoms may include:
- Pelvic pain or discomfort
- Unusual vaginal discharge
- Cramps, fever, and a positive STD screen
Prompt treatment with antibiotics is crucial to prevent serious complications such as infertility or widespread infection.
6. Other Non-Reproductive Causes of Pelvic Pain
Not every case of pelvic pain traces back to the reproductive system. Other potential causes include:
- Gastrointestinal issues (e.g., Irritable Bowel Syndrome, diverticulitis)
- Kidney stones or infections
- Hernias
- Musculoskeletal issues (e.g., broken pelvis, fibromyalgia, nerve conditions)
- Adhesions (scar tissue from previous surgeries or infections)
- Psychogenic pain (linked to stress or psychological conditions)
Addressing these causes may require referral to specialists such as gastroenterologists, urologists, or pain management experts.
Symptoms to Watch For
Pelvic pain varies widely among women but some common features include:
- Dull, aching feeling or sharp, stabbing pain in the lower abdomen
- Pain during menstruation, urination, sex, or bowel movements
- Associated symptoms: abnormal discharge, fever, gastrointestinal issues, fatigue
- Intensity or frequency unrelated to the underlying cause
Since symptoms can overlap with different illnesses, a careful and detailed medical history is essential for proper diagnosis.
How Is Pelvic Pain Diagnosed?
Diagnosis begins with a detailed discussion of your symptoms with a gynecologist or primary care provider, followed by a thorough physical examination. You should provide:
- Precise location and description of pain
- When and how the pain occurs: constant or intermittent, triggers or relievers
- Associated symptoms like fever, discharge, urinary or gastrointestinal complaints
Key Diagnostic Steps
- Physical pelvic exam: Checks organs, muscles, and identifies local tenderness or masses
- Pap test: Screens for cervical abnormalities
- Urine and blood tests: Help identify infection, inflammation, or other problems
- Ultrasound or imaging: Used to visualize reproductive organs, urinary tract, or digestive system
- Laparoscopy: Minimally invasive surgery, typically used to confirm endometriosis or assess unexplained pelvic pain
If initial evaluations are inconclusive, referrals to other specialists (gastroenterology, urology, or pain management) or additional testing may be warranted. Sometimes, pelvic pain may be caused by conditions not directly related to reproductive organs.
Table: Common Causes of Pelvic Pain and Their Features
| Cause | Typical Symptoms | First-line Treatment |
|---|---|---|
| UTI | Burning pee, urgency, pelvic ache | Antibiotics |
| Fibroids | Heavy/painful periods, pressure, constipation | Medication, surgery |
| Endometriosis | Cramping, GI symptoms, fatigue | Medication, surgery |
| Interstitial Cystitis | Bladder pain, urgency, frequency | Lifestyle, bladder treatments |
| PID | Pain, discharge, fever | Antibiotics |
| Non-reproductive Causes | Varies: GI pain, urinary pain, musculoskeletal | Depends on underlying cause |
How Is Pelvic Pain Treated?
Treatment is determined by the underlying cause(s):
- Medications: Antibiotics for infections, hormonal therapies for endometriosis or fibroids, pain relievers
- Lifestyle Modifications: Dietary changes, physical therapy, stress reduction techniques
- Pelvic Floor Physical Therapy: Especially helpful in cases with muscle tension, myalgia, or postural issues
- Surgery: Removal of fibroids, endometrial tissue, or treating adhesions
- Multidisciplinary Approach: For chronic or complex cases, combining gynecology, urology, gastroenterology, pain management, and mental health support
Some causes can be addressed with a single treatment, while others require combination therapies and ongoing management for the best outcome.
When Should You See a Doctor?
- If your pelvic pain is severe, persistent, or worsening
- When pain is accompanied by fever, nausea, vomiting, or unusual discharge
- If you experience symptoms during pregnancy
- When pelvic pain impacts your daily life or is associated with pain during sex, urination, or bowel movements
Ignoring persistent pelvic pain can result in serious complications, including fertility problems, chronic infection, or severe illness, so prompt evaluation is critical.
Frequently Asked Questions (FAQs)
What is considered chronic pelvic pain?
Chronic pelvic pain is generally defined as non-cyclic pain lasting six months or longer, originating from the pelvic region and significantly impacting physical, sexual, or emotional wellbeing.
Can pelvic pain be caused by more than one problem?
Yes. Multiple medical conditions may coexist in the pelvic region, and women with one chronic pain diagnosis are at increased risk for developing others.
Do hormonal changes affect pelvic pain?
Hormonal fluctuations—especially during menstruation, ovulation, or menopause—can exacerbate existing pelvic conditions like endometriosis or fibroids, but are rarely the sole cause.
Are there lifestyle changes that can help relieve pelvic pain?
Lifestyle measures such as stress reduction, gentle exercise, dietary modifications, and physical therapy may effectively reduce symptoms, particularly for chronic or musculoskeletal pain sources.
When is surgery necessary for pelvic pain?
Surgery is generally reserved for cases when less invasive treatments are unsuccessful or when certain conditions—like large fibroids, endometriosis, or structural problems—demand removal or correction.
Tips for Managing Pelvic Pain at Home
- Use a heating pad or warm compress on your lower abdomen to ease cramps
- Consider over-the-counter pain relievers, as recommended by a healthcare provider
- Avoid triggers (such as certain foods or activities) that worsen your symptoms
- Maintain good hydration, regular gentle exercise, and stress management routines
- Seek support groups or counseling for chronic pain
Conclusion
Pelvic pain in women is a multifaceted condition with various causes—it is not a symptom to ignore. While some forms are easily treated, others involve complex factors requiring careful diagnosis and management. Being proactive about seeking care, tracking symptoms, and pursuing appropriate treatments offers the best chance for relief and restored quality of life.
References
- https://www.goodhousekeeping.com/health/g5190/pelvic-pain/
- https://bestpractice.bmj.com/topics/en-us/722
- https://www.nichd.nih.gov/health/topics/pelvicpain/conditioninfo/causes
- https://www.goodhousekeeping.com/uk/health/a556230/how-to-strengthen-your-pelvic-floor-exercises/
- https://www.nichd.nih.gov/health/topics/pelvicpain
- https://uroweb.org/guidelines/chronic-pelvic-pain
- https://www.auanet.org/guidelines-and-quality/guidelines/male-chronic-pelvic-pain
Read full bio of Sneha Tete












