Pelvic Pain in Women Beyond Menstruation: Causes, Diagnosis, and Effective Management
Expert insights into chronic lower abdominal distress pave the way for tailored care.
Pelvic pain is a common concern in women, frequently associated with menstruation. However, many women experience pelvic pain beyond their period, which can be persistent, severe, and challenging to diagnose. This comprehensive guide explores the many causes, the difficulties in obtaining a diagnosis, the diagnostic tools available, and strategies for management and relief.
Table of Contents
- Understanding Pelvic Pain Beyond Menstruation
- Common Causes of Pelvic Pain Beyond Menstruation
- Diagnosing Pelvic Pain: Challenges and Misdiagnosis
- When to Seek Medical Help
- Diagnostic Tools and Approach
- Management and Treatment Options
- Lifestyle Adjustments and Support
- Frequently Asked Questions (FAQ)
Understanding Pelvic Pain Beyond Menstruation
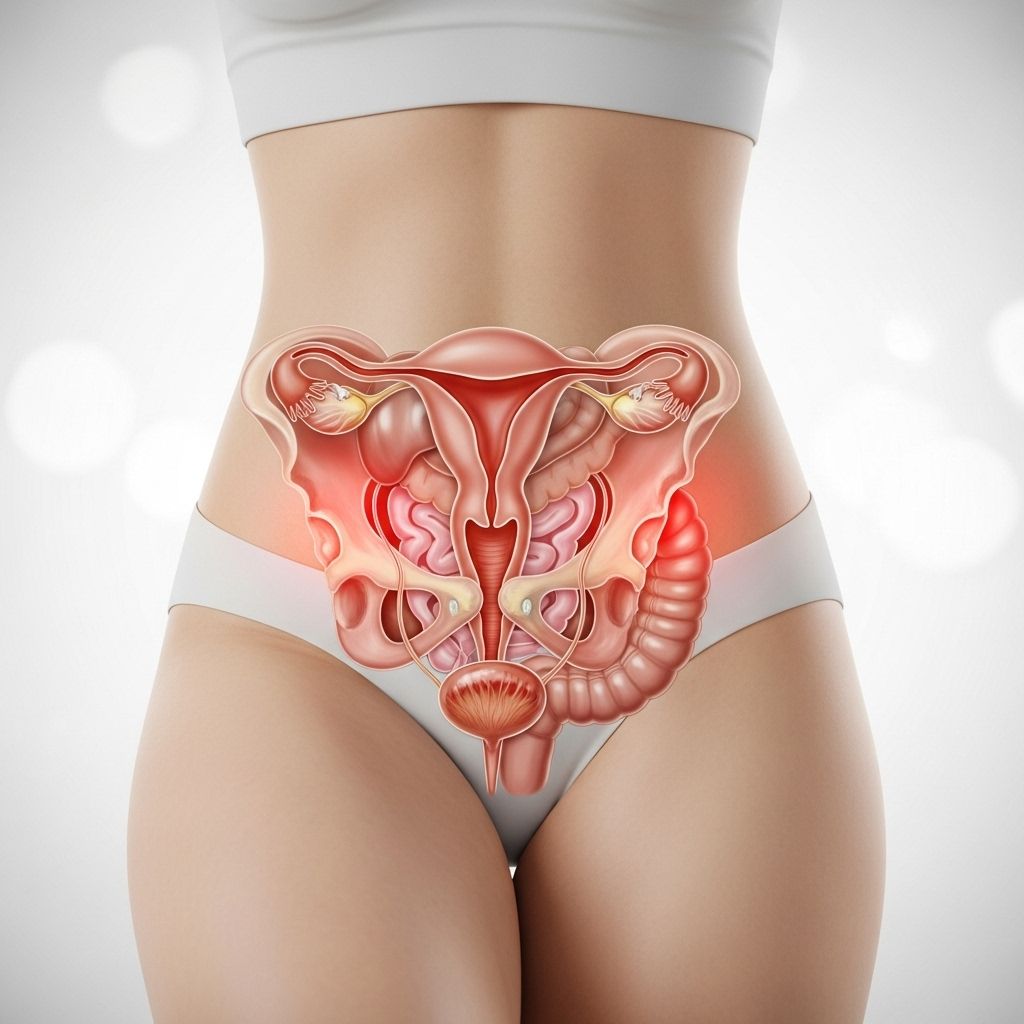
Pelvic pain outside of menstruation refers to discomfort felt in the lowest part of the abdomen — between the belly button and groin — that persists or recurs at times other than during a menstrual period. This symptom may appear suddenly (acute) or last for months to years (chronic), affecting quality of life and daily functioning. Importantly, pelvic pain may be mild or severe, sharp or dull, constant or intermittent, and can be localized or diffuse.
Women commonly attribute pelvic pain to their reproductive tract, yet there are many potential sources within the reproductive, urinary, digestive, musculoskeletal, and nervous systems. Sometimes, more than one condition contributes to a woman’s pain simultaneously .
Common Causes of Pelvic Pain Beyond Menstruation
Pelvic pain in women outside the context of menstruation can arise from a myriad of causes, some specific to the reproductive system and others involving neighboring organs or tissues. Understanding these helps guide evaluation and treatment.
| System / Organ | Potential Causes | Key Features |
|---|---|---|
| Reproductive System |
|
If you find yourself dealing with lingering discomfort, explore the potential reasons behind it in our detailed article on the persistent dull ache in the left upper quadrant, including diagnostics and management options. This resource may hold the key to alleviating your discomfort. |
| Urinary System |
|
|
| Digestive System |
|
|
| Musculoskeletal/Nervous System |
|
|
Reproductive Origin Causes
- Endometriosis: Growth of tissue similar to the uterine lining outside the uterus, causing often severe pelvic pain, pain with intercourse, pain during bowel movements, and infertility .
- Pelvic Inflammatory Disease (PID): Infection and inflammation of the reproductive organs, often resulting in chronic pain, abnormal discharge, or fever.
- Pelvic Adhesions: Scar tissue from previous inflammation or surgery may tether organs and cause persistent pain .
- Uterine Fibroids: Benign growths of the uterus that can cause cramping, heaviness, pain with intercourse, and pressure symptoms.
- Ovarian Cysts: Fluid-filled sacs in or on ovaries; can rupture or cause torsion, leading to sudden or persistent pain.
- Ectopic Pregnancy: Life-threatening emergency when a fertilized egg implants outside the uterus; classic symptoms are sharp pelvic pain, vaginal bleeding, and dizziness .
Urinary System Causes
- Urinary Tract Infections (UTIs) & Cystitis: Infections can cause suprapubic pain, burning during urination, urinary frequency, or urgency .
- Interstitial Cystitis (Painful Bladder Syndrome): Chronic, non-infectious bladder inflammation causes pelvic pain, especially with a full bladder, and can be accompanied by painful urination and frequent urges .
- Urinary Stones: Stones in the kidneys or bladder may lead to severe lower abdominal or pelvic pain radiating to the groin, as well as visible blood in urine .
Digestive Tract Causes
- Irritable Bowel Syndrome (IBS): Chronic digestive disorder leads to abdominal pain, bloating, and changes in bowel habits (constipation/diarrhea). The pain often improves after a bowel movement .
- Inflammatory Bowel Disease (IBD): Includes Crohn’s disease and ulcerative colitis, both causing persistent abdominal and pelvic pain, diarrhea, and sometimes bloody stools .
- Constipation and Diverticulitis: Can generate cramping or aching pelvic discomfort.
Musculoskeletal and Neurologic Causes
- Pelvic Floor Dysfunction: Weakening, injury, or spasm of the pelvic floor muscles can create persistent pain, disrupting urination, defecation, or sexual function .
- Hernias and nerve entrapment can cause localized pain, which may worsen with activity or certain positions.
Other Causes
- Post-surgical pain (from scarring or adhesions)
- Nerve pain (neuropathy)
- Psychological conditions (chronic pain syndromes can be linked with anxiety, depression, or trauma)
Diagnosing Pelvic Pain: Challenges and Misdiagnosis
The diagnosis of pelvic pain in women is inherently complex due to:
- The wide variety of potential underlying causes.
- Overlapping symptoms between abdominal, reproductive, urinary, and musculoskeletal conditions.
- Women frequently presenting with multiple pain conditions simultaneously (e.g., IBS and endometriosis) .
- Variable pain perception, reporting, and treatment response among individuals.
- Historically, women’s pain may have been dismissed or attributed solely to stress or menstruation, leading to delayed or inaccurate diagnoses .
This diagnostic complexity necessitates a thorough, multi-faceted approach by healthcare professionals.
When to Seek Medical Help
While some mild pelvic discomfort may not be concerning, medical evaluation is urgent if you experience:
- Sudden, severe pelvic pain
- Pain associated with fever, nausea, or vomiting
- Pain with vaginal bleeding outside of periods
- Pain with fainting or dizziness (may suggest ectopic pregnancy)
- Pain that interferes with daily life, sexual activity, or fertility
- Pain that persists despite over-the-counter treatments
Early consultation with a women’s health specialist can improve outcomes and help avoid complications.
Diagnostic Tools and Approach
A comprehensive evaluation for pelvic pain typically involves:
- Detailed medical history: Including onset, duration, severity, relationship to periods, sexual activity, urination, and bowel movements .
- Physical examination: Checking for tenderness, palpable masses, and examination of the pelvic organs, muscles, and nerves.
- Laboratory tests: Blood and urine tests to check for infection, inflammation, or bleeding.
- Imaging: Most commonly ultrasonography (transvaginal and/or transabdominal). CT or MRI scans may be considered for further evaluation or complex cases .
- Diagnostic procedures: Laparoscopy (a minimally invasive surgery) may be done if endometriosis, adhesions, or other internal causes are suspected and not found on imaging.
Diagnosis is often a process of exclusion, ruling out the most urgent causes first (ectopic pregnancy, appendicitis, infection), followed by systematic investigation of reproductive, urinary, and digestive systems.
Management and Treatment Options
Management of pelvic pain in women extends beyond treating the underlying condition; it often requires an integrated and individualized approach:
Medical Treatments
- Analgesics: Over-the-counter NSAIDs (ibuprofen, naproxen) or prescription medications for pain relief.
- Hormonal therapy: Oral contraceptives, progestins, or Gonadotropin-releasing hormone (GnRH) analogues for endometriosis, ovarian cysts, and fibroids.
- Antibiotics: For proven cases of pelvic inflammatory disease, UTIs, or cystitis.
- Bladder instillations: For interstitial cystitis (direct introduction of medicines into the bladder).
- Bowel management: Fiber supplements, antispasmodics, or other IBS/IBD therapies.
Minimally Invasive and Surgical Techniques
- Laparoscopy: Both diagnostic and therapeutic—allows for treatment of endometriosis, removal of cysts, or lysis of adhesions.
- Hysteroscopic or laparotomic surgery: For larger tumors or fibroids.
- Urologic or gastrointestinal surgery: For stones, severe diverticulitis, or bowel disease not responsive to medical therapy.
Physical Therapy and Integrative Approaches
- Pelvic floor physical therapy: Effective for muscular or tension-related causes.
- Biofeedback: Helps manage muscle tension and chronic pain syndromes.
- Trigger point injections: Useful for muscle spasms.
Psychological and Behavioral Support
- Cognitive behavioral therapy (CBT): To manage chronic pain, associated anxiety, depression, or emotional distress.
- Mindfulness, stress management, and relaxation techniques.
A multidisciplinary team—often involving gynecologists, urologists, gastroenterologists, physiotherapists, and psychologists—is optimal for complex, chronic pelvic pain.
Lifestyle Adjustments and Support
Simple, supportive strategies can also help alleviate or prevent worsening pelvic pain:
- Regular exercise (gentle stretching, yoga, and walking)
- Application of heat (warm baths or heating pads)
- Managing bowel habits (diet high in fiber, adequate hydration)
- Routine gynecologic care and STI prevention practices
- Support groups or online communities for chronic pain
Frequently Asked Questions (FAQ)
Q: Can pelvic pain be normal if it happens outside my period?
A: While mild, short-lived pelvic discomfort is not uncommon, persistent or severe pelvic pain outside menstruation is not considered normal and warrants medical evaluation.
Q: What conditions besides reproductive issues can cause pelvic pain in women?
A: Urinary tract infections, interstitial cystitis, irritable bowel syndrome, inflammatory bowel disease, musculoskeletal disorders, and nerve conditions may all cause pelvic pain in women .
Q: What if multiple tests come back negative but I still have pain?
A: Chronic pelvic pain is complex and sometimes more than one undetected or overlapping issue is present. Specialized pain clinics and multidisciplinary teams can help guide further management .
Q: Is pelvic pain always a sign of cancer?
A: Most causes of pelvic pain are benign or treatable conditions. However, persistent, unexplained pain should be evaluated to exclude more serious causes, including cancers.
Q: Can stress or emotional factors worsen pelvic pain?
A: Yes, stress, anxiety, and depression can heighten pain perception and are often intertwined with chronic pelvic pain syndromes. Addressing psychological well-being is important in management.
Remember: Timely consultation with healthcare professionals improves care, reduces risks, and supports a return to quality living for women experiencing pelvic pain beyond menstruation.
References
- https://www.texaschildrens.org/content/wellness/why-pelvic-pain-may-be-misdiagnosed-and-what-you-can-do
- https://www.webmd.com/women/cramps-but-no-period
- https://www.medicalnewstoday.com/articles/323796
- https://www.nichd.nih.gov/health/topics/factsheets/pelvicpain
- https://www.mayoclinic.org/symptom-checker/pelvic-pain-in-adult-females-adult/related-factors/itt-20009075
- https://nortonhealthcare.com/news/causes-of-pelvic-pain/
- https://www.centerofendometriosis.com/blog/pelvic-pain-causes-metro-detroit-etcoa/
- https://www.spirehealthcare.com/health-hub/specialties/womens-health/what-causes-cramps-no-period-and-white-discharge/
- https://www.uhhospitals.org/blog/articles/2019/07/3-signs-that-your-pelvic-pain-could-be-endometriosis
Read full bio of medha deb












