Pediatric Barrier Function: Physiological Development in Infants, Skin and Gut Health, and Implications for Lifelong Well-Being
Early skin and gut care set the stage for a resilient immune system and healthy growth.
Pediatric Barrier Function: Infants and Development
The health and resilience of infants depend profoundly on two essential physiological barriers: the skin and the gut. These barriers play central roles in protecting infants from external pathogens, regulating interactions with the environment, and supporting immune development. Their maturation is a dynamic process beginning in utero and extending through the first years of life—a critical window that lays the foundation for lifelong well-being.
Table of Contents
- Introduction to Barrier Function in Pediatrics
- Skin Barrier Function in Infants
- Gut Barrier Function and Microbiome Development
- Maturation and Developmental Timeline
- External and Internal Factors Influencing Barrier Development
- Common Barrier-Related Disorders in Infancy
- Clinical Implications and Preventative Measures
- Frequently Asked Questions
Introduction to Barrier Function in Pediatrics
Infants enter the world with developing biological systems designed to protect their bodies from harm while exchanging beneficial molecules with their environment. These barrier systems—primarily the skin and the gut—are structurally and functionally distinct from those of adults and undergo significant maturation over the first months and years of life.
Barrier function refers to the set of physical and biochemical properties that regulate the passage of water, ions, nutrients, immune factors, and pathogens across tissue boundaries. In neonates and infants, the maturation of these barriers influences vulnerability to infection, sensitivity to environmental agents, hydration status, and immune development. The implications of barrier function extend to the risk of allergic and autoimmune diseases and overall resilience to illness.
Skin Barrier Function in Infants
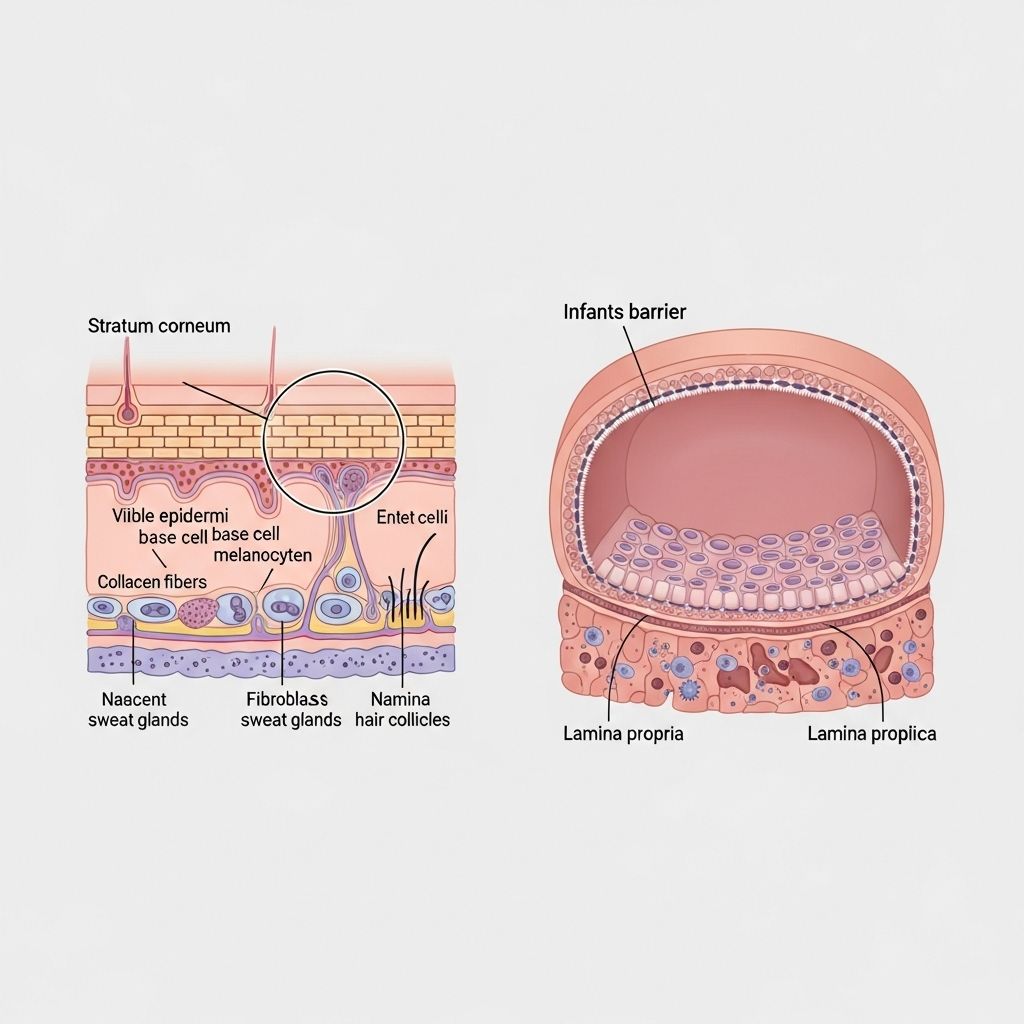
Structure and Physiology
The skin is the largest organ and its primary barrier, the stratum corneum (SC), protects the body from external insults and regulates water loss. Infant skin differs significantly from adult skin in the following ways:
- Thinner stratum corneum and epidermal layer leading to increased permeability.
- Smaller corneocytes and less organized dermal extracellular matrix.
- Higher rates of transepidermal water loss (TEWL), making infants susceptible to dehydration.
- Inefficient formation of the acid mantle—the acidic pH that provides antimicrobial protection and influences microbiome establishment.
Structural Differences Between Infant and Adult Skin
| Feature | Infant Skin | Adult Skin |
|---|---|---|
| Stratum Corneum Thickness | Thin | Thicker, more layered |
| Epidermal Maturity | Less mature | Fully matured |
| Collagen Organization | Less dense | More organized |
| Transepidermal Water Loss | High | Low |
| Acid Mantle Formation | Incomplete | Established |
| Natural Moisturizing Factor (NMF) | Lower | Higher |
Timeline of Skin Barrier Maturation
- Gestation: Epidermal and barrier development begins during the first trimester.
- Full-term infants: Have a well-formed SC at birth (34 weeks gestation), but maturation continues postnatally.
- Preterm infants: Exhibit significantly compromised skin barrier with thinner layers and higher vulnerability, especially in the first 2–3 weeks after birth.
- Vernix caseosa: At birth, newborn skin is coated with a protective, hydrophobic layer of lipids, proteins, and water, guarding against water loss and infection. This is gradually removed in the first hours to days, increasing vulnerability.
Functional Implications
- Protection: The immature skin barrier increases susceptibility to irritants, allergens, and microbes.
- Hydration: Elevated TEWL can result in dry or inflamed skin, raising the risk for eczema and atopic dermatitis.
- PH Regulation: As the acid mantle forms, skin pH shifts from near neutral to more acidic, enhancing defense and regulating the formation of the microbiome.
Impact of Products and Practices
- Diapers and wipes: Regular use can influence barrier integrity and water loss; product composition matters.
- Bathing: WHO recommends delaying the first bath for at least six hours after birth to preserve natural protection from the vernix caseosa.
- Skin care products: Mild, pH-adjusted cleansers and emollients are recommended to protect the developing barrier.
Gut Barrier Function and Microbiome Development
Gut Structure and Selective Barrier Function
At birth, the gastrointestinal (GI) tract is tasked with a dual role: defending against harmful pathogens and antigens, while allowing selective passage of nutrients and maternal antibodies necessary for immune development. Key structural components include:
- Mucus layer: Provides a physical blockade and habitat for beneficial bacteria.
- Intestinal epithelium: A single layer of tightly joined cells with selective transport functions, including active endocytosis to internalize beneficial macromolecules.
- Local immune system: Includes lymphoid tissues and immune cells that interact with microbes and regulate tolerance and defense.
Microbiome Development and the Gut-Brain Axis
Infants begin acquiring their intestinal microbiome at birth, with significant changes occurring in the first 36 months. This process is influenced by:
- Mode of delivery: Vaginal delivery exposes infants to maternal vaginal and fecal microbiota, while cesarean section leads to colonization by skin and hospital-associated microbes.
- Diet: Breastfeeding introduces protective antibodies (like IgG), oligosaccharides, and beneficial bacteria, while formula feeding supports distinct microbial profiles.
- Antibiotic exposure: Can disrupt microbial diversity and resilience.
- Environmental exposures: Contact with household members, pets, and surroundings shape microbiome composition and barrier training.
The gut microbiome, immune cells, and neurodevelopment are intricately linked via the microbiome-gut-brain axis, which coordinates metabolic, immune, and neurological signaling. Critical windows during early childhood may set lifelong risk trajectories for diseases including allergies, autism spectrum disorder, inflammatory bowel disease, and neuropsychiatric conditions.
Immature Gut Barrier and Macromolecular Transfer
- Selective transfer: The neonatal gut allows passage of maternal IgG and other bioactive molecules, supporting immune system training.
- Risk of permeability: Increased permeability enables transfer of not only nutrients but also microbial metabolites that—if deregulated—can trigger inflammation and immune dysregulation.
Maturation and Developmental Timeline
- Prenatal period: Structural formation of skin and gut epithelium begins; maternal health and exposures influence initial barrier properties.
- Birth–6 months: Rapid changes in skin hydration, TEWL, acid mantle establishment, and gut microbial colonization. Breast milk and early nutrition are pivotal.
- 6–36 months: Progressive strengthening of both barriers, adult-like microbiome achieved, immune tolerance and resilience developed, skin maturation nearing completion.
External and Internal Factors Influencing Barrier Development
- Genetic makeup: Influences structure, function, and sensitivity to external insults.
- Gestational age: Preterm infants have thinner, more permeable skin and less mature gut epithelium.
- Nutrition: Breastfeeding enhances barrier function via bioactive factors; early introduction of solids may influence microbiome and risk of allergies.
- Environmental exposures: Early contact with diverse microbes promotes immune training; excessive hygiene or antibiotic use may stunt beneficial colonization.
- Topical care: Unnecessarily harsh skin care products, frequent wetting/drying, or toxicants may impede barrier function.
Common Barrier-Related Disorders in Infancy
- Atopic dermatitis: Linked to delayed or deficient skin barrier development, high TEWL, and altered skin pH.
- Diaper dermatitis: Results from moisture, friction, and irritants overwhelming immature skin.
- Food allergies: Associated with increased gut permeability allowing sensitization to dietary antigens.
- Infections: Compromised skin or gut barriers can increase risk for local or systemic infections.
Clinical Implications and Preventative Measures
Supporting Healthy Barrier Development
- Skin: Use of pH-neutral cleansers, protective emollients, and avoidance of unnecessary exposure to irritants or harsh chemicals.
- Gut: Promotion of breastfeeding when possible, prudent use of antibiotics, and consideration of probiotics or prebiotics in special circumstances.
- Environmental exposures: Controlled introduction of diverse, low-pathogen environments to stimulate immune maturation.
- Monitoring: Watch for signs of barrier compromise such as persistent dryness, rash, recurrent infections, or feeding difficulties.
Recommendations
- Delay bathing full-term infants to preserve vernix caseosa for several hours after birth.
- Provide gentle, fragrance-free skin care products and avoid excessive scrubbing.
- Encourage skin-to-skin contact and appropriate exposure to household microbes.
- Support healthy gut colonization through breastfeeding and careful dietary transitions.
Frequently Asked Questions (FAQs)
Q: What are the main differences between infant and adult skin?
A: Infant skin has a thinner stratum corneum, higher water loss, incomplete acid mantle, and less mature collagen structure, making it more permeable and vulnerable to external irritants.
Q: Why is the gut barrier important in infancy?
A: The immature gut allows selective passage of protective antibodies, nutrients, and antigens critical for immune development, but is also susceptible to increased permeability that can lead to inflammation and allergies.
Q: How does the microbiome affect barrier function?
A: Early microbial colonization guides barrier maturation, immune education, and can impact brain development and risk for diseases like allergies and autism.
Q: What practices harm or help infant barrier function?
A: Gentle skin care, adequate hydration, breastfeeding, and controlled environmental exposures support barrier development, while harsh chemicals, excessive hygiene, and early antibiotics may disrupt maturation.
Q: Are preterm infants at greater risk for barrier dysfunction?
A: Yes, preterm infants have underdeveloped skin and gut barriers, making them more susceptible to dehydration, infections, and allergic sensitization.
References
- https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2022.815885/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8880311/
- https://onlinelibrary.wiley.com/doi/full/10.1002/clt2.12043
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.01153/full
- https://publications.aap.org/neoreviews/article/10/4/e180/88333/The-Intestinal-Immune-Barrier
Read full bio of medha deb












