Oral Contraceptives and Gut Barrier Permeability: Exploring Connections, Mechanisms, and Health Implications
Emerging research shows hormonal birth control can compromise intestinal integrity.
Oral Contraceptives and Gut Barrier Permeability Link
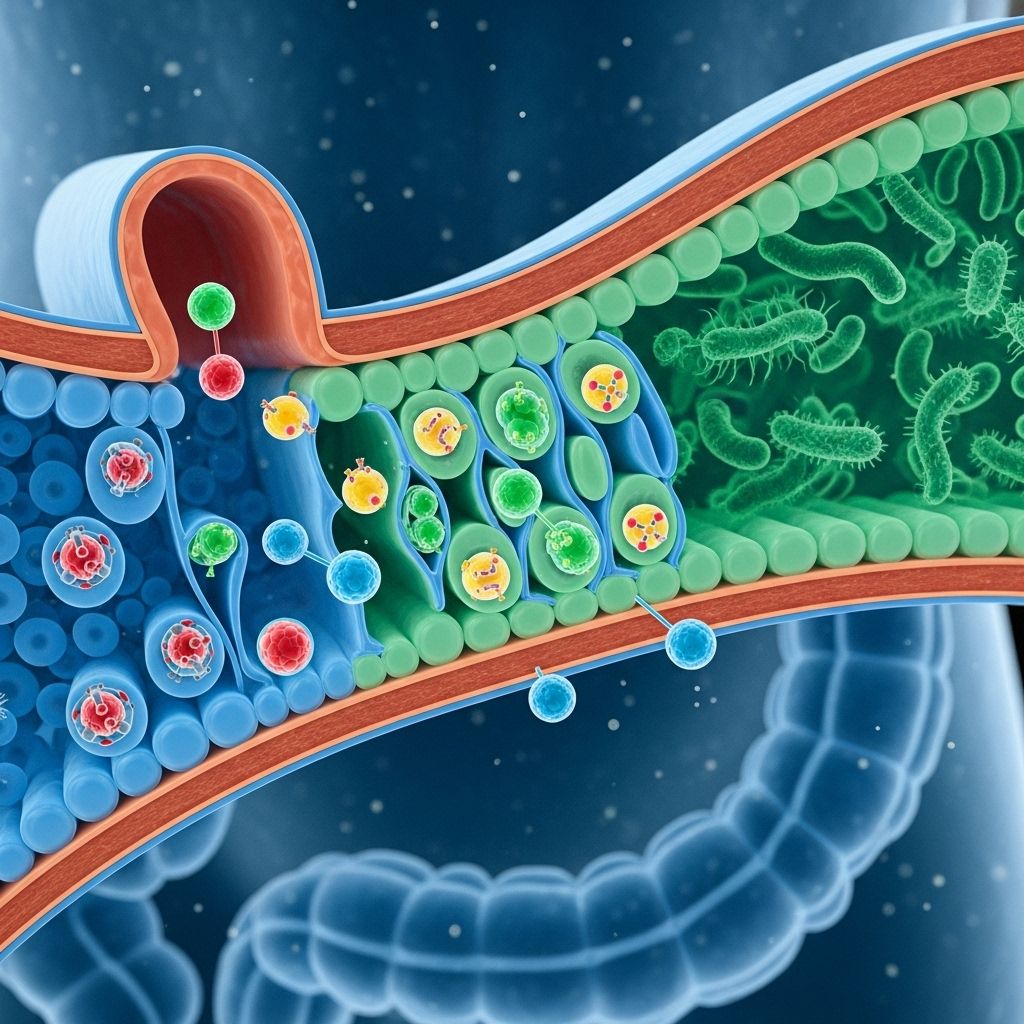
Oral contraceptives (OCs), especially combined oral contraceptives (COCs) containing estrogen and progestin, are widely used for birth control and menstrual regulation. The past decade has seen growing interest and concern regarding how OCs may interact with gastrointestinal health, specifically gut barrier permeability—the ability of the intestines to regulate which substances cross from the digestive tract into the bloodstream. This article provides a comprehensive review of existing evidence, mechanisms, health outcomes, and practical implications surrounding the connection between OCs, gut barrier permeability, and related health risks.
Table of Contents
- Introduction: Oral Contraceptives and Gut Health
- Key Mechanisms: How OCs Affect Gut Barrier Permeability
- OCs and the Gut Microbiome
- Intestinal Permeability and ‘Leaky Gut’
- Oral Contraceptives and Inflammatory Bowel Disease
- The Gut-Brain Axis: Mental Health Implications
- Clinical and Epidemiological Evidence
- Risk Factors and Susceptible Populations
- Practical Implications for Women’s Health
- Frequently Asked Questions
- Conclusion: Summary and Future Directions
Introduction: Oral Contraceptives and Gut Health
Oral contraceptives are among the most commonly prescribed medications for women worldwide. While their primary role is in preventing pregnancy and regulating menstrual cycles, research is increasingly exploring their broader physiological effects—including impacts on the immune system, hormone regulation, and gastrointestinal health. The emerging evidence indicates that COCs may alter the composition and function of the gut microbiota and influence the permeability of the intestinal barrier, possibly contributing to both digestive and neuropsychiatric conditions.
Key Mechanisms: How OCs Affect Gut Barrier Permeability
Several mechanisms have been proposed to explain the link between oral contraceptives and gut barrier permeability:
- Hormonal Modulation: OCs introduce exogenous estrogen and progestin, influencing the hormonal balance in the gut environment. Estrogen is known to affect immune responses and cellular proliferation within the intestinal wall, potentially altering how tightly the intestinal cells are joined together.
- Microbiome Dysbiosis: The hormone-altering effects of OCs can disrupt the normal balance of gut bacteria, which themselves play a role in maintaining barrier function.
- Immune System Activation: Changes in gut permeability allow inflammatory signals and microbial products to cross into the bloodstream, triggering immune responses that can further compromise gut integrity.
- GI Barrier Function Differences: Clinical studies using sugar absorption tests show users of COCs have higher ratios (lactulose-to-rhamnose excretion) indicating increased intestinal permeability compared to non-users.
OCs and the Gut Microbiome
The gut microbiome is the complex ecosystem of bacteria, viruses, and fungi that inhabit the digestive tract. Oral contraceptives—especially those containing estrogen—can disrupt the composition and diversity of this microbiome:
- Reduced Diversity: Some studies reveal that women using hormonal contraceptives have decreased diversity and abundance of beneficial bacterial species compared to non-users, though overall diversity changes are modest.
- Functional Alterations: Even when overall bacterial composition remains unchanged, functional differences such as metabolic activity and neurotransmitter production can be observed.
- Microbial Hormone Modulation: Bacteria in the gut are involved in metabolizing and modulating endogenous hormones such as estrogen and testosterone, and altered microbial balance can feedback to impact hormone levels systemically.
These changes in microbiome can have downstream consequences:
- Compromised gut barrier function (‘leaky gut’)
- Altered immune system activation
- Gut-brain axis disruptions affecting mental health
Intestinal Permeability and ‘Leaky Gut’
Gut barrier permeability refers to the ability of the intestinal lining to selectively allow nutrients to pass while blocking potentially harmful substances (toxins, microbes, large molecules). Increased permeability—commonly called ‘leaky gut’—means the barrier is compromised. Oral contraceptives are associated with heightened permeability:
- Sugar Absorption Findings: Dual sugar absorption techniques show elevated lactulose-to-rhamnose excretion in users of COCs, indicative of greater permeability.
- Inflammatory Pathways: Increased permeability can lead to the passage of bacteria, bacterial products, and antigens into the bloodstream, stimulating inflammation that is implicated in diseases like Crohn’s disease (CD) and ulcerative colitis (UC).
- Role of Estrogen: Effects appear to be most pronounced with estrogen-containing contraceptives, not with progestin-only pills.
This permeability contributes to a cascade of potential health risks, particularly when coupled with genetic or environmental susceptibility.
Oral Contraceptives and Inflammatory Bowel Disease
The link between OC use and increased risk of inflammatory bowel diseases (IBD), particularly Crohn’s disease and ulcerative colitis, is supported by epidemiological and clinical studies:
| Condition | Degree of Risk with OC Use | Notes |
|---|---|---|
| Crohn’s Disease (CD) | Up to 50% increased risk; higher with longer use; risk diminishes upon discontinuation | Meta-analyses and large cohort studies confirm increased CD risk |
| Ulcerative Colitis (UC) | Modest increased risk, but not statistically significant after adjusting for smoking | Evidence less consistent for UC than CD |
OC use is linked not only to increased disease risk, but also worse outcomes (e.g., increased risk of surgery among women with established CD). The biological plausibility stems from the leaky gut pathway due to barrier disruption and subsequent inflammation.
The Gut-Brain Axis: Mental Health Implications
The gut-brain axis describes the bidirectional communication between the gastrointestinal tract and the central nervous system. Recent evidence suggests a possible connection between COC-induced gut changes and mental health complications:
- Microbiome Disruptions: Alterations in gut bacteria can affect neurotransmitter production (such as serotonin), which in turn may impact mood and anxiety.
- Inflammatory Signaling: Increased permeability facilitates inflammatory signals reaching the brain, possibly contributing to conditions such as anxiety and depression.
- Epidemiological Associations: Some studies suggest increased risk of depression in adolescent and adult COC users.
This area of research is evolving rapidly, and more studies are needed to determine the extent and clinical relevance of these neuropsychological effects.
Clinical and Epidemiological Evidence
- Longitudinal Clinical Trials: A 3-point longitudinal study with healthy women initiating OC use noted marginal, but not significant, changes in the gut microbiome—although changes in gut function were present.
- Sugar Absorption Studies: Studies using sugar excretion ratios confirm increased permeability in users of COCs compared with non-users and men.
- Prospective Cohort Studies: Large cohort studies (Nurses’ Health Study) reinforce the increased risk of Crohn’s disease with prolonged and current OC use.
- Discontinuation Effects: Disease risk declines or reverses upon cessation of OC use.
Most current evidence points to estrogen-containing OCs (combination pills) as the main contributor to these effects, with progestin-only pills showing little or no similar impact.
Risk Factors and Susceptible Populations
Not all women using OCs will experience significant changes in gut barrier function or resulting health problems—certain populations and circumstances may heighten susceptibility:
- Genetic Predisposition: Family history of IBD or autoimmune diseases may increase vulnerability.
- Duration and Type of OC Use: Longer use and estrogen-containing formulations amplify risk.
- Other Medications or Lifestyle Factors: Antibiotic use, poor dietary habits, smoking, and chronic stress can worsen gut barrier integrity.
- Age and Hormonal Status: Adolescents and perimenopausal women may be more sensitive to hormonal disruptions.
Practical Implications for Women’s Health
Given the possible health consequences, women and their healthcare providers should take practical steps:
- Risk Assessment: Consider family and personal history of IBD, autoimmune, and mental health disorders before starting OCs.
- Monitor Symptoms: Be vigilant for changes in digestive function, persistent abdominal symptoms, or mood disturbances after starting OCs.
- Alternative Methods: For high-risk individuals, progestin-only pills or non-hormonal contraceptive options may be considered.
- Diet and Lifestyle: Supporting gut health through diet (fiber-rich foods, fermented products), regular physical activity, and stress management can be beneficial.
- Open Dialogue: Discuss side effects and concerns with healthcare providers for personalized contraceptive planning.
Frequently Asked Questions (FAQs)
Q: Do all oral contraceptives affect gut permeability?
No. Evidence suggests estrogen-containing combined oral contraceptives have a greater effect on gut permeability compared to progestin-only pills.
Q: Is the risk of IBD permanent with OC use?
Risk increases with duration of use but diminishes or disappears after discontinuation of OCs.
Q: Can OCs cause mental health problems?
Recent studies indicate changes in the gut microbiome and permeability due to OCs may contribute to depression and mood disorders, though causality for each individual remains to be established.
Q: What symptoms indicate a leaky gut?
Common signs include persistent digestive discomfort, unexplained fatigue, food sensitivities, and frequent inflammatory symptoms. Consult a clinician if these occur after starting OCs.
Q: How can women minimize these risks?
Discuss family history with your provider, consider non-estrogen options, support gut health with diet and lifestyle, and monitor for changes in digestive or mental health after beginning OCs.
Conclusion: Summary and Future Directions
The relationship between oral contraceptives and gut barrier permeability is an evolving field in women’s health. Current evidence supports that estrogen-containing OCs can increase intestinal permeability, alter gut microbiome composition and function, and contribute to higher risk of digestive and neuropsychiatric conditions in susceptible individuals. More research is needed to unravel the underlying biological mechanisms, quantify risks in different populations, and inform clinical practice for contraceptive counseling and gut health preservation.
Healthcare providers and patients should remain informed about potential GI and mental health effects of OCs and use ongoing monitoring and personalized decision-making to optimize outcomes.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12034237/
- https://www.cureus.com/articles/350221-estrogen-gut-brain-axis-examining-the-role-of-combined-oral-contraceptives-on-mental-health-through-their-impact-on-the-gut-microbiome.pdf
- https://naturalwomanhood.org/gut-estrogen-brain-connection/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4752384/
- https://clinicaltrials.gov/ct2/show/NCT06089811
- https://mybioma.com/en/blogs/science/how-the-pill-affects-your-gut-microbiome-what-you-should-know
- https://www.contemporaryobgyn.net/view/how-birth-control-pills-may-impact-mood-through-the-gut-brain-axis
Read full bio of Sneha Tete












