Ocular Epithelium Barrier Function and Eye Health: Cellular Defenses, Disorders, and Healing
Surface defenses of the cornea and conjunctiva ensure clarity and enable natural repair.
The surface of the eye, continuously exposed to the external environment, relies on a multi-layered epithelial barrier as its first line of defense. This highly specialized structure plays a fundamental role in protecting against physical, chemical, and microbial insults, ensuring visual clarity and overall ocular health. Disruption of this barrier is linked to a range of eye disorders, making its integrity crucial for maintaining the health of the eye.
Table of Contents
- Introduction to the Ocular Epithelium and Its Barrier Function
- Anatomy of the Ocular Epithelium
- Cellular and Molecular Components of the Barrier
- Functional Roles of the Epithelial Barrier
- Regulation of Barrier Integrity
- Barrier Dysfunction and Eye Disorders
- Barrier Repair and Regeneration
- Clinical Implications and Future Directions
- Frequently Asked Questions (FAQs)
Introduction to the Ocular Epithelium and Its Barrier Function
The ocular epithelium encompasses the corneal and conjunctival epithelia—multi-layered cellular barriers that face constant challenges from the environment. As the outermost tissue, the epithelium shields the eye from mechanical trauma, microbial invasion, desiccation, and toxic substances. Its strategic structure and biochemical properties make it indispensable for preserving vision and comfort.
The efficiency of the ocular barrier directly relates to its capacity to uphold surface integrity, support tear film stability, and orchestrate immune defense responses. Breakdowns in this barrier are strongly associated with surface inflammation, infection, and several chronic ocular surface diseases.
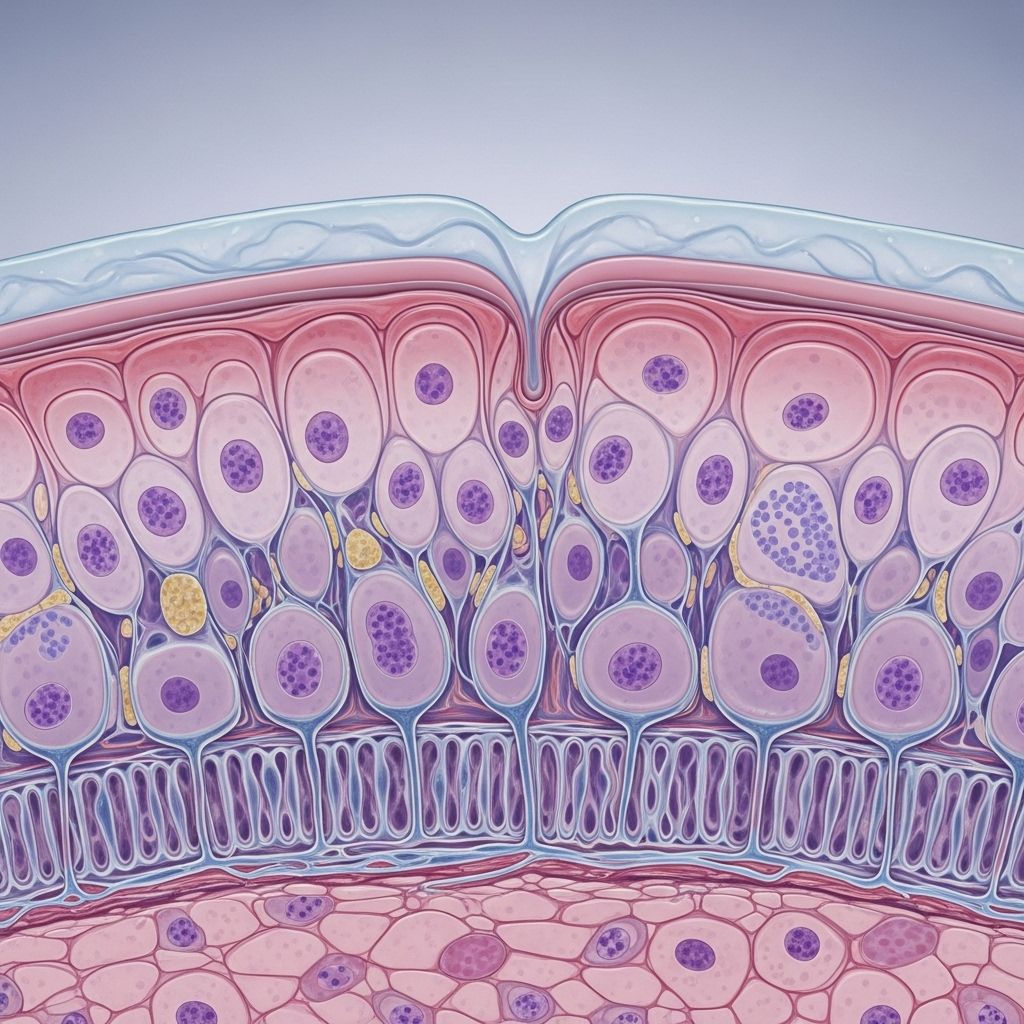
Anatomy of the Ocular Epithelium
The ocular surface comprises two key epithelial types:
- Corneal Epithelium: The transparent, non-keratinized, stratified squamous epithelium covering the central eye. It consists of 5–7 cell layers in humans.
- Conjunctival Epithelium: Lines the inner surface of the eyelids and extends onto the sclera. It has 2–5 cell layers and contains specialized goblet cells that secrete mucins.
Both epithelia are supported by an underlying basement membrane that provides structural support and regulates cell behavior. The corneal epithelium is particularly crucial due to its transparency, avascularity, and regenerative ability.
Corneal Epithelium Stratification
- Superficial (Apical) Cells: Equipped with microvilli and produce surface mucins, forming the interface with the tear film.
- Wing Cells: Intermediate layers, rich in desmosomes, providing tensile strength.
- Basal Cells: Proliferative, attached to the basement membrane by hemidesmosomes, and serve as progenitors for cell renewal.
Key Distinctions
| Feature | Corneal Epithelium | Conjunctival Epithelium |
|---|---|---|
| Cell Layers | 5–7 | 2–5 |
| Transparency | Transparent | Non-transparent |
| Specialized Cells | None | Goblet cells (mucin production) |
| Main Function | Structural barrier and optics | Mucosal immunity and lubrication |
Cellular and Molecular Components of the Barrier
The effectiveness of the ocular epithelial barrier is a result of highly coordinated intercellular junctions and a specialized surface glycocalyx.
Intercellular Junctional Complexes
- Tight Junctions (Zonula Occludens): Located at the apical-most layer. Assemble from proteins like claudins, occludin, and junctional adhesion molecules, supported by adaptor proteins such as ZO-1. These junctions seal the spaces between cells, thus blocking paracellular diffusion of molecules, allergens, and pathogens.
- Desmosomes (Macula Adherens): Provide robust links between cells, maintaining tissue integrity under shear forces—abundant in wing cell layers.
- Adherens Junctions (Zonula Adherens): Facilitate strong adhesion throughout the epithelium, linking cytoskeletal filaments between adjacent cells.
- Hemidesmosomes: Anchor the basal epithelial cells to the basement membrane, vital for epithelial cohesion and re-epithelialization after injury.
- Gap Junctions: Permit intercellular communication and coordinate responses for wound healing, particularly prevalent in basal layers.
Apical Barrier: The Glycocalyx
The superficial epithelial cells are covered by an extensive glycocalyx, composed of heavily O-glycosylated transmembrane mucins (notably MUC1, MUC4, and MUC16). These mucins repel pathogens and particulates, minimize cell adhesion by microbes, and retain tear film stability. MUC16, one of the largest known mucins, is indispensable for surface protection—the loss of its expression leads to barrier disruption and increases susceptibility to infection.
Carbohydrate-binding proteins, such as galectin-3, interact with mucins’ carbohydrate residues, forming multivalent glycoprotein complexes. These complexes further reinforce the physical apical barrier and restrict transcellular passage of potential hazards.
Functional Roles of the Ocular Epithelial Barrier
The ocular epithelial barrier serves several related but distinct physiological functions:
- Physical Barrier: Blocks the entry of pathogens, allergens, and toxic substances, preventing them from accessing deeper tissues.
- Immune Barrier: Regulates innate and adaptive immune responses, acts as a source of antimicrobial peptides, and participates in early defense against infection and inflammation.
- Tear Film Maintenance: Supports tear film adherence and stability, thereby protecting against desiccation and frictional damage.
- Transparency and Optics: In the cornea, the barrier maintains a smooth optical surface and contributes to light refraction needed for vision.
- Cellular Homeostasis: Maintains a controlled environment for the epithelial cells and regulates molecular and cellular turnover for healing.
Regulation of Barrier Integrity
Barrier function is tightly regulated at the genetic, molecular, and cellular levels. Proper expression and localization of junctional proteins, mucins, and supporting factors are critical to maintaining barrier strength.
Transcriptional Regulation
- Krüppel-like Factor 4 (KLF4): A master transcription factor essential for maintaining corneal epithelial barrier integrity. KLF4 upregulates key cell junction proteins, including those forming tight junctions and the basement membrane, thereby bolstering the epithelial defense.
Disruption or knockout of KLF4 expression impairs cell junction assembly, decreasing barrier functionality and increasing susceptibility to inflammatory and infectious ocular surface diseases.
External and Internal Factors
- Tear Film Components: Supply nutrients, growth factors, and antimicrobial peptides; continuous removal of debris and pathogens.
- Innate Immune System: Signals epithelial repair, regulates inflammation, and produces defensins and lysozyme as chemical barriers.
- Cell Signaling Pathways: Coordinate cell proliferation, differentiation, and wound healing response.
Barrier Dysfunction and Eye Disorders
Compromise of the ocular epithelial barrier function can have immediate and long-term impacts on eye health, resulting in a range of ocular surface diseases and increasing the risk for deeper tissue damage.
Major Conditions Related to Barrier Dysfunction
- Dry Eye Disease: Loss of surface mucins or disruption in tear film stability leads to desiccation, inflammation, and epithelial breakdown.
- Allergic Eye Disease: Chronic exposure to allergens can impair tight junctions and mucins, facilitating allergen penetration and triggering immune overactivation. This is central to the pathophysiology of allergic conjunctivitis and vernal keratoconjunctivitis.
- Infectious Keratitis: Weakened barriers increase susceptibility to pathogens like bacteria (e.g., Pseudomonas aeruginosa, Staphylococcus aureus), viruses, and fungi, especially in contact lens wearers or following trauma.
- Autoimmune Diseases: Disorders such as ocular cicatricial pemphigoid result in scarring and breakdown of epithelial integrity.
- Genetic and Dystrophic Disorders: Elevated risk of corneal epithelial barrier incompetence is noted in Meesmann’s dystrophy and other genodermatoses affecting structural proteins.
Consequences of Barrier Breakdown
- Increased pathogen penetration and infection risk
- Enhanced ocular inflammation and discomfort
- Greater risk of chronic eye surface disease
- Delayed wound healing and persistent epithelial defects
- Loss of corneal transparency and reduced visual acuity
Barrier Repair and Regeneration
The ocular surface exhibits robust repair mechanisms to restore barrier function following injury. Recent research highlights the orchestration of cell migration, proliferation, and differentiation:
- Limbal Stem Cells: Located at the corneal periphery, these are vital for renewal and repair of the corneal epithelium.
- Cell Migration: Damaged cells are rapidly replaced by migratory surrounding cells closing the wound gap.
- Cell Proliferation: Basal cells divide to supply new epithelial layers.
- Junction Reassembly: Formation and maturation of new intercellular junctions restore barrier properties.
- Growth Factor Signaling: Factors in the tear film and stroma stimulate wound healing, including EGF, HGF, and others.
Persistent or repeated injury, or deficiencies in stem cells, may lead to non-healing defects, scarring, or increased infection risk.
Clinical Implications and Future Directions
Understanding the core biology of ocular epithelial barrier function informs both clinical management and therapeutic innovation. Restoration of the barrier is a key goal in treating eye surface diseases and preventing vision loss.
Diagnostic Applications
- Vital Dye Testing: Use of dyes (e.g., fluorescein, lissamine green) helps highlight barrier disruption and epithelial defects in clinical exams.
- Molecular Markers: Assays for mucins, tight junction proteins, and inflammatory cytokines are under investigation for diagnosis and monitoring.
Therapeutic Strategies
- Artificial Tears and Lubricants: Support tear film and protect apical cells in dry eye.
- Anti-inflammatory and Immunomodulatory Agents: Restore immune homeostasis and limit epithelial barrier damage in allergies and autoimmune disease.
- Barrier Protectants: Emerging therapies that stabilize cell junctions or promote mucin production.
- Cell-based Therapies: Expansion of limbal stem cells to treat non-healing epithelial defects and persistent corneal injuries.
Continued research in genomics, proteomics, and regenerative medicine promises further advances in understanding and manipulating these critical ocular surface barriers for optimal eye health.
Frequently Asked Questions (FAQs)
Q: What is the most critical component of the ocular epithelial barrier?
A: The tight junctions at the apical corneal epithelium are often regarded as the primary barrier to pathogen entry and water loss, while apical mucins provide essential surface protection.
Q: How does the tear film interact with the epithelial barrier?
A: The tear film adheres to and is stabilized by the epithelial glycocalyx. It continuously removes debris and provides essential nutrients and antimicrobial factors, supporting both physical integrity and immune defense.
Q: What causes disruption of the epithelial barrier?
A: Disruption may result from trauma, chronic inflammation, infections, exposure to environmental toxins, genetic disorders affecting structural proteins, or immunological diseases.
Q: Can ocular epithelial barrier function be restored?
A: Yes, the barrier can usually regenerate after mild insults through rapid cell migration and proliferation, but chronic or severe damage may require clinical intervention, including medications or regenerative therapies.
Q: Why is the ocular epithelial barrier important for contact lens wearers?
A: Wearing contact lenses can alter tear film dynamics, disrupt epithelial tight junctions, and increase susceptibility to infection by enabling microorganism adhesion to the ocular surface.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3858173/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3101671/
- https://openophthalmologyjournal.com/VOLUME/9/PAGE/49/
- https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1384500/full
- https://onlinelibrary.wiley.com/doi/10.1111/all.15174
- https://iovs.arvojournals.org/article.aspx?articleid=2126520
Read full bio of Sneha Tete












