The Complex Interplay Between NAFLD and Cardiovascular Disease: Mechanisms, Risks, and Clinical Management
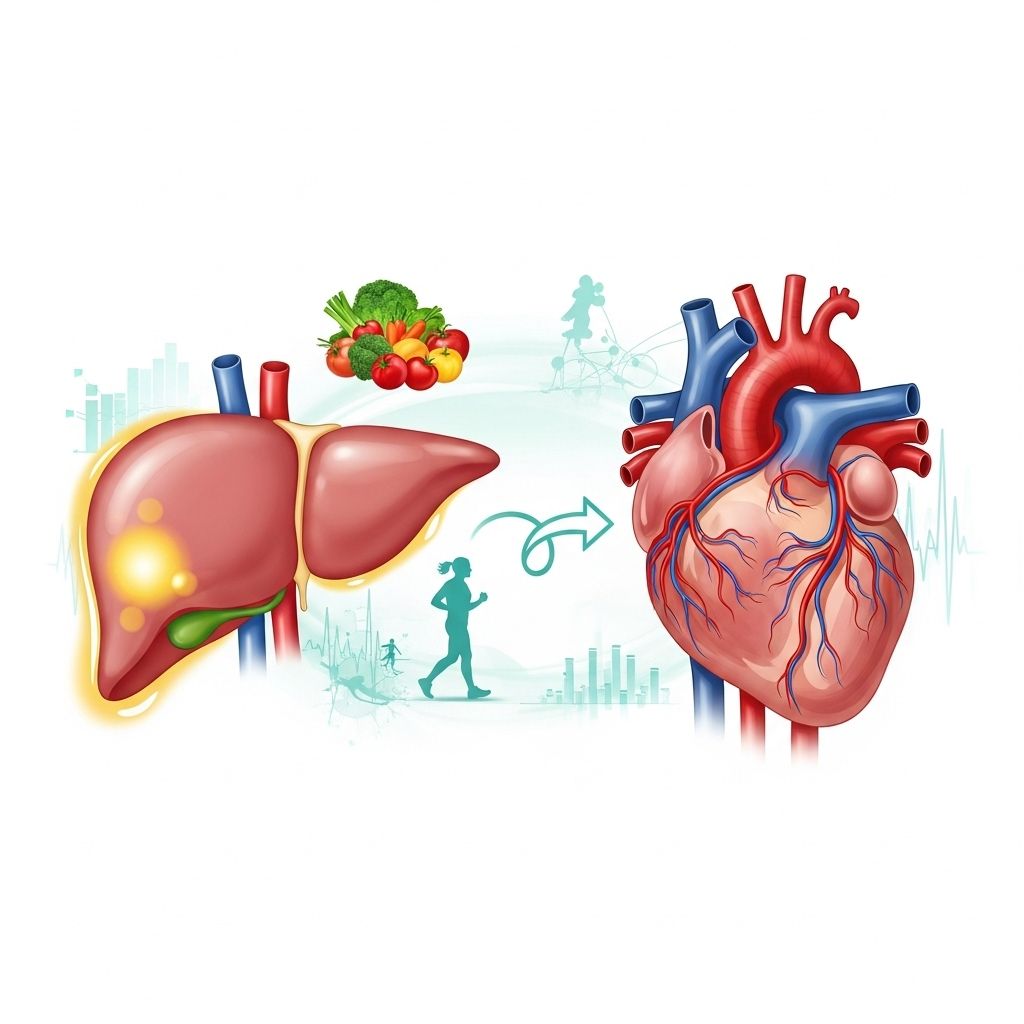
Combining liver care and heart health strategies can reduce risks across the body.
The Complex Interplay Between NAFLD and Cardiovascular Disease
Non-alcoholic fatty liver disease (NAFLD) is increasingly recognized as a key player not just in liver health, but also in the development and progression of cardiovascular disease (CVD). This article explores the intricate relationship between NAFLD and CVD, detailing pathophysiology, shared risk factors, clinical consequences, and best practices for risk management.
Table of Contents
- Introduction to NAFLD and CVD
- Pathogenesis of NAFLD
- Epidemiology and Burden
- Mechanisms Linking NAFLD and CVD
- Shared Risk Factors and Metabolic Syndrome
- Clinical Manifestations and Outcomes
- Diagnosis and Risk Stratification
- Management and Prevention Strategies
- Research and Future Directions
- Frequently Asked Questions (FAQs)
- References
Introduction to NAFLD and CVD
NAFLD describes a spectrum of liver pathology, ranging from simple fat accumulation in the liver (hepatic steatosis) to inflammation (non-alcoholic steatohepatitis, or NASH), with progression possible toward liver fibrosis, cirrhosis, and even hepatocellular carcinoma. Importantly, only a fraction of those with NAFLD advance to severe liver complications, but the condition carries significant systemic risks, most notably for cardiovascular health. In fact, cardiovascular disease has become the leading cause of death in individuals with NAFLD, outpacing liver-related mortality.
Pathogenesis of NAFLD
The development of NAFLD is closely related to the modern epidemic of obesity and metabolic syndrome. Its pathology involves:
- Excess calorie intake and sedentary lifestyle leading to hepatic fat accumulation.
- Insulin resistance that promotes hepatic lipogenesis and impairs lipid export from the liver.
- Oxidative stress and inflammation from fat overload, triggering liver cell injury.
- Progression to NASH when inflammation and cellular injury accompany steatosis.
- Potential evolution into advanced fibrosis or cirrhosis if damage persists.
NAFLD is considered the hepatic manifestation of metabolic syndrome, closely tied to disorders such as type 2 diabetes mellitus, dyslipidemia, and hypertension.
Epidemiology and Burden
NAFLD affects approximately 25% of adults in Western countries, with the prevalence rising globally. Key epidemiological highlights include:
- NAFLD incidence is increasing in tandem with rates of obesity and type 2 diabetes.
- While most patients do not progress beyond simple steatosis, many have significant comorbidities that increase cardiovascular risk compared to the general population.
- NAFLD is now viewed as a major component—and consequence—of the global metabolic disease burden.
Mechanisms Linking NAFLD and CVD
The relationship between NAFLD and CVD is multifactorial, involving a complex web of metabolic, inflammatory, and possibly genetic pathways. Key mechanisms include:
- Insulin resistance: Central to both NAFLD and CVD, it promotes excessive free fatty acids, dysglycemia, and hypertension.
- Dyslipidemia: Altered fat metabolism in NAFLD leads to increased triglycerides, low HDL cholesterol, and small, dense LDL particles—core drivers of atherosclerosis.
- Chronic inflammation: Fatty liver generates inflammatory cytokines (e.g., CRP, TNF-α, IL-6) that exacerbate systemic endothelial dysfunction and vascular disease.
- Oxidative stress: Imbalance between reactive oxygen species and antioxidants in NAFLD can damage vessels and worsen plaque instability.
- Endothelial dysfunction: Impaired vascular response increases risk for hypertension and thrombosis.
- Genetic and epigenetic factors: May predispose some individuals to both NAFLD and increased CVD risk.
Importantly, these mechanisms are not mutually exclusive and their interplay accelerates the atherogenic process.
Shared Risk Factors and Metabolic Syndrome
NAFLD and CVD share numerous modifiable and non-modifiable risk factors:
- Obesity: Particularly central (visceral) adiposity, increases hepatic fat and cardiovascular strain.
- Type 2 diabetes mellitus (T2DM): Strongly linked to NAFLD and a powerful predictor of CVD.
- Dyslipidemia: Elevated triglycerides, low HDL, and increased LDL.
- Hypertension: Both a cause and effect of disrupted metabolic processes in NAFLD.
- Genetics: Some familial clustering hints at marginal polygenic risk.
The clustering of these features defines the metabolic syndrome. NAFLD is often considered its hepatic expression—reflecting and reinforcing cardiovascular morbidity risk.
Clinical Manifestations and Outcomes
Cardiovascular involvement in NAFLD can be:
- Subclinical: Early atherosclerosis, arterial stiffness, abnormal cardiac structure detectable by imaging.
- Clinical: Higher rates of:
- Atherosclerotic cardiovascular disease (ASCVD)
- Coronary artery disease
- Heart failure (especially with preserved ejection fraction—HFpEF)
- Cardiac arrhythmias, e.g., atrial fibrillation
- Cerebrovascular disease (stroke)
- Peripheral arterial disease
In NAFLD, particularly NASH and advanced fibrosis, the risk of adverse cardiovascular events rises strikingly, with odds ratios up to 2–4 for subclinical markers of atherosclerosis. Notably, in NAFLD patients, cardiovascular disease accounts for the vast majority of excess mortality, exceeding deaths due to end-stage liver disease.
NAFLD and Atherosclerosis: The Evidence
| Manifestation | Association with NAFLD |
|---|---|
| Carotid artery intima-media thickness | OR 1.74 (increased thickening or plaque) |
| Arterial stiffness | OR 1.56 (more rigid vessels) |
| Coronary artery calcification | OR 1.40 (calcified plaques—subclinical CAD) |
| Endothelial dysfunction | OR 3.73 (severe impairment) |
Diagnosis and Risk Stratification
NAFLD is most often detected incidentally by imaging or elevated liver enzymes in patients with metabolic risk factors. Key diagnostic steps include:
- Liver ultrasound or elastography: Non-invasive detection of hepatic steatosis or fibrosis.
- Exclusion of secondary causes: Rule out other liver disease (viral hepatitis, alcohol overuse).
- Fibrosis scoring systems: Use of FIB-4, NAFLD fibrosis score, or transient elastography to assess progression risk.
Once NAFLD is identified, a comprehensive evaluation of CVD risk is warranted:
- Screen for diabetes, hypertension, and dyslipidemia.
- Assess for signs of subclinical atherosclerosis: e.g., coronary artery calcium score or carotid intima-media thickness (when indicated).
- Integrate hepatic and cardiovascular risk into individualized management.
Management and Prevention Strategies
Given the strong links between NAFLD and CVD, an integrated management approach is crucial. Strategies include:
1. Lifestyle Modification
- Encourage weight loss (7–10% reduction shown to reverse hepatic steatosis in many patients).
- Dietary interventions: Emphasis on Mediterranean or DASH-style patterns, minimizing simple sugars and saturated fats.
- Physical activity: 150+ minutes/week of moderate-intensity aerobic exercise.
2. Treating Metabolic and Cardiovascular Risk Factors
- Optimize glycemic control in diabetes using agents with cardiovascular benefit (e.g., SGLT2 inhibitors, GLP-1 agonists).
- Manage hypertension and dyslipidemia per guidelines (statins are safe in most cases of NAFLD).
- Address other contributors: Smoking cessation, blood pressure control, and sleep apnea screening.
3. Pharmacological Therapies for NAFLD
- Currently, no medication is approved specifically for NAFLD, but some diabetes drugs show benefit in NASH.
- Ongoing clinical trials are exploring agents that target key metabolic and inflammatory pathways.
4. Regular Screening and Multidisciplinary Care
- Monitor at-risk patients for both liver disease progression and cardiovascular morbidity.
- Collaboration between hepatology, endocrinology, cardiology, and primary care is often needed.
Research and Future Directions
- Further research is needed to unravel the genetic and molecular links between NAFLD and CVD.
- Development of robust non-invasive markers for both liver and cardiovascular risk.
- New therapies targeting not just steatosis but systemic inflammation and oxidative stress.
- Population-level interventions (public health) to address root causes—sedentary lifestyles, diet, and obesity.
Frequently Asked Questions (FAQs)
Q: Does everyone with fatty liver develop heart disease?
A: No, but all individuals with NAFLD are at higher risk for CVD, especially those with additional metabolic risk factors or advanced liver fibrosis. Not everyone with NAFLD will experience cardiovascular events, but their overall risk is elevated compared to healthy controls.
Q: How is NAFLD detected in patients at risk for heart disease?
A: Usually through imaging (ultrasound, CT, or MRI) or abnormal liver tests in people with obesity, diabetes, or metabolic syndrome. Further evaluation for fibrosis or progression, as well as cardiovascular risk stratification, is important.
Q: Are statins safe for patients with NAFLD?
A: Statins are generally safe and effective for lipid lowering in NAFLD, with large trials showing no increase in serious liver side effects. They are recommended when indicated to reduce cardiovascular risk.
Q: What lifestyle changes are most effective for both NAFLD and cardiovascular protection?
A: Weight loss through healthy diet and regular physical activity (preferably aerobic), along with management of blood sugar, blood pressure, and cholesterol, are the most effective interventions.
Q: Can treating NAFLD reverse heart disease risk?
A: While NAFLD regression can reduce risk, best outcomes come from addressing all metabolic components concurrently. Early detection and multidisciplinary management are key.
References
- PubMed Clinical Review: NAFLD and cardiovascular diseases.
- Times of India health article: Heart diseases caused by fatty liver.
- European Cardiology Review: Management of CVD in NAFLD.
- American College of Cardiology: Non-Alcoholic Fatty Liver Disease and cardiovascular risk.
References
- https://pubmed.ncbi.nlm.nih.gov/32696080/
- https://timesofindia.indiatimes.com/life-style/health-fitness/health-news/heart-diseases-caused-by-fatty-liver-understanding-the-link-between-metabolic-dysfunction-and-cardiovascular-health/articleshow/124310237.cms
- https://www.ecrjournal.com/articles/management-cardiovascular-risk-non-alcoholic-fatty-liver-disease-setting?language_content_entity=en
- https://www.acc.org/Latest-in-Cardiology/Articles/2022/07/13/14/58/Non-Alchoholic-Fatty-Liver-Disease
- https://pubmed.ncbi.nlm.nih.gov/30253056/
Read full bio of Sneha Tete












