Migraine Aura vs. Ocular Migraine: Comprehensive Symptom, Origin, and Treatment Comparison
Understanding distinct vision changes helps differentiate conditions and guide care.
Migraines are complex neurological conditions that can manifest a diverse range of symptoms. Among the most confusing types are migraine aura and ocular migraine. These phenomena both involve visual disturbances, but their origins, clinical implications, and management strategies differ significantly. This article delivers an in-depth, research-based comparison between migraine with aura and ocular migraine, equipping you with essential knowledge to distinguish and manage each condition effectively.
Table of Contents
- Introduction and Overview
- Definitions and Core Concepts
- Symptoms: Overlaps and Differences
- Visual Disturbances: A Closer Look
- Underlying Causes and Pathophysiology
- Prevalence, Risk Factors, and Demographics
- Diagnosis: How to Tell Them Apart
- Treatment and Management Strategies
- Complications and Prognosis
- Prevention and Lifestyle Modifications
- Migraine Aura vs. Ocular Migraine: At-a-Glance Table
- Frequently Asked Questions
- Conclusion
Introduction and Overview
Migraines are more than just severe headaches—they are often accompanied by a complex array of neurological symptoms. Two distinct yet often-confused types are migraine aura and ocular migraine, both of which can present dramatic visual phenomena. However, their location, causes, risk profiles, and management approaches are different.
Understanding these distinctions is crucial for ensuring accurate diagnosis and the best possible care.
Definitions and Core Concepts
- Migraine with Aura: Refers to a migraine that is preceded or accompanied by a group of transient neurological symptoms known as “aura,” with visual symptoms being the most common. The disturbance arises from temporary changes in brain function, particularly in the visual cortex, and typically affects both eyes simultaneously.
Prevalence: About 20-25% of migraine sufferers experience aura, often before the onset of headache. - Ocular Migraine (also called Retinal Migraine): Involves episodes of visual disturbance or vision loss in one eye only, generally resulting from temporary changes in retinal or ocular blood flow.
Prevalence: Much less common, affecting only about 0.5% (1 in 200) of all migraine patients.
Symptoms: Overlaps and Differences
Both conditions can present with strikingly similar visual phenomena, but their scope and associated symptoms differ:
- Visual Symptoms Common to Both:
- Flashes of light (photopsia)
- Zigzag patterns or fortification spectra
- Scintillating scotoma (twinkling or shimmering areas)
- Blind spots (scotomas)
- Shimmering or colored lights
- Distinct Features:
- Migraine with Aura: Visual symptoms occur in both eyes and originate in the brain. Other aura symptoms can include tingling (pins and needles), numbness, trouble speaking, or changes in sensation.
- Ocular Migraine: Visual changes occur in one eye only and may include complete or partial vision loss, dimming, blurring, or fading. Pain may or may not be present during the episode, but is often felt behind the affected eye.
Associated Headache and Systemic Symptoms
- Migraine with Aura: Headache typically follows the aura, lasting 4–72 hours and frequently accompanied by nausea, vomiting, or sensitivity to light and sound.
- Ocular Migraine: Headache may be simultaneous with, follow, or even be absent with the visual disturbance; when present, pain is usually localized behind the affected eye.
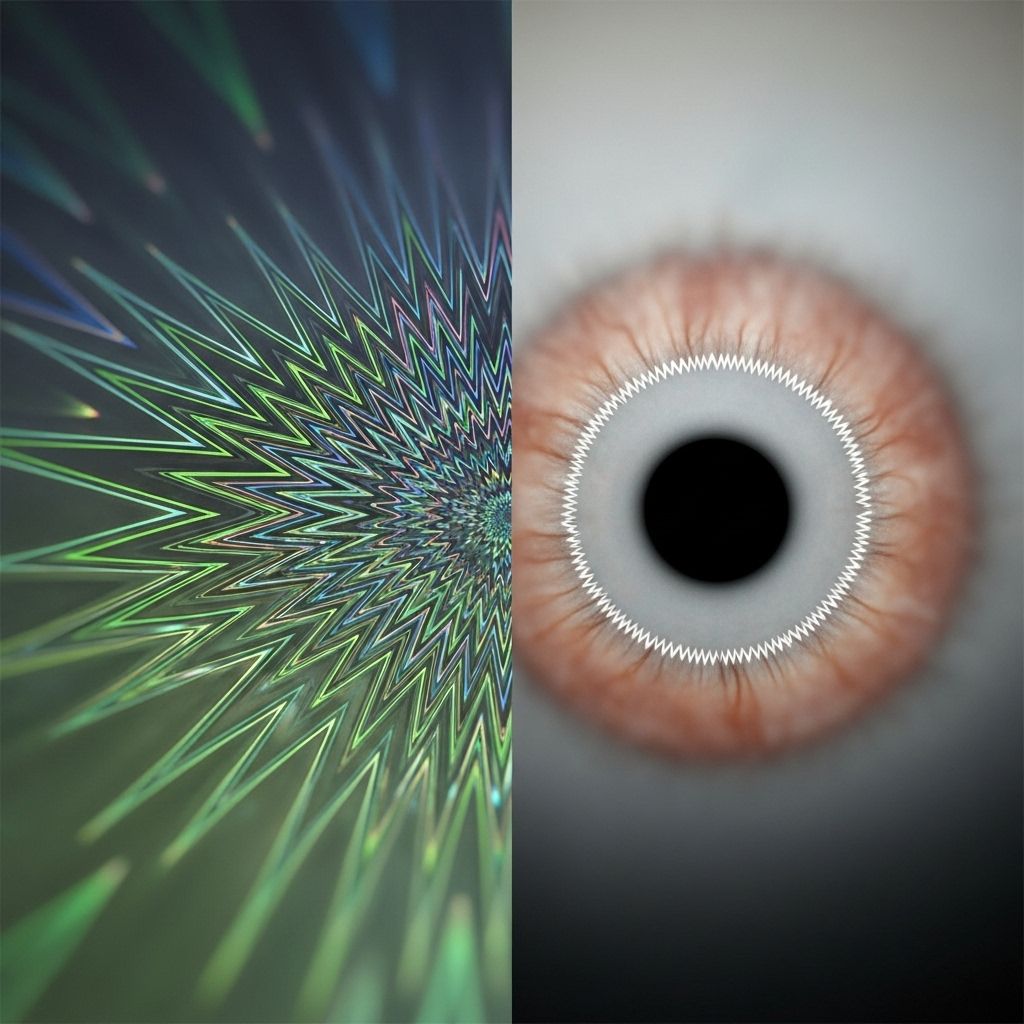
Visual Disturbances: A Closer Look
Visual disruptions are key to differentiating between these two migraine forms. Their nature, onset, and distribution are distinct:
| Feature | Migraine Aura | Ocular Migraine |
|---|---|---|
| Affected Area | Both eyes (usually the peripheral field) | One eye only (monocular) |
| Visual Patterns | Scintillating scotoma, fortification lines, bright spots | Blurring, dimming, central/partial vision loss, fading |
| Duration | 5–60 minutes (usually builds and recedes gradually) | Shorter on average (a few minutes to an hour), abrupt or gradual onset |
| Pain | Headache frequently follows; sometimes aura occurs without pain | Pain may be simultaneous, follow, or sometimes absent |
| Potential for Permanent Damage | Very rare, typically none | Very rare but possible permanent vision loss in the affected eye if attacks are severe/repeated |
Underlying Causes and Pathophysiology
- Migraine Aura: Caused by cortical spreading depression—a wave of electrical and chemical disturbance originating in the brain’s visual cortex. This leads to temporary altered nerve signaling and changes in blood flow, affecting both eyes. Triggers may include stress, hormonal fluctuations, certain foods, sensory stimulation, or sleep changes.
- Ocular Migraine: Linked to temporary changes in blood flow to the retina (retinal vasospasm), resulting in monocular visual symptoms. Triggers can overlap with those for migraine aura but occasionally involve cardiovascular risk factors.
Prevalence, Risk Factors, and Demographics
- Migraine Aura: About 8–25% of migraine sufferers, more common in women and those with a family history of migraine. Onset typically between ages 15-40.
- Ocular Migraine: Rare, affecting roughly 0.5% of migraineurs. May be more likely in people with vascular risk factors.
Diagnosis: How to Tell Them Apart
Accurate diagnosis is critical because the management and risks associated with each type can differ, especially regarding the eye’s health. Key considerations include:
- Laterality Test: During an episode, cover one eye. If the visual disturbance remains regardless of which eye is covered, it likely affects both eyes—suggesting migraine aura. If visual changes stop when one specific eye is covered, it is monocular and points to ocular migraine.
- Neuro-ophthalmological Examination: Needed to rule out other causes for vision loss, especially in monocular cases (e.g., retinal artery occlusion, optic neuritis, stroke).
- Patient History: Examining the pattern, frequency, triggers, and associated symptoms can help distinguish between the two types.
- Imaging Studies: Occasionally warranted to exclude serious neurological or ophthalmic conditions, particularly if episodes are atypical or progressive.
Treatment and Management Strategies
- Migraine Aura:
- Triggers should be identified and avoided.
- Acute attacks: Use of standard migraine treatments (NSAIDs, triptans, antiemetics as needed).
- Preventive medications: Considered for frequent or severe attacks (beta-blockers, anticonvulsants, anti-CGRP agents, tricyclic antidepressants).
- Maintain regular sleep, hydration, and stress management routines.
- Ocular Migraine:
- Immediate medical attention recommended for vision changes in one eye to exclude dangerous causes.
- Acute attacks: Rest in a dark, quiet environment; standard migraine medications if headache present; address cardiovascular risks if identified.
- Preventive medications and risk factor modification in recurrent cases (quit smoking, manage blood pressure etc.).
- In rare cases with ongoing vision loss, further work-up by an ophthalmologist or neurologist is mandatory.
Complications and Prognosis
- Migraine Aura: Prognosis is generally good; rarely linked to stroke and not associated with permanent visual loss. Aura without headache tends to increase with age.
- Ocular Migraine: While usually reversible, rare cases can lead to permanent vision deficit in the affected eye—especially if underlying vascular disease is present or if attacks are prolonged/recurrent.
Prevention and Lifestyle Modifications
- Monitor and avoid known triggers (certain foods, bright lights, dehydration, irregular sleep).
- Adopt a healthy diet rich in vegetables and whole grains; limit alcohol and caffeine.
- Practice regular exercise and stress-reduction techniques (yoga, mindfulness, biofeedback).
- For ocular migraine, work with your doctor to manage systemic and vascular risk factors (blood pressure, cholesterol).
Migraine Aura vs. Ocular Migraine: At-a-Glance Table
| Migraine with Aura | Ocular (Retinal) Migraine | |
|---|---|---|
| Origin | Brain’s visual cortex | Retina (eye) |
| Visual Disturbance | Both eyes | One eye |
| Frequency | 20–25% of migraine patients | 0.5% (1 in 200) of migraineurs |
| Typical Symptoms | Zigzag lines, scintillating scotoma, spreading visual field loss | Partial or complete visual loss, blurring, dimming |
| Duration | 5–60 minutes | Few minutes to 1 hour |
| Risk of Permanent Damage | Extremely rare | Potentially, if recurrent/severe |
| Other Symptoms | Tingling, speech/language trouble (aura); followed by headache, nausea, photophobia | Pain behind the affected eye, may or may not involve headache |
Frequently Asked Questions (FAQs)
Q: How can I quickly tell if I am having an ocular migraine or migraine with aura?
During a visual disturbance, cover one eye. If symptoms remain present in either eye, the likely culprit is migraine with aura (bilateral effect). If symptoms disappear when you cover one eye, it is likely an ocular migraine (monocular effect) and warrants immediate evaluation if it’s your first experience or if symptoms persist.
Q: Are ocular migraines dangerous?
Most cases are harmless and reversible, but rare instances can lead to permanent vision loss in the affected eye, especially with repeated or prolonged attacks. Always consult an eye specialist to rule out other causes for monocular vision changes.
Q: Can migraine aura occur without headache?
Yes. Some people experience migraine aura without subsequent headache (known as silent or acephalgic migraines, more common with increasing age).
Q: What triggers both migraine with aura and ocular migraines?
Trigger overlap is common: stress, certain foods (aged cheese, processed meats, wine), bright/flashing lights, hormonal changes, changes in sleep schedule, dehydration, and in ocular migraine, sometimes cardiovascular issues.
Q: Do both conditions require imaging or further workup?
Migraine with aura, when following a classic pattern, may not need imaging unless symptoms are new, changing, or atypical. Any first-time or recurrent monocular vision loss (ocular migraine) should be assessed urgently to rule out serious causes such as retinal artery occlusion.
Conclusion
Differentiating between migraine with aura and ocular migraine is essential for accurate management and prevention of complications. While they share many visual symptoms, their origin (brain versus retina), laterality (both eyes versus one eye), risk factors, and potential complications differ. Comprehensive evaluation—including a simple eye-covering test, a detailed medical history, and, when indicated, specialist work-up—is key to distinguishing these often-misunderstood entities, enabling tailored treatment to maximize both neurological and ocular health.
References
- https://www.allaboutvision.com/conditions/ocular-migraine/overview-of-retinal-migraine/
- https://coopervision.com/blog/difference-between-migraines-aura-and-ocular-migraines
- https://sydneymigraine.com.au/aura-vs-ocular-migraine/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7739549/
- https://www.henryford.com/Blog/2024/12/Retinal-Migraine
- https://eyeqvc.com/cataract/ocular-migraines-vs-migraine-auras/
- https://www.youtube.com/watch?v=NTBbRqv05Hg
- https://americanmigrainefoundation.org/resource-library/retinal-migraine/
Read full bio of medha deb












