Microbiome’s Role in Barrier Function: The Interplay Between Gut and Skin Health
A friendly microbe community fortifies inner defenses and sustains outer health.
The human body is host to trillions of microorganisms, forming complex communities known as microbiomes. Nowhere is their impact more critical than in the maintenance of barrier function, especially in the gut and skin. This article examines the role of the microbiome in fortifying these crucial barriers, explores the gut-skin axis, discusses implications for health and disease, and provides practical recommendations for preserving microbiome balance.
Table of Contents
- Understanding Barrier Function in Gut and Skin
- The Skin Microbiome and Barrier Integrity
- The Gut Microbiome and Intestinal Barrier
- How Microbiomes Influence the Barrier Function
- The Gut–Skin Axis: Communication Between Barriers
- Microbiome Dysbiosis and Disease
- Strategies to Support Microbiome Balance
- Frequently Asked Questions (FAQs)
- Conclusion
Understanding Barrier Function in Gut and Skin
Barrier function describes the body’s ability to protect internal tissues from environmental threats, regulate moisture, and maintain selective permeability. Both the gut and skin act as sentinels — front-line defenses against pathogens, toxins, and allergens. Crucially, they are both supported by resident microbiomes that play a vital part in this protective role.
| Barrier | Location | Principal Function | Microbiome Involvement |
|---|---|---|---|
| Intestinal | Gut lining | Absorb nutrients, block pathogens/toxins | Metabolite production, immune regulation, epithelial integrity |
| Skin | Epidermis/stratum corneum | Prevent water loss, block irritants/pathogens | Pathogen defense, lipid production, immune modulation |
The Skin Microbiome and Barrier Integrity
The skin microbiome represents a vast community of bacteria, fungi, viruses, and mites residing on human skin. Despite initial perceptions, not all microorganisms are harmful; in fact, many are crucial for preserving the skin barrier’s structure and function.
Key Functions of the Skin Microbiome
- Physical fortification: Healthy skin microbiota support the formation and maintenance of tight junctions in keratinocyte layers, reinforcing a nearly impermeable outer surface to prevent pathogen entry.
- Chemical defense: Resident microbes produce antimicrobial peptides (AMPs) and pH-lowering compounds, limiting the proliferation of harmful species.
- Lipid metabolism: Some skin bacteria (e.g., Staphylococcus epidermidis) secrete enzymes that generate ceramides, strengthening the lipid matrix and preventing moisture loss.
- Immune signaling: The microbiome helps calibrate local immune responses, enhancing the skin’s capacity to react to threats without triggering chronic inflammation.
- Wound healing: Microbial metabolites activate pathways (e.g., the aryl hydrocarbon receptor – AHR) critical for epithelial differentiation and regeneration.
Disruption of the Skin Barrier
If the microbiome is disturbed — through overuse of antibiotics, harsh cleansers, or underlying medical conditions — the integrity of the skin’s defensive wall can be compromised. This increases the risk for infections, delayed wound healing, water loss, and inflammatory conditions like eczema and psoriasis.
The Gut Microbiome and Intestinal Barrier
The gut microbiome comprises a diverse ecosystem of bacteria, viruses, fungi, and archaea along the gastrointestinal tract. This community exerts remarkable influence over digestion, nutrient synthesis, and immune system homeostasis.
How Gut Microbes Support the Intestinal Barrier
- Mucus layer regulation: Gut microbes stimulate mucus production, creating a protective buffer between intestinal epithelial cells and potential threats.
- Tight junction maintenance: Microbial metabolites help reinforce the proteins holding epithelial cells together, ensuring selective permeability.
- Immune training: Beneficial bacteria modulate immune cells (e.g., regulatory T cells or Tregs), promoting tolerance to harmless antigens and mounting defense against invaders.
- Short-chain fatty acid production: Fermentation of plant fibers yields SCFAs (such as butyrate), which play anti-inflammatory roles, fortify barrier integrity, and may even have protective effects for the skin.
Intestinal Barrier Dysfunction
Compromised gut barriers allow microbial fragments, toxins, and food antigens to enter circulation (“leaky gut”). This can incite systemic inflammation and is increasingly linked to dermatological diseases, allergies, and autoimmune disorders.
How Microbiomes Influence the Barrier Function
Both skin and gut microbiomes interact closely with their respective barriers, using several common and unique mechanisms:
- Metabolite production: Microbes generate bioactive compounds (like SCFAs, polysaccharide A, sphingomyelinases) that regulate junction formation, immune responses, and lipid synthesis.
- Competition with pathogens: Healthy commensals occupy attachment sites and secrete antimicrobial substances, reducing risk of infection.
- Immunity modulation: Continuous interaction with host cells teaches local and systemic immune systems to distinguish friend from foe, preventing overreaction.
- Regulation of inflammation: Balanced microbiomes calibrate cytokine levels and help resolve inflammation efficiently.
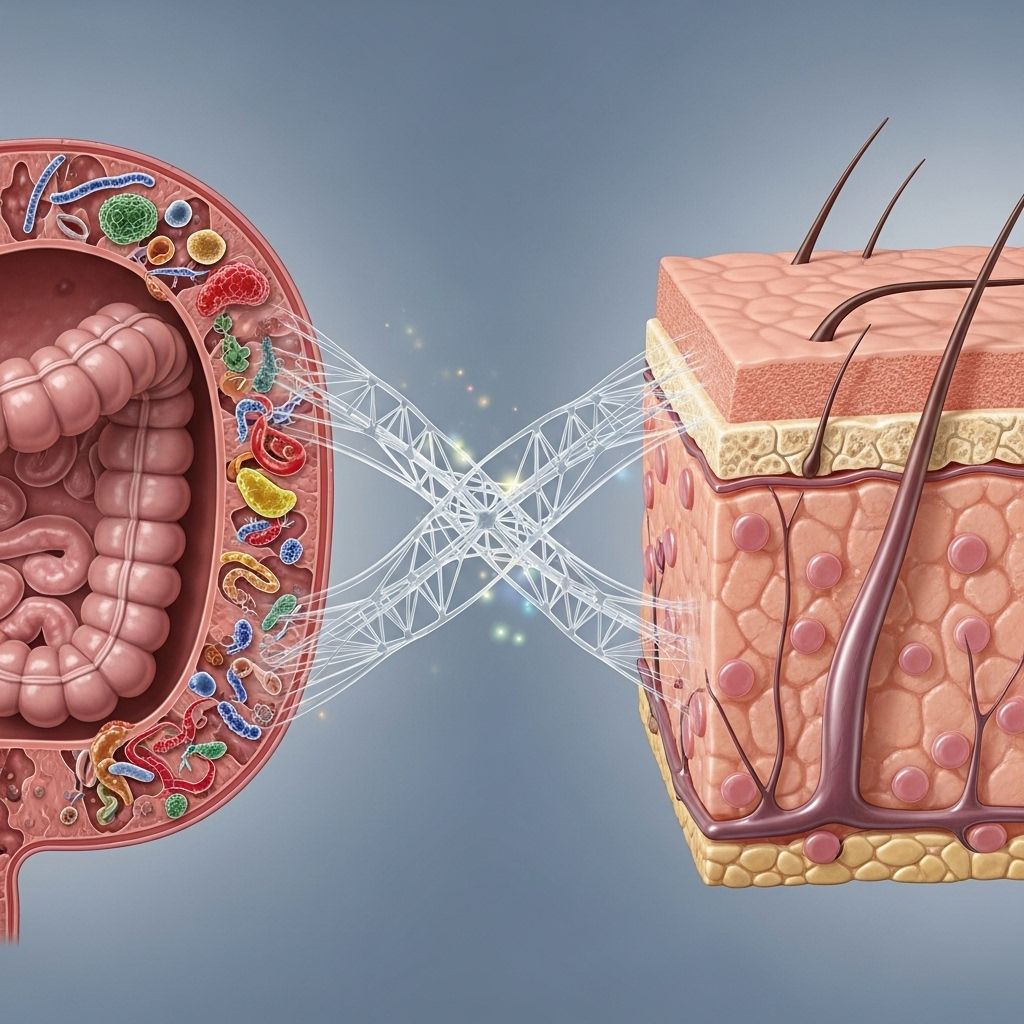
The Gut–Skin Axis: Communication Between Barriers
The concept of a gut-skin axis recognizes that gut and skin do not function in isolation: their microbiomes, immune systems, and barrier functions are intimately linked.
- Systemic immune signaling: Metabolites and immune cells influenced in the gut can affect inflammation and health of the skin, and vice versa. Gut-derived SCFAs, for instance, travel through the bloodstream and exert anti-inflammatory effects on the skin.
- Cross-barrier impact in disease: Gut microbiome disruptions are correlated with dermatological diseases (e.g., atopic dermatitis, acne, psoriasis). Conversely, skin injuries can alter gut microbial composition, heightening intestinal inflammation and colitis susceptibility, as shown in mouse models.
- Nutritional and dietary effects: Diets rich in fiber, prebiotics, and probiotics can benefit both gut and skin health by promoting a diverse, balanced microbiome.
Examples of the Gut–Skin Axis in Action
- Psoriasis patients frequently exhibit altered gut flora, with evidence of increased gut permeability (“leaky gut”), systemic inflammation, and worsened skin symptoms.
- Probiotics have shown therapeutic potential in alleviating eczema and atopic dermatitis by restoring intestinal microbial diversity.
Microbiome Dysbiosis and Disease
Dysbiosis — the imbalance or maladaptation of the microbiome — can have serious consequences for barrier function in both the gut and skin.
Links to Skin Conditions
- Atopic dermatitis (eczema): Lower skin microbial diversity and reduced protective species like S. epidermidis often coincide with higher colonization by pathogens (e.g., Staphylococcus aureus), weakening the skin barrier.
- Psoriasis: Dysbiosis in both gut and skin contributes to impaired barriers and elevated inflammatory signaling.
- Acne: Excess proliferation of certain bacteria (e.g., Cutibacterium acnes) and inflammation can damage the barrier and promote outbreaks.
Gut Barrier-Associated Diseases
- Inflammatory Bowel Disease (IBD): Reduced microbial diversity and decreased SCFA production are implicated in barrier disruption, immune overactivity, and relapsing inflammation.
- Food allergies and autoimmune disease: Leaky gut can allow allergens and immune-stimulating agents into circulation, predisposing to systemic disorders.
Strategies to Support Microbiome Balance
Improving or maintaining microbiome health can reinforce both gut and skin barriers. Consider these evidence-based approaches:
- Dietary diversity: Eating a wide range of plant-based foods provides fibers and polyphenols that nourish beneficial microbes.
- Probiotics and prebiotics: Supplementation with live beneficial bacteria (probiotics) and their food sources (prebiotics like inulin, oligosaccharides) can promote microbiome diversity and resilience, supporting barrier repair.
- Avoid unnecessary antibiotics: Judicious antibiotic use prevents accidental elimination of protective microbes.
- Gentle skin care: Use fragrance-free, pH-balanced skin products to avoid disturbing skin flora.
- Adequate sleep and stress reduction: Both factors modulate the microbiome via immune and hormone pathways and can help maintain robust barrier function.
Frequently Asked Questions (FAQs)
Q: How do gut microbes influence skin health?
A: Gut microbes produce metabolites (like SCFAs) and modulate immune signaling, directly affecting systemic inflammation, immune balance, and ultimately the health of the skin barrier.
Q: Can consuming probiotics improve my skin condition?
A: Several studies suggest that orally administered probiotics may help reduce symptoms of eczema and other skin conditions by restoring gut and skin microbial diversity, though more robust clinical data are still needed.
Q: What are signs of a disturbed skin or gut barrier?
A: Symptoms may include chronic dry or inflamed skin, frequent skin infections, digestive discomfort, food sensitivities, or persistent fatigue. These indicate possible barrier compromise and merit evaluation.
Q: Are there risks in using harsh soaps or overusing hand sanitizers?
A: Yes. Such products can strip both good and bad microbes from the skin, disrupting its microbiome and weakening its protective barrier.
Q: How quickly can microbiome-supporting lifestyle changes improve barrier function?
A: Some studies indicate that beneficial shifts in the gut and skin microbiomes can be observed within days to weeks after positive changes, but full restoration of barrier function may take longer.
Conclusion
Mounting evidence confirms the extraordinary and reciprocal influence of the gut and skin microbiomes in shielding the body through robust barrier functions. The emerging science of the gut-skin axis offers promising therapeutic opportunities for diverse diseases — from eczema and acne to inflammatory bowel disorders — by targeting microbiome balance. Daily choices in diet, skincare, and health practices play a profound role in protecting these microbial communities and, by extension, the body’s first and most vital lines of defense.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9654002/
- https://www.aveeno.com/journal/the-gut-skin-and-microbiome
- https://fldscc.com/how-gut-microbiome-impacts-your-skin/
- https://www.nature.com/articles/s41467-024-47072-3
- https://pubmed.ncbi.nlm.nih.gov/36361857/
- https://www.science.org/doi/10.1126/science.abo0693
Read full bio of medha deb












