Mast Cells, Histamine, and Barrier Permeability Flares: Mechanisms, Impact, and Clinical Insights
Immune mediators reshape tissue defenses, offering a blueprint for targeted therapies.
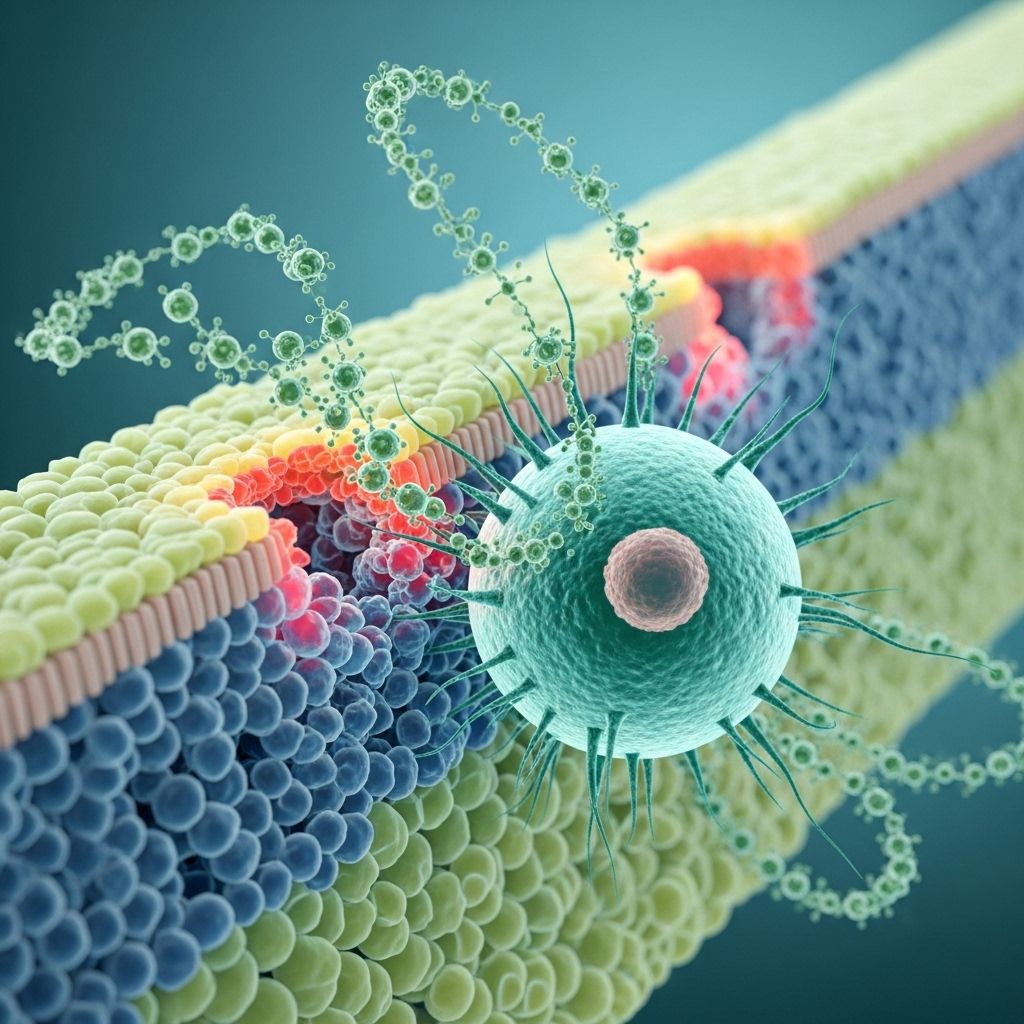
Mast cells and histamine serve as fundamental players in the body’s response to allergens, infection, and tissue injury. Their central action on barrier permeability orchestrates not only protective immune responses but, when dysregulated, underlies many pathological flares seen in allergy and inflammation. This article provides a comprehensive examination of the biology, signaling, and clinical significance of mast cell-driven barrier permeability flares, illuminating paths for therapeutic intervention.
Table of Contents
- Introduction to Mast Cells, Histamine, and Barrier Permeability
- The Biology of Mast Cells
- Histamine and Other Mast Cell Mediators
- Mechanisms of Barrier Permeability Flare
- Cellular Signaling in Histamine-Induced Permeability
- Clinical Implications: Allergy, Urticaria, and Anaphylaxis
- Therapeutic Strategies and Research Directions
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction to Mast Cells, Histamine, and Barrier Permeability
The human body relies on dynamic biological barriers—endothelial linings in blood vessels, epithelial walls in the gut, skin, and airways—to maintain homeostasis and protect against external threats. Mast cells, sentinel immune cells found throughout connective tissue and mucosae, are best known for their rapid release of histamine and other mediators upon activation. These substances transiently but powerfully increase barrier permeability, facilitating the movement of plasma proteins, leukocytes, and molecules to sites of challenge or injury. However, excessive or uncontrolled flares of barrier permeability underlie swelling, hives, systemic shock, and the pathology of many allergic and inflammatory conditions.
The Biology of Mast Cells
Mast cells are granulated immune cells derived from precursors in the bone marrow and differentiated within tissues. Found in abundance around blood vessels, nerves, and at the host-environment interface (skin, respiratory, and gastrointestinal tracts), mast cells act as rapid responders to various environmental and endogenous signals.
- Origin: Hematopoietic (bone-marrow-derived), mature in tissues.
- Main Locations: Skin, mucosa, connective tissues, perivascular spaces.
- Activation Methods: IgE-mediated (classic allergy), direct stimulation by pathogens (via Toll-like receptors), physical and chemical stimuli.
Upon activation, mast cells undergo degranulation, explosively releasing the contents of their cytoplasmic granules into the surrounding tissue.
Key Features of Mast Cell Degranulation
- Rapid exocytosis of granules after trigger recognition.
- Immediate release of pre-formed mediators (e.g., histamine, proteases, heparin).
- Subsequent synthesis and release of de novo mediators (eicosanoids, cytokines, chemokines).
These mediators coordinate acute vascular and tissue responses, fueling both defense and disease depending on context.
Histamine and Other Mast Cell Mediators
Histamine is the signature mediator released from mast cells, driving classical allergic symptoms. However, mast cell granules contain a variety of substances influencing tissue barriers and surrounding cells:
| Mediator | Main Function |
|---|---|
| Histamine | Increases vascular permeability, smooth muscle contraction, stimulation of nerve endings (itch, pain). |
| Proteases: Tryptase, Chymase, Carboxypeptidase | Degrade extracellular matrix, activate matrix metalloproteases, contribute to tissue remodeling. |
| Heparin | Anticoagulant effects, regulates protease activity. |
| Cytokines (TNF-α, IL-4, IL-5, IL-6, etc.) | Pro-inflammatory signaling, leukocyte recruitment, modulation of immune responses. |
| Lipid mediators (Prostaglandins, Leukotrienes, Platelet-Activating Factor) | Vasodilation, bronchoconstriction, increased permeability, chemotaxis. |
Among these, histamine plays the most direct role in increasing vascular and epithelial permeability, especially by acting on specific cellular receptors.
Histamine Receptors and Their Function
- H1 Receptor: Mediates vasodilation, increased vascular permeability, smooth muscle contraction. Highly expressed on endothelial cells and smooth muscle.
- H2 Receptor: Stimulates gastric acid secretion, vasodilation.
- H3, H4 Receptors: Modulate neurotransmitter release and immune cell chemotaxis, respectively.
Stimulation of H1 receptors on vascular endothelium is chiefly responsible for the classic allergic and inflammatory flare—characterized by swelling, redness, and tissue edema.
Mechanisms of Barrier Permeability Flare
Mast cell degranulation, particularly in response to antigen-IgE interactions (type I hypersensitivity), floods the local tissue with histamine and related mediators. This triggers a cascade of biochemical and biophysical changes in endothelial and epithelial cells, culminating in localized or systemic increases in permeability.
Vascular vs. Epithelial Barrier Dysfunction
- Vascular Endothelial Barrier: Maintains separation between the blood and tissue. Barrier disruption allows plasma proteins and leukocytes to migrate into tissue, causing edema and inflammation.
- Epithelial Barriers (Skin, Gut, Airways): Protect against external environment. Histamine weakens tight junctions, increasing passage of allergens or pathogens.
The immediate effects of histamine include:
- Expansion of endothelial cell gaps (paracellular leak)
- Altered cell-cell adhesion (disruption of adherens and tight junctions)
- Enhanced transcellular transport
In allergic flares, these changes manifest as urticaria (hives), angioedema, rhinorrhea, or, in severe cases, systemic shock.
Cellular Signaling in Histamine-Induced Permeability
The effects of histamine on barrier permeability are driven by complex intracellular signaling cascades. The major steps are:
- Histamine-H1 Receptor Binding: Activates G protein-coupled receptor pathways (primarily Gαq family).
- Phospholipase C (PLC) Activation: Leads to hydrolysis of PIP2 into inositol trisphosphate (IP3) and diacylglycerol (DAG).
- Calcium Mobilization: IP3 increases cytoplasmic Ca2+, activating enzymes including myosin light chain kinase (MLCK).
- RhoA/ROCK Pathway: Gαq activates the guanine nucleotide exchange factor Trio, leading to RhoA and Rho-associated kinase (ROCK) activation.
- MLC Phosphorylation: Both calcium/MLCK and RhoA/ROCK pathways ultimately phosphorylate myosin light chain (MLC), inducing actin-myosin contraction.
- Junctional Complex Remodeling: Stress fibers and contraction cause loosening of VE-cadherin-mediated adherens junctions, forming gaps between endothelial cells and increasing permeability.
Importantly, RhoA/ROCK-driven contractility is strictly required for histamine-induced barrier breakdown, even more than calcium-mediated effects alone. This insight has led to interest in ROCK inhibitors as potential therapies for pathological vascular leak syndromes.
Other Modulators of Barrier Permeability
- Nitric Oxide (NO): Induced by histamine, relaxes vascular smooth muscle and increases local blood flow, augmenting delivery of immune mediators. However, direct NO blockade does not fully prevent barrier breakdown, highlighting the dominance of cytoskeletal restructuring in permeability regulation.
- Platelet-Activating Factor (PAF): Also released from mast cells, PAF synergizes with histamine to disrupt barrier function.
- Bradykinin: Causes permeability flares independently of histamine, important in some forms of angioedema.
- Prostaglandin D2 (PGD2): Released from mast cells, may counteract permeability flares by enhancing barrier function in some contexts.
Clinical Implications: Allergy, Urticaria, and Anaphylaxis
Fluctuations in barrier permeability governed by mast cells and histamine underlie a spectrum of acute and chronic diseases:
- Urticaria (Hives): Localized mast cell activation in the skin creates transient wheals due to plasma leakage.
- Allergic Rhinitis & Asthma: Increased permeability in respiratory epithelium contributes to edema, excess mucus, and airway narrowing.
- Anaphylaxis: Systemic mast cell degranulation causes rapid vascular leakage, hypotension, and, if severe, life-threatening shock.
- Food Allergies & GI Disorders: Mast cell activity disrupts gut epithelial tight junctions, increasing vulnerability to ingested antigens.
- Chronic Inflammatory States: Dysregulated mast cell activation sustains barrier leak and tissue damage in disorders such as chronic urticaria, mastocytosis, and some autoimmune diseases.
Table: Key Clinical Manifestations of Mast Cell-Driven Permeability Flares
| Condition | Main Barrier Affected | Common Symptoms |
|---|---|---|
| Urticaria (Hives) | Skin (Endothelial) | Itchy, raised, red or pale wheals |
| Allergic Rhinitis | Nasal Epithelium | Runny nose, sneezing, congestion |
| Anaphylaxis | Systemic (Multi-organ) | Hives, swelling, hypotension, airway obstruction |
| Food Allergy | Gut Epithelium | Abdominal pain, diarrhea, anaphylaxis |
| Mastocytosis | Multiple | Flushing, abdominal symptoms, anaphylaxis |
Therapeutic Strategies and Research Directions
Management of mast cell-driven permeability flares relies on pharmacological agents targeting histamine action and mast cell function or stabilizing barrier integrity. Research continues to reveal new avenues for intervention.
- Antihistamines: H1-blockers remain first-line therapy for urticaria and allergic rhinitis.
- Corticosteroids: Suppress mast cell activation and reduce barrier inflammation in acute flares.
- Mast Cell Stabilizers (e.g., cromolyn): Inhibit degranulation, less effective for severe reactions.
- Leukotriene Receptor Antagonists: Used as adjuncts in asthma and allergic disorders.
- Anti-IgE Therapy (omalizumab): Reduces mast cell sensitivity in chronic urticaria and asthma.
- PAF and ROCK Inhibitors: Experimental; may be promising for severe vascular leak syndromes.
- Immunomodulators: Target cytokine networks sustaining chronic barrier dysfunction.
Personalized approaches based on mast cell subtype, mediator profile, and barrier-specific dysfunction offer hope for the future treatment of allergic and inflammatory disorders driven by permeability flares.
Frequently Asked Questions (FAQs)
Q: What triggers mast cell degranulation leading to barrier permeability flares?
A: The most common trigger is IgE-mediated binding to allergens (type I hypersensitivity), but mast cells can also degranulate due to physical stimuli (heat, cold), infections (bacterial, viral), neuropeptides, drugs, or even stress hormones.
Q: How does histamine increase vascular permeability?
A: Histamine binds to H1 receptors on endothelial cells, activating Gαq-protein-coupled signaling, which leads to cytoskeletal contraction and the opening of junctions between endothelial cells, thereby allowing plasma proteins and fluids to leak into tissues.
Q: Why do some people experience frequent barrier permeability flares?
A: Chronic urticaria, mast cell activation syndrome (MCAS), connective tissue disorders, or certain autoimmune diseases can all feature heightened mast cell responsiveness or abnormal mediator production, predisposing to recurrent flares.
Q: Are antihistamines always effective for controlling permeability flares?
A: While antihistamines block the effects of histamine at H1 (and sometimes H2) receptors, flares may involve additional mediators (like PAF, leukotrienes) or non-histaminergic pathways, necessitating combination therapy or alternative agents.
Q: What areas of research are advancing care of patients with permeability issues?
A: Discovery of new mast cell and endothelial signaling mechanisms (e.g., RhoA/ROCK pathway), identification of genetic risk factors, development of biologics targeting IgE or cytokines, and repurposing of drugs like ROCK inhibitors offer novel approaches to managing barrier dysfunction.
Conclusion
Mast cells and histamine are vital architects of the body’s immediate defense system, rapidly orchestrating permeability flares to help contain threats and alert the immune system. However, when these flares become exaggerated or chronic, they drive disease pathology—from annoying hives to life-threatening anaphylaxis. Continued elucidation of the precise cellular signals and mediators orchestrating barrier changes holds promise for tailored, effective therapies that restore health without compromising protection.
References
- https://www.nature.com/articles/ncomms7725
- https://www.jstage.jst.go.jp/article/trs/advpub/0/advpub_2025-010/_html/-char/en
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2015.00620/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6099187/
- https://all-imm.com/index.php/aei/article/view/1272/1936
- https://en.wikipedia.org/wiki/Mast_cell
Read full bio of Sneha Tete












