Managing Constipation Post-Bariatric Surgery: Effective Strategies for Recovery and Ongoing Health
Fluid, fiber, and light activity renew gut balance for smoother postoperative healing.
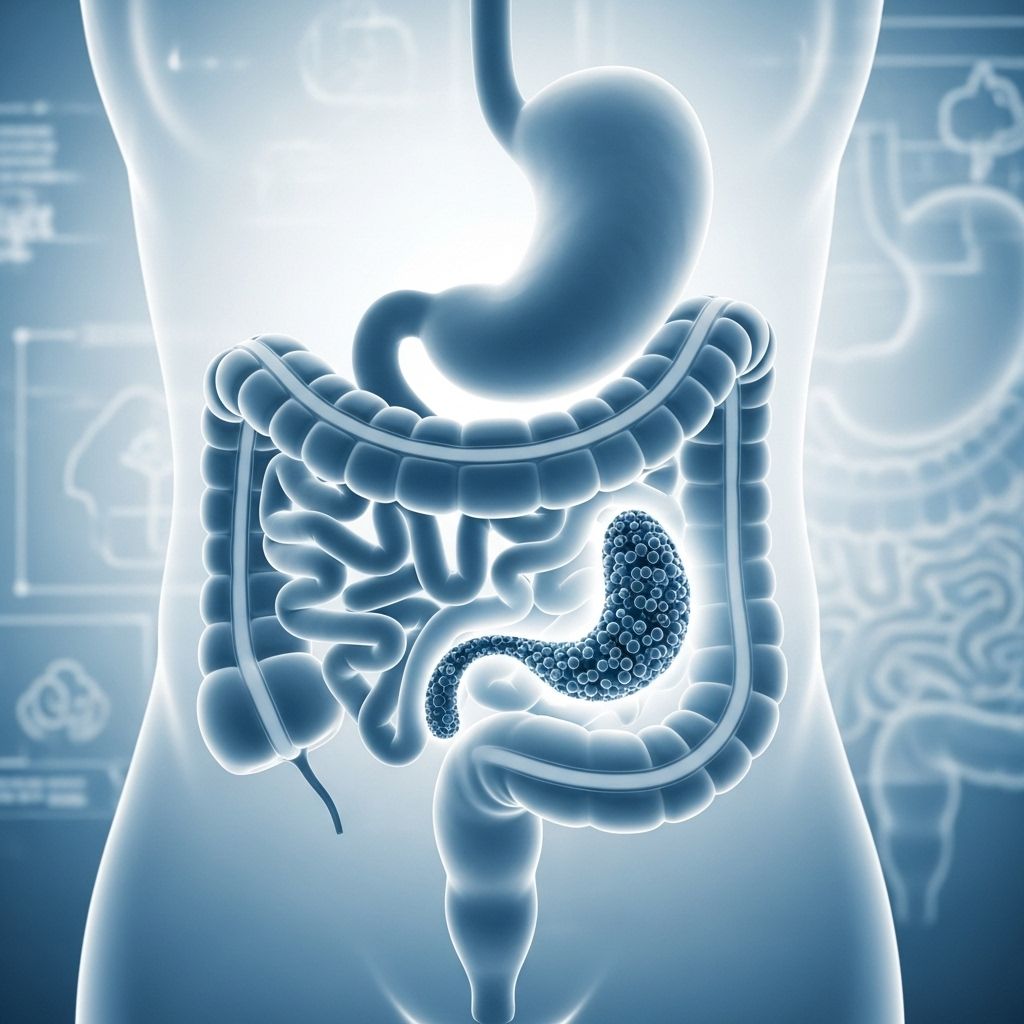
Bariatric surgery is a transformative solution for weight management and comorbidity reduction, but postoperative constipation remains a frequently reported and distressing side effect. This comprehensive guide provides practical, evidence-based advice for preventing and managing constipation after bariatric surgery, aiming for safe, comfortable recovery, and long-term digestive wellness.
Table of Contents
- Understanding Constipation after Bariatric Surgery
- Why Does Constipation Occur Post-Surgery?
- Recognizing Symptoms of Postoperative Constipation
- Preventive Strategies: Staying Ahead of Constipation
- Optimizing Hydration
- Diet and Nutrition Adjustments
- Physical Activity and Bowel Regularity
- The Role of Fiber: Tips for Gradual Introduction
- Probiotics: Supporting Gut Health after Surgery
- Medications and Supplements: Addressing Common Culprits
- Over-the-Counter Relief: Laxatives and Stool Softeners
- Practical Tips for Symptom Relief
- What to Avoid during Recovery
- When to Seek Medical Attention
- Frequently Asked Questions (FAQs)
Understanding Constipation after Bariatric Surgery
Constipation is one of the most common gastrointestinal complaints following bariatric procedures like gastric bypass, sleeve gastrectomy, and adjustable gastric banding. Factors range from surgical changes and altered physiology to changes in diet, supplementation, hydration, and research confirms that constipation typically peaks in the early weeks after surgery but can persist for months if not promptly managed.
Why Does Constipation Occur Post-Surgery?
The onset of constipation after bariatric surgery is typically multifactorial. Key causes include:
- Reduced Fluid Intake: Early post-surgery patients often struggle to drink sufficient fluids due to stomach size and discomfort.
- Lower Fiber Intake: Progression diets initially exclude high-fiber foods, limiting stool bulk.
- Decreased Physical Activity: Recovery periods may limit movement, slowing GI transit.
- Changes in Diet Composition: High protein, low residue diets favored after surgery limit stool formation.
- Medication Side Effects: Pain medications (especially opioids), iron, and calcium supplements are known to cause constipation.
Recognizing Symptoms of Postoperative Constipation
Common symptoms include:
- Fewer than three bowel movements per week
- Difficulty passing stool or requiring straining
- Dry, hard, or pellet-like stools
- Bloating, abdominal discomfort, or cramping
- A sense of incomplete evacuation
For many post-bariatric patients, it is not unusual to go up to three days without a bowel movement, but discomfort, pain, or persistent symptoms should be taken seriously.
Preventive Strategies: Staying Ahead of Constipation
Proactive bowel management helps prevent severe symptoms and complications. The following general principles are highly effective:
- Hydration: Sipping fluids frequently throughout the day
- Gradual introduction of fiber: According to post-op dietary stage
- Early gentle physical activity
- Use of probiotics where tolerated
- Monitoring medications that may worsen constipation
Optimizing Hydration
Proper hydration is the cornerstone of constipation prevention after bariatric surgery:
- Aim for 1.5–2 liters (roughly 64–80 ounces) of fluids daily.
- Sip fluids regularly rather than drinking large amounts at once.
- Prefer clear fluids: water, broth, herbal teas. Low-fat milk or soya milk can contribute to both hydration and protein intake.
- Do not drink liquids for 30 minutes before or after meals to avoid overwhelming the small stomach pouch.
- Carrying a water bottle or setting phone reminders can encourage consistent drinking.
Diet and Nutrition Adjustments
The post-surgical diet evolves in phases:
- Stage 1—Liquids: Minimal fiber, focus on hydration and protein supplements.
- Stage 2—Pureed Foods: Carefully introduce soft, low-residue foods such as pureed prunes or applesauce (from week 2 onwards).
- Stage 3—Softer Solids: Stewed fruits, Weetabix, and mashed vegetables (typically from week 3–5).
- Stage 4—Regular Solids: Gradually add in more fibrous foods like cooked vegetables, oats, and after several months, raw fruit and vegetables if tolerated.
Important: Each person’s tolerance varies and dietary advances should be individualized with the support of a registered dietitian or your surgical team.
The Role of Fiber: Tips for Gradual Introduction
Fiber adds bulk and solubility to stool while also promoting healthy gut bacteria. Strategies for safe and effective fiber intake include:
- Pureed prunes/stewed fruits (from week 2 post-op if tolerated).
- High-fiber cereals e.g., oatmeal, oat flour (from week 3–5).
- Blended or cooked vegetables (begin after week 2, but increase more after week 6).
- Gradual reintroduction of raw salads or vegetables beginning at 2–3 months post-op; many patients may require even longer before these are tolerated.
- Plant-based options: Add ground flaxseed or linseeds to yogurt, soups, or cereal (ensure extra fluid intake to avoid obstruction).
- Other fiber-rich foods (when appropriate): Chia seeds, beans, lentils, and well-soaked almonds/nuts (from third dietary period onward).
Probiotics: Supporting Gut Health after Surgery
Bariatric surgery can disrupt the gut microbiome. Introducing foods with probiotic cultures (plain yogurt) may help restore healthy intestinal flora, improve digestion, and reduce constipation.
- Choose unsweetened, plain, live-culture yogurts (Greek or regular).
- These can be incorporated once tolerating pureed or soft foods.
- Consult your provider before starting probiotic supplements.
Physical Activity and Bowel Regularity
Increased movement stimulates bowel motility and reduces the water absorbed from stool. Early and ongoing activity recommendations:
- Short walks (10–15 minutes) several times daily promote bowel function.
- Stretching and gentle yoga can activate the abdominal area.
- Always wait at least an hour after eating before exercising.
- Gradual return to aerobic and strength training, as cleared by your surgical team.
Medications and Supplements: Addressing Common Culprits
Certain medications commonly prescribed after surgery may trigger or exacerbate constipation:
- Pain medications (opioids): Limit use as soon as possible.
- Calcium and iron supplements: Both can reduce bowel motility. Take with plenty of fluids, and discuss alternative formulations with your provider.
- Other supplements: Some protein shakes or vitamins with high mineral content may slow transit; review all medications with your care team.
- Never discontinue prescribed vitamins or minerals on your own; seek professional advice for severe constipation.
Over-the-Counter Relief: Laxatives and Stool Softeners
If lifestyle measures are insufficient, certain non-prescription remedies may provide relief. Use only as directed by your healthcare provider:
- Osmotic laxatives (e.g., MiraLAX, Phillips’ Milk of Magnesia)
- Stool softeners (e.g., Colace)
- Mild stimulant laxatives (e.g., Dulcolax) for short periods only
- Fiber supplements (e.g., Benefiber or Metamucil)—ensure extra water intake
Do not rely on any laxative for longer than recommended. If there is no response within 24 hours, contact your provider.
Practical Tips for Symptom Relief
- Try a warm beverage (e.g., herbal tea) upon waking to stimulate movement.
- Adopt a “squatty potty” posture with knees elevated when sitting on the toilet to ease bowel passage.
- Establish a consistent daily routine and allow unhurried bathroom time.
- Track fluid and fiber intake in a diary to monitor patterns and challenges.
- Contact your bariatric care team if you have any questions or persistent issues.
What to Avoid during Recovery
- Raw vegetables and salads too early—these are best reintroduced after 2–3 months, and only if tolerated.
- Large, infrequent drinks; these can cause discomfort and are less effective for hydration.
- Chronic use of stimulant laxatives—may harm normal bowel function.
- Abandoning supplements without medical guidance.
When to Seek Medical Attention
Seek prompt care if you experience:
- More than 3–4 days without a bowel movement
- Severe, persistent abdominal pain or bloating
- Vomiting or inability to keep fluids down
- Blood in stool
- Unresponsive constipation despite all strategies discussed above
- Signs of bowel obstruction or complications after surgery
Timely intervention can prevent more serious complications associated with constipation, such as bowel impaction or anastomotic leaks.
Frequently Asked Questions (FAQs)
Is constipation normal after bariatric surgery?
Yes, mild to moderate constipation is one of the most common side effects post-surgery, particularly in the first 6 months due to dietary changes, reduced hydration, and physical inactivity.
How long does constipation usually last?
In most cases, constipation resolves within several weeks to a few months as fluid, fiber, and activity levels normalize. Persistent or severe constipation should be investigated further.
What should I eat to help prevent constipation?
Soft, fiber-rich foods like cooked or pureed fruits and vegetables, oatmeal, and gradually, beans and finely ground seeds, alongside adequate hydration. Follow your surgical program’s progression diet for safe advancement.
Can I take laxatives if lifestyle changes aren’t working?
Yes, short courses of gentle laxatives or stool softeners are generally considered safe after bariatric surgery—always under medical supervision and never as a long-term solution.
Why is hydration so important after surgery?
Insufficient fluids result in the colon absorbing too much water from the stool, leading to hard, difficult-to-pass motions. Consistent sipping of fluids throughout the day is crucial.
Should I stop my vitamins or iron if I experience constipation?
No, do not stop taking prescribed supplements without professional advice. Your care team may suggest changes in formulation or timing to reduce side effects.
How can I make bowel movements more comfortable?
Use a footstool to raise your knees while sitting, never rush, and try timing bowel movements after a warm beverage in the morning to encourage regularity.
Constipation after bariatric surgery is common, but with attentive self-care and guidance from your healthcare team, most cases are temporary and manageable. If you have questions, never hesitate to reach out to your providers for individual advice and support.
References
- https://www.alweightlosscenter.com/weight-loss-tips/tips-for-relieving-constipation-after-bariatric-surgery/
- https://www.somersetft.nhs.uk/bariatric-surgery/wp-content/uploads/sites/73/2021/07/Constipation-post-op-Nov-20-bg.pdf
- https://www.bariatricservices.eu/constipation-after-bariatric-surgery/
- https://www.healthline.com/health/constipation/constipation-after-gastric-sleeve
- https://memorial.health/Resources/4df26502-44f4-4ef9-8dc0-189bd36923e8/194-0309%20MWC%20Handout_Post-Op%20Bari%20Constipation_101823_web.pdf
- https://www.royalberkshire.nhs.uk/media/wabprfsy/dealing-with-constipation-after-bariatric-surgery_apr25.pdf
- https://www.medicalnewstoday.com/articles/constipation-after-gastric-sleeve
- https://asmbs.org/resources/bariatric-surgery-postoperative-concerns/
- https://towerhealth.org/sites/default/files/pdfs/2023-03/managing-constipation-after-weight-loss-surgery-english.pdf
- https://www.ucsfhealth.org/education/recovering-from-bariatric-surgery
Read full bio of Sneha Tete












