Managing Chronic Pain from Nerve Entrapment in Scar Tissue: Comprehensive Strategies and Treatments
Targeted methods dissolve fibrous adhesions to increase mobility and reduce discomfort.
Chronic pain resulting from nerve entrapment within scar tissue presents a complex therapeutic challenge that affects countless individuals following injuries or surgeries. As advances in rehabilitation, medical interventions, and pain science converge, patients have more options than ever to manage the often debilitating discomfort and functional limitations generated by this condition. This article provides a thorough, evidence-based overview of the causes, identification, and multidisciplinary management of chronic pain associated with nerve entrapment in scar tissue, empowering patients and practitioners alike to navigate the available solutions.
Table of Contents
- Understanding Nerve Entrapment in Scar Tissue
- Symptoms and Complications of Nerve Entrapment
- Diagnosis: Identifying Nerve Entrapment within Scar Tissue
- Non-Invasive and Conservative Therapies
- Minimally Invasive and Interventional Procedures
- Rehabilitation and Physical Therapy
- Lifestyle Strategies and Self-Management
- Emerging and Advanced Treatments
- Frequently Asked Questions (FAQs)
- Further Resources
Understanding Nerve Entrapment in Scar Tissue
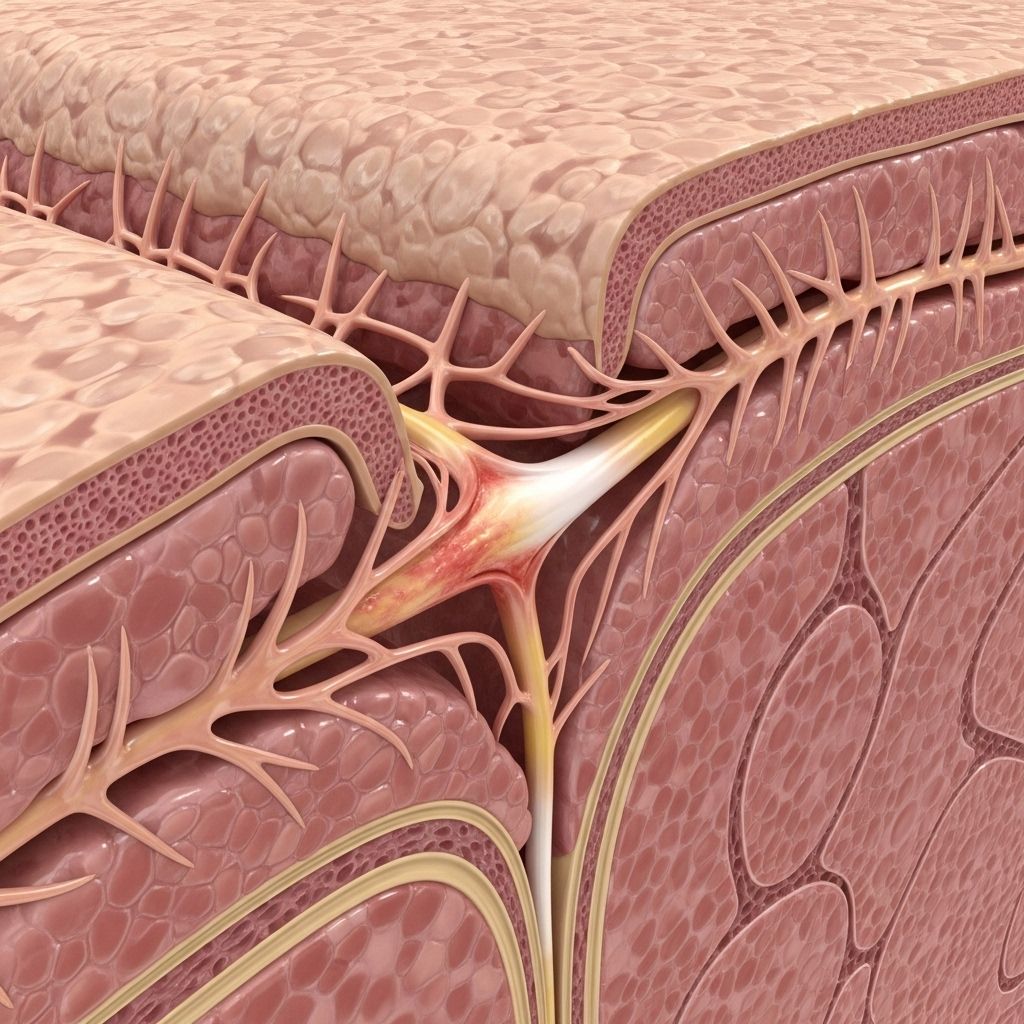
Scar tissue forms as a natural response to skin injury, surgery, or trauma, functioning as the body’s rapid repair mechanism. While scars are a sign of healing, they sometimes develop with characteristics that compromise nerve function. In some cases, nerve fibers become trapped or compressed within the fibrous matrix of scar tissue. This entrapment can instigate persistent pain, abnormal sensations, and movement restrictions.
How Scar Tissue Entraps Nerves
- Abnormal collagen formation: After injury, the body produces collagen fibers that can create dense, disorganized plaques—sometimes enveloping or compressing peripheral nerves.
- Adhesions: These fibrous connections can tether nerves to surrounding tissues, limiting their normal movement during body motion and leading to irritation.
- Inflammatory responses: Chronic inflammation in or around a scar can sensitise nerve fibers, amplifying pain signals or causing new nerve branches to form aberrantly through the scar itself.
Symptoms and Complications of Nerve Entrapment
The symptoms of nerve entrapment in scar tissue can be persistent and severe, often affecting quality of life and functional capacity. Common clinical features include:
- Localized or radiating pain: Stabbing, burning, or tingling sensations at or near the scar site.
- Hypersensitivity: Heightened sensitivity to touch (allodynia or hyperalgesia).
- Numbness or altered sensation: Areas with partial loss of feeling adjacent to the scar.
- Reduced range of motion: Due to pain or tissue tightness, affecting daily activities.
- Muscle weakness: If nerve conduction is significantly impaired.
- Functional limitations: Difficulty with walking, gripping, or other movements depending on location.
Chronic pain from nerve entrapment may develop soon after injury or surgery, but it can also emerge months or years later as scar tissue matures and changes in structure.
Diagnosis: Identifying Nerve Entrapment within Scar Tissue
Accurate diagnosis forms the cornerstone of effective management. A multidisciplinary approach is often used, combining:
- Detailed history and examination: Eliciting the pain’s onset, nature, aggravating factors, and impact on function.
- Physical inspection: Palpation of scar tissue for tenderness, thickening, or areas suggestive of nerve involvement.
- Sensory mapping: Identifying patterns of numbness, hypersensitivity, or referred pain.
- Electrodiagnostic testing: Studies such as nerve conduction velocity (NCV) and electromyography (EMG) can localize nerve dysfunction.
- Imaging: High-resolution ultrasound or MRI may visualize nerve entrapment, scar thickness, or soft-tissue changes obstructing nerve pathways.
Non-Invasive and Conservative Therapies
First-line management strategies target symptom relief, restoration of mobility, and prevention of further impairment. Conservative methods may be effective, especially for mild to moderate cases or as part of a combination approach.
Manual Therapies
- Massage and Myofascial Release: Gentle to firm tissue mobilization, often following the scar’s direction, to desensitize nerves, reduce pain, and soften scar tissue.
- Graston Technique: Special metal instruments gently break down fibrous adhesions and promote tissue remodeling. Effective for improving range of motion and reducing pain in affected joints.
- Cupping and Soft Tissue Mobilization: Techniques that lift and mobilize the skin and underlying tissues may further enhance flexibility and blood flow.
- Nerve Gliding Manual Therapy: Specialized techniques to mobilize entrapped nerves, improving their movement and reducing discomfort.
Physical Modalities
- Compression Therapy: Elastic wraps or compression garments can decrease inflammation and discomfort while flattening scar tissue.
- Electrical Stimulation (TENS): Safe, non-invasive electrical currents may help modulate pain perception and improve local circulation.
- Vibration Therapy: Handheld massagers or vibration devices desensitize nerves when used regularly.
- Moisturizers and Silicone Gel: Hydrating creams and silicone sheets or gels reduce sensitivity and encourage softening of new or mature scars.
Exercise and Movement
- Controlled Exercise Programs: Guided stretching and movement routines, tailored by a physical therapist, prevent joint stiffness and improve functionality.
Summary Table: Core Non-Invasive Scar Pain Therapies
| Therapy | Mechanism | Benefits |
|---|---|---|
| Massage/Myofascial Release | Mobilizes scar Tissue desensitization | Reduces pain Improves movement |
| Compression | Reduces swelling Flattens tissue | Decreases pain Scar minimization |
| Electrical Stimulation | Modifies nerve signaling | Lessens chronic pain |
| Vibration | Desensitizes nerves | Reduces sensitivity over time |
| Exercise/Stretching | Improves flexibility | Prevents joint contracture |
| Silicone Gel/Sheets | Promotes hydration Encourages remodeling | Lessens tightness Enhances tissue health |
Minimally Invasive and Interventional Procedures
For persistent cases where conservative therapies provide inadequate relief, several minimally invasive interventions may be appropriate. Selection should be individualized based on scar characteristics, pain patterns, and overall medical status.
- Dry Needling: Involves insertion of fine, sterile needles directly into tissues near painful scars, fascia, or adjacent muscles to disrupt painful adhesions, stimulate blood flow, and decrease nerve excitability. Can be combined with other modalities for enhanced relief.
- Trigger Point Injections: Utilizing local anesthetics (like lidocaine) or agents such as clonidine, these injections target focal areas of irritability to block abnormal pain signals and diminish hypersensitivity for extended periods.
- Corticosteroid Injections: Injected into or adjacent to the scar, corticosteroids reduce inflammation and disrupt overactive collagen production. Particularly helpful for scars associated with swelling, itching, or hypertrophy, though side effects (skin thinning, depigmentation) must be considered.
- Astym® Therapy: Instrument-assisted soft tissue treatment designed to break down scar tissue, address soft tissue dysfunction, and promote normal healing. Usually paired with a stretching protocol.
- Fat Grafting: Surgical transplantation of fat cells and associated stem cells beneath a restrictive scar may encourage fresh, healthy tissue growth, reduce tightness, and enhance nerve mobility.
- Laser Therapy: Non-ablative lasers stimulate collagen remodeling, soften scar tissue, and reduce associated pain and itching. Particularly effective for mature or thick scars.
- Scar Revision Surgery: Reserved for intractable pain or functional loss, this surgical procedure removes problematic scar tissue and reconstructs the area, sometimes utilizing skin grafts for optimal results. Risks and recovery time are weighed against potential benefits.
Rehabilitation and Physical Therapy
A multidisciplinary rehabilitation program plays a pivotal role for individuals with chronic pain due to nerve entrapment in scar tissue. Core goals of therapy include pain relief, restoration of functional mobility, and prevention of secondary complications such as muscle weakness or joint contracture.
- Personalized Exercise Regimens: Including stretching, strengthening, and graded activity tailored to the affected region.
- Manual Scar Manipulation: Consistent, evidence-based scar massage under professional supervision to reduce tension and increase pliability.
- Therapeutic Modalities: Hot/cold therapy, ultrasound, and kinesiotaping may all facilitate tissue healing and pain reduction.
- Education and Self-Management: Patients are trained in home techniques for ongoing scar care, pain tracking, and functional adaptation.
Lifestyle Strategies and Self-Management
Empowering patients to actively participate in their pain management yields the best long-term results. The following lifestyle interventions have shown value:
- Daily Gentle Movement: Incorporate low-impact activities (walking, swimming, gentle yoga) to enhance circulation and prevent deconditioning.
- Skin and Scar Care: Use unscented moisturizers to keep skin supple; avoid harsh chemicals that may irritate scars.
- Activity Modification: Adapt daily tasks to avoid repeated stress or impact to the affected area.
- Stress Management Techniques: Chronic pain may lead to psychological impacts; mindfulness, guided relaxation, or cognitive behavioral therapy can help mitigate the emotional burden.
- Nutrition: A balanced diet rich in antioxidants and omega-3 fatty acids may modulate inflammation and support tissue healing.
Emerging and Advanced Treatments
Research continues to identify novel approaches for stubborn or complex cases:
- Regenerative Medicine: Growing interest exists in platelet-rich plasma (PRP) and stem cell therapies, which may expedite optimal tissue remodeling, though robust clinical data are still forthcoming.
- Neurostimulation Devices: For select patients, implantable or external devices that deliver targeted electrical pulses to block pain transmission offer a promising solution.
Frequently Asked Questions (FAQs)
Q: How long after surgery or injury can scar tissue start causing nerve pain?
A: Nerve pain from scar tissue may start within weeks of recovery or emerge months to years later as scar tissue matures and changes.
Q: Can scar tissue pain go away on its own?
A: Mild cases may spontaneously improve as nerve irritation settles, but chronic pain often requires active interventions.
Q: Are there risks to manual therapy or massage over scar tissue?
A: While generally safe, improper pressure or aggressive manipulation can exacerbate pain or damage delicate tissues. Always consult a licensed provider for techniques appropriate to your scar.
Q: What are signs that I should seek medical intervention for scar-related pain?
A: Persistent, worsening, or disabling pain; progression of numbness or weakness; or new functional impairment all warrant specialist evaluation.
Q: Are surgical options always successful for chronic nerve pain in scar tissue?
A: Surgery can be highly effective, especially when targeted, but carries risks like infection, recurrence, or further scarring. It is usually considered after less invasive methods have failed.
Further Resources
- Consult board-certified physiatrists, pain specialists, and plastic surgeons for multidisciplinary care.
- National pain foundations and patient advocacy groups offer educational materials and support networks.
Disclaimer: This article is intended for information only. For persistent or severe symptoms, consult with your healthcare provider for an individualized plan.
References
- https://www.healthline.com/health/scar-tissue-pain
- https://excelsportspt.com/7-ways-to-relieve-chronic-scar-tissue-pain/
- https://www.medicalnewstoday.com/articles/scar-tissue-pain
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8994628/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10155853/
- https://www.youtube.com/watch?v=B_kArnWVEK4
- https://protailored.com/scar-management/
- https://www.houstonmethodist.org/blog/articles/2024/jan/what-to-do-when-post-surgical-scar-tissue-is-affecting-you/
- https://www.bcm.edu/healthcare/specialties/orthopedics-and-sports-medicine/orthopedic-and-sports-physical-therapy/scar-tissue-treatment
- https://www.robsatriano.com/scar-tissue-treatment
Read full bio of Sneha Tete












