Low Stomach Acid & Nutrient Deficiencies: B12 and Iron Absorption Explained
Balancing digestive enzymes supports nutrient uptake and eases ongoing gut discomfort.
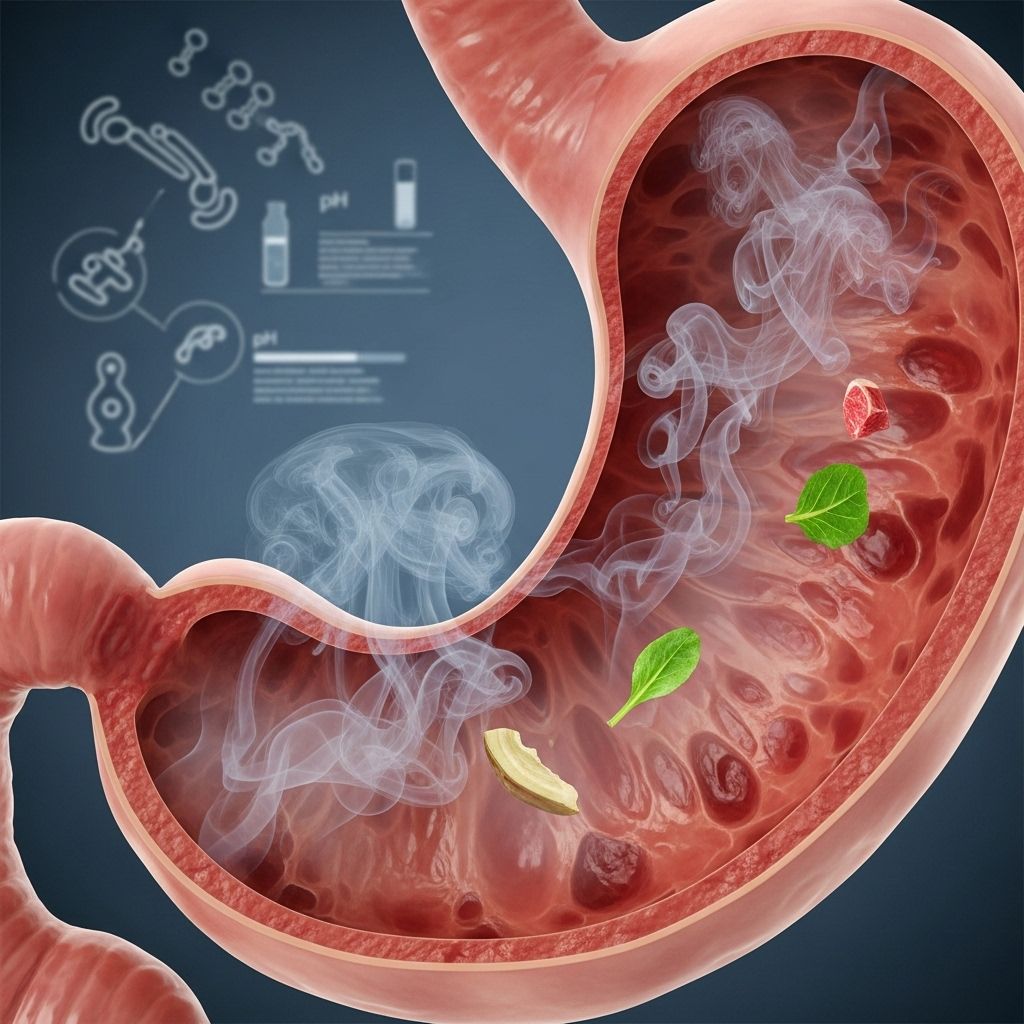
Table of Contents
- Introduction
- The Crucial Role of Stomach Acid in Digestion
- What is Hypochlorhydria (Low Stomach Acid)?
- Common Causes of Low Stomach Acid
- Recognizing Symptoms and Signs
- Impact on Nutrient Absorption
- Vitamin B12 Deficiency
- Iron Deficiency
- Testing and Diagnosis
- At-Risk Populations
- Long-Term Complications
- Holistic and Medical Treatment Strategies
- Frequently Asked Questions
- Conclusion
Introduction
Stomach acid, scientifically known as hydrochloric acid (HCl), performs essential functions in digestion, nutrient absorption, and defense against pathogens. When levels drop below normal, a condition called hypochlorhydria arises. This can quietly disrupt your health, often resulting in inadequate absorption of critical nutrients such as Vitamin B12 and iron, both vital for energy production, neurological function, and immune support. This article explores the causes, symptoms, and solutions for low stomach acid and its relationship with nutrient deficiencies.
The Crucial Role of Stomach Acid in Digestion
Hydrochloric acid in the stomach serves as a foundation for proper digestion. It triggers the breakdown of proteins, activates digestive enzymes, and creates an acidic environment necessary for absorbing nutrients. Stomach acid also acts as a natural barrier to infections by neutralizing harmful microorganisms that enter via food.
Key digestive roles include:
- Initiating protein digestion by activating pepsin.
- Facilitating mineral (iron, calcium, magnesium) and vitamin (B12, folate) absorption.
- Preventing bacterial overgrowth by creating an inhospitable environment for pathogens.
- Triggering the release of hormones that guide further digestive steps downstream.
What is Hypochlorhydria (Low Stomach Acid)?
Hypochlorhydria refers to a reduced concentration or production of hydrochloric acid by the stomach lining. It is distinct from achlorhydria (no acid production) and hyperchlorhydria (excess acid production). Insufficient acid impairs the stomach’s ability to digest food efficiently and absorb nutrients, often leading to silent or subtle symptoms.
Some critical aspects to understand:
- Hypochlorhydria can affect people of any age but becomes more common with advancing age.
- Chronic cases frequently go undiagnosed until related health issues emerge.
- Standard treatments for acid reflux, such as antacids and proton pump inhibitors, sometimes aggravate or cause low acid states.
Common Causes of Low Stomach Acid
Multiple factors can contribute to low stomach acid production. Main triggers include:
- Age: Acidity naturally diminishes as people get older, especially beyond age 65.
- Stress: Chronic stress downregulates the nervous system’s focus on digestion, reducing acid secretion.
- Medications: Long-term use of antacids (like PPIs) targeting ulcers or reflux often suppress stomach acid.
- Helicobacter pylori infection: This common bacterium causes ulcers and can impair acid secretion over time.
- Stomach surgery: Gastric bypass or other surgeries affecting the stomach’s capacity often reduce acid output.
- Autoimmune disorders: Conditions such as atrophic gastritis or lupus may damage the stomach lining.
Other contributing conditions include:
- Thyroid problems
- Chronic inflammatory illnesses (psoriasis, eczema, arthritis)
- Dietary deficiencies and poor nutrition
Recognizing Symptoms and Signs
Many symptoms of hypochlorhydria arise due to poor digestion and absorption. Some signs may seem unrelated to the gut, making diagnosis challenging.
Common symptoms include:
- Bloating after meals
- Frequent burping or gas
- Heartburn or acid reflux
- Early satiety (feeling full quickly)
- Nausea, especially when taking supplements
- Abdominal pain or discomfort
- Diarrhea and/or constipation
- Undigested food in stool
- Hair loss or brittle nails
- Fatigue and weakness
- Weight loss (in unexplained or chronic cases)
Possible additional symptoms due to nutrient deficiencies:
Table: Symptom Comparison
| Symptom | Low Stomach Acid (Hypochlorhydria) | Excess Stomach Acid (Hyperchlorhydria) |
|---|---|---|
| Bloating | Common | Less common |
| Burping/Gas | Frequent | Occasional |
| Reflux/Heartburn | Yes | Yes |
| Indigestion | Common | Common |
| Nutrient Deficiencies | Frequent | Rare |
Impact on Nutrient Absorption
Low stomach acid directly impairs the absorption of several critical nutrients:
- Vitamin B12: Requires stomach acid to detach from protein in food and bind to intrinsic factor for absorption.
- Iron: Acidic conditions convert iron from food (ferric form) into the absorbable ferrous form.
- Calcium and magnesium: Need acid for optimal absorption and function.
- Protein: Without acid, pepsin enzyme cannot activate to break down dietary protein.
Decreased acid also raises infection risk and gut barrier problems (“leaky gut”), further exacerbating difficulties in absorbing and retaining nutrients.
Vitamin B12 Deficiency
Vitamin B12 is vital for red blood cell formation, DNA synthesis, and nerve function. Its absorption is complex, requiring adequate stomach acid:
- B12 in food binds to protein.
- Hydrochloric acid and pepsin in the stomach break this bond.
- Free B12 links to intrinsic factor for safe passage and absorption in the small intestine.
When stomach acid is low:
- B12 remains bound, leading to malabsorption.
- Deficiency symptoms surface gradually: tiredness, pale skin, neurological changes (numbness, tingling, memory loss), and anemia.
- Pernicious anemia can result if both B12 and intrinsic factor are lacking.
Those with long-term low stomach acid, older adults, vegetarians/vegans, and people on PPIs are at increased risk.
Iron Deficiency
Iron is essential for oxygen transport and cellular metabolism. Dietary iron comes in two forms: heme (from animal sources) and non-heme (from plants). Stomach acid facilitates the conversion of non-heme iron to the more absorbable ferrous form.
- Without adequate acid, absorption decreases—especially for plant-sourced iron.
- Iron deficiency anemia may develop, with symptoms like fatigue, pale skin, shortness of breath, and poor concentration.
Iron deficiency often co-exists with B12 deficiency in hypochlorhydria because both depend on acidic digestion for absorption.
Testing and Diagnosis
Diagnosing hypochlorhydria and related deficiencies involves:
- Blood tests for markers of anemia, B12, iron, and intrinsic factor.
- Gastrointestinal evaluation: assessing signs of indigestion, stool analysis for undigested food.
- Specific gastric testing: measuring stomach acidity via Heidelberg or similar pH capsule.
Physicians may also check for underlying conditions such as autoimmune disorders, Helicobacter pylori infection, or thyroid issues.
At-Risk Populations
- Older adults: Acid production naturally declines with age.
- Chronic users of acid-lowering drugs: Those on long-term PPIs or antacids.
- Individuals with chronic stress: Prolonged stress suppresses digestive activity.
- Previous stomach surgery patients
- People with autoimmune conditions
Long-Term Complications
If low stomach acid is not addressed, complications may arise:
- Anemia: Due to insufficient B12 or iron.
- Bacterial overgrowth: Less acid creates an environment where bacteria flourish, risking infections and “leaky gut”.
- Osteoporosis and bone fractures: Linked to calcium and vitamin D malabsorption.
- Neurological issues: Nerve damage from prolonged B12 deficiency.
- Autoimmune disorders: Risk increases as gut barrier integrity weakens.
Holistic and Medical Treatment Strategies
Restoring stomach acid and addressing nutrient deficiencies involve several approaches:
- Manage underlying causes: Treat Helicobacter pylori, reduce stress, address autoimmune factors.
- Review medication use: Only use acid-lowering drugs as genuinely needed, under medical supervision
- Dietary changes:
- Eat whole foods, especially nutrients easily absorbed with acid (lean meats, eggs).
- Chew food thoroughly to aid digestion.
- Limit processed foods and excess sugar, which may impair gut function.
- Add small amounts of apple cider vinegar or bitters before meals (if tolerated) to stimulate acid.
- Nutrient supplementation:
- Vitamin B12 (oral or injections; sublingual forms may bypass absorption issues).
- Iron supplements (rust-colored ferrous sulfate may be preferred).
- Magnesium, calcium, and other minerals.
- Specific therapies:
- In severe cases, supervised betaine HCl supplementation to increase stomach acidity.
- Monitor progress: Repeat bloodwork and symptom review. Watch for improvement in fatigue, skin, and digestive symptoms.
Preventive Measures
- Avoid unnecessary use of acid-suppressing medications.
- Support digestion with regular mealtimes, stress reduction, and adequate hydration.
- Consider probiotics for gut health (after discussion with a healthcare provider).
Frequently Asked Questions
Q: Is heartburn always due to excess acid?
No. Heartburn can result from both excess and low stomach acid. Often, hypochlorhydria is mistaken for excessive acidity, yet the symptoms may be driven by poor digestion and bacterial imbalance rather than acid overflow.
Q: Who should be tested for low stomach acid?
Testing is advisable if you have persistent indigestion, unexplained anemia, or symptoms of nutrient deficiency and have risk factors such as older age, chronic medication usage, or autoimmune conditions.
Q: Can low stomach acid be cured permanently?
The outcome depends on the cause. Some cases respond well to treatment if caused by manageable factors like diet or medications. Others, such as age-related decline, may require ongoing management and supplementation.
Q: Is supplementing with enzymes or HCl safe?
Usually safe under guidance, especially when done with medical supervision and gradual introduction; not recommended for those with active ulcers or certain medical conditions.
Q: Are vegetarians more susceptible to B12 deficiency?
Yes. Vitamin B12 is found mainly in animal products and requires acid for absorption; low acid compounds the risk for vegetarians and vegans, making supplementation and regular monitoring important.
Conclusion
Low stomach acid, or hypochlorhydria, is a frequently overlooked cause of digestive problems and nutrient deficiencies. Its impact on absorption of vitamin B12 and iron can lead to anemia, fatigue, neurological symptoms, and long-term health complications. Awareness, accurate diagnosis, and targeted treatment—spanning dietary modifications, stress management, and supplementation—are essential for restoring digestive health and preventing chronic illness.
References
- https://www.healthline.com/health/hypochlorhydria
- https://www.parsleyhealth.com/blog/low-stomach-acid-symptoms-treatment
- https://www.buzzrx.com/blog/low-stomach-acid-symptoms
- https://zoe.com/learn/low-stomach-acid-symptoms
- https://www.webmd.com/digestive-disorders/what-is-hypochlorhydria
- https://thefunctionalgutclinic.com/post/low-stomach-acid-everything-you-need-to-know
- https://www.culturalhealthsolutions.com/the-link-between-stomach-acid-and-optimal-health/
- https://www.medicalnewstoday.com/articles/322491
- https://en.wikipedia.org/wiki/Achlorhydria
Read full bio of Sneha Tete












