Slowly Starving: Lisa Brown’s Battle with Gastroparesis and SMAS
A hidden digestive compression can cause life-threatening malnutrition and unfair judgment.
“I’m Slowly Starving to Death—And I Can’t Stop It”
Lisa Brown’s life changed dramatically when her body began to turn against her. Despite a former career as a model and a sociable, energetic lifestyle, the Wisconsin resident found herself facing a rare and debilitating gastrointestinal disorder. Lisa’s journey is one of profound struggle, repeated medical setbacks, and a daily fight—not just for survival, but for understanding.
A Misunderstood Illness: Beyond the Surface
Standing 5’10”, Lisa had always been lean but healthy. Her drastic weight loss—plummeting from 140 to under 90 lbs—caused strangers to make hurtful assumptions about eating disorders. “People come up and give me advice, or say things like ‘skinny bitch’, thinking it’s anorexia,” Lisa recalls. But her condition is rooted not in choice, but in a pair of rare, life-threatening gastrointestinal diseases.
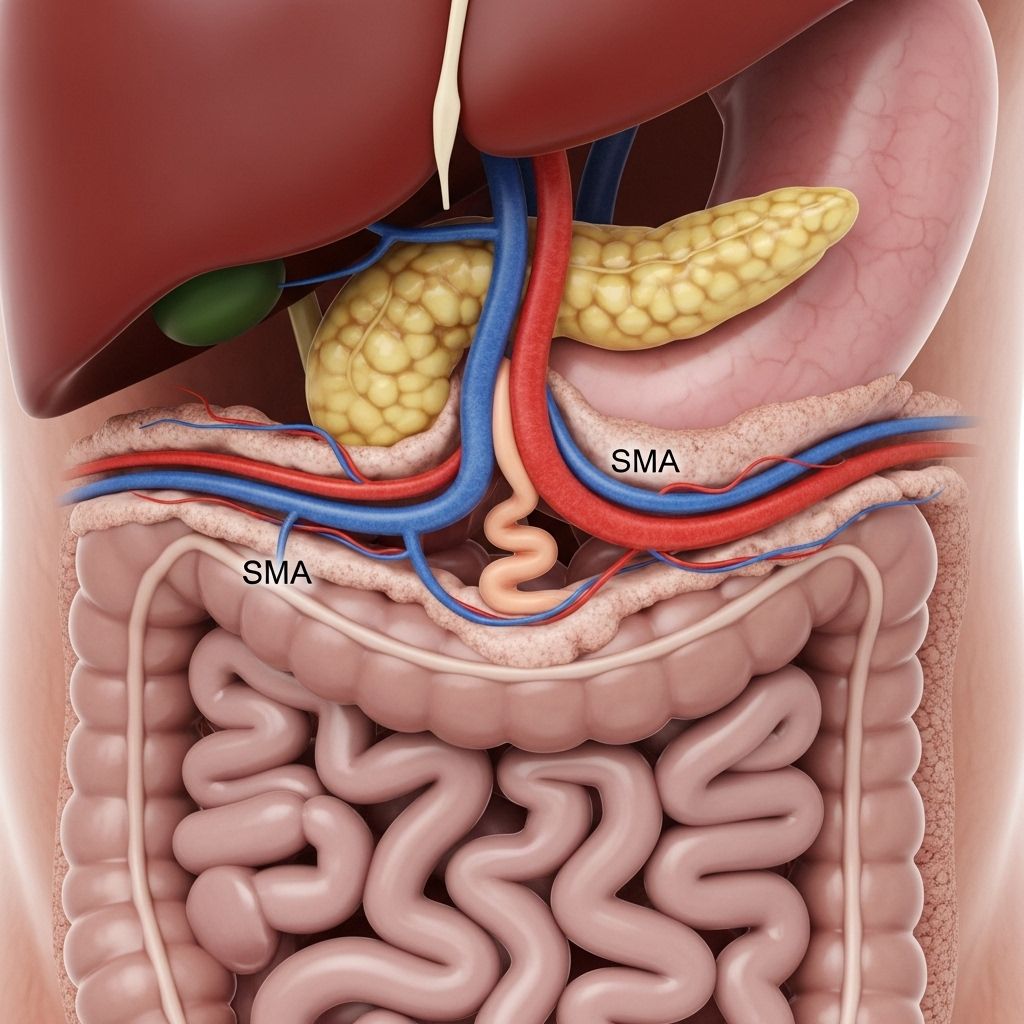
- Superior Mesenteric Artery Syndrome (SMAS): A disorder where the small intestine is compressed between arteries, causing a near-total blockage of digestion.
- Gastroparesis: A form of stomach paralysis that prevents proper emptying and absorption of food, resulting in malnutrition.
A Healthy, Happy Life, Interrupted
Back in 2012, Lisa’s life was filled with joy—her marriage, her travels, and active social life. That year, subtle but ominous changes began:
- Early satiety—feeling full after just a few bites
- Pants and her pink sapphire wedding ring started slipping off
- Unexplained nausea and abdominal pain
- Inability to keep food down, frequent vomiting after meals
The symptoms intensified quickly. “My ability to eat quantities kept shrinking, until I couldn’t eat anything,” Lisa remembers. The pain often left her curled up on the floor, in tears. Yet, initial tests—ranging from thyroid panels to food intolerance checks—provided no explanations. The months dragged on without answers.
Diagnostic Challenges and Medical Frustrations
Lisa’s struggle underscores the difficulties of diagnosing gastrointestinal disorders:
- Similar Symptoms: Many GI diseases share overlapping symptoms—nausea, weight loss, pain—making diagnosis complex.
- Exhaustive Testing: Lisa underwent imaging, endoscopies, colonoscopies, and restrictive diets—all yielding no relief.
- Time Wasted: “I was just being shuffled between doctors while my health kept declining,” Lisa notes.
An Elusive Diagnosis: SMAS and Its Impact
In 2013, after consultations at three hospitals and numerous CT scans, Lisa was finally diagnosed with Superior Mesenteric Artery Syndrome (SMAS). This rare condition occurs when the duodenum is compressed by a critical artery, halting digestion and preventing food from passing through the small intestine. Only 0.1% or fewer people develop SMAS, and delayed diagnosis is common due to lack of awareness among physicians.
SMAS Fast Facts
| Aspect | Details |
|---|---|
| Prevalence | ~0.1% of the population |
| Mortality | About 30% chance of death if untreated |
| Symptoms | Severe weight loss, vomiting, pain, malnutrition |
| Treatments | Feeding tubes, surgery, nutritional support |
Despite multiple surgeries and interventions—including nasogastric feeding tubes, stomach tubes, and vascular feeding systems—Lisa’s condition continued to worsen.
Brief Respite: Hope, Then Relapse
For a few brief months, Lisa experienced what she calls a “honeymoon period.” She could keep some food down, travel with her husband, and almost imagine a return to normalcy. But in May, her vomiting and pain returned relentlessly. “I’d thought it was a total fix,” she says, “but everything just got worse again.” Ongoing nutritional interventions could not halt the inexorable decline.
The New Normal: Life on a Feeding Tube
When Lisa arrived at Cleveland Clinic, her health was so dire it took two and a half weeks of stabilization before doctors even dared perform further tests. Dr. Matthew Kroh and his team focused on counteracting her severe malnutrition and searching for additional answers.
- SmartPill Test: A high-tech capsule sent through her intestines tracked hormone, pH, and transit data—ultimately pointing to a second diagnosis.
- Second Diagnosis: Gastroparesis, likely caused by nerve damage after abdominal surgery for SMAS, further paralyzed her stomach.
Lisa’s current daily routine revolves around a feeding pump. For 16 hours each day, she remains tethered to a tube just to receive essential calories and nutrients. Even so, “I still feel like two metal fists are twisting my insides,” she explains. Mornings, when pain is the least, are the most bearable part of her day. Most days, Lisa rarely leaves her home, confined by fatigue and pain.
Medical Realities: Why Gastroparesis Develops
Gastroparesis is a little-known and poorly understood condition in which nerve damage prevents the stomach from pushing food into the intestines. Food lingers in the stomach—leading to nausea, bloating, vomiting, and malnutrition. It often follows abdominal surgery, especially when coupled with pre-existing vascular conditions like SMAS.
- Symptoms: Constant nausea, severe abdominal pain, vomiting, chronic malnutrition
- Risk Factors: Abdominal surgery, diabetes, viral infections
- Treatments: Diet modifications, prokinetic medications, surgical implants, and long-term tube feeding
Social Isolation and Emotional Pain
Beyond physical agony, Lisa’s condition brings profound emotional consequences. She is frequently the target of public shaming by those who mistake her skeletal appearance for an eating disorder. “High school students yell at me to eat a cheeseburger,” she says. Even medical professionals, she notes, often lack awareness of SMAS and gastroparesis—leading to misdiagnosis and delayed care.
Support from her husband, Patrick Brown, and close family has been crucial. “The disease changed everything,” Patrick admits. “I fix things for a living, but I can’t fix this. All I can do is be her rock.” Their relationship has become a partnership in endurance and resilience, confronting challenges at every level—physical, emotional, and practical.
Building Awareness: Advocacy for Rare Digestive Diseases
Lisa is one of only about 400 documented cases of SMAS worldwide. She now channels her remaining energy into educating both the public and the medical community:
- Advocating that rare digestive illnesses are often invisible, easily misunderstood, and mistaken for behavioral disorders
- Emphasizing the importance of prompt recognition and intervention to prevent life-threatening malnutrition
- Encouraging compassion, not judgment, from those witnessing drastic weight loss or unusual eating patterns
“One out of three people with SMAS die,” Lisa warns, urging practitioners and laypeople alike to take such conditions seriously and to consider rare disorders when standard diagnoses fall short.
Daily Realities and Coping Mechanisms
The logistics of Lisa’s life are dictated by her feeding regimen. Every day at around 2 p.m., she connects to her feeding pump—often for 16 hours or more. She plans her days around moments when pain is tolerable, using mornings to attempt brief outings or social interaction. Even basic tasks can be overwhelming.
Frequently Asked Questions (FAQs)
What is Superior Mesenteric Artery Syndrome (SMAS)?
SMAS is a rare gastrointestinal disorder in which the duodenum (part of the small intestine) is compressed between two major arteries, obstructing the passage of food and leading to severe malnutrition.
How is gastroparesis different from SMAS?
Gastroparesis involves paralysis of the stomach muscles, preventing food from passing normally into the intestines. While SMAS is a physical blockage due to vascular compression, gastroparesis is a nerve dysfunction that impairs motility.
What are the main signs of gastroparesis?
Persistent nausea, vomiting, feeling full after small meals, unexplained weight loss, and severe abdominal pain are the primary symptoms. It can sometimes be mistaken for more common digestive issues or even eating disorders.
Why are these conditions so hard to diagnose?
Both SMAS and gastroparesis are extremely rare and share symptoms with many more common illnesses. Many healthcare providers may not consider them initially, leading to delayed or missed diagnoses.
How can the public help individuals battling these diseases?
Approach with empathy, avoid assumptions about eating behavior, listen, and help spread awareness. Chronic conditions like Lisa’s are not choices—they are complex medical realities that deserve understanding, not judgment.
Towards Hope: Treatment, Research, and Compassion
Though Lisa’s journey has been marked by pain and isolation, it is also defined by resilience and advocacy. Her story highlights the need for:
- Earlier and more accurate diagnosis of rare digestive disorders
- Better support systems for patients and families
- Continued research into the causes and treatments for gastroparesis and SMAS
- Reduction of stigma for those whose symptoms are easily misread
Lisa’s simple wish is to regain enough health to enjoy basic pleasures—like a meal without pain, or a walk in the sunshine with her husband. Until then, she remains a tireless advocate, ensuring that the world understands what it really means to be “starving to death”—not by choice, but by cruel biological fate.
References
- https://www.goodhousekeeping.com/health/a33459/lisa-brown-starving-to-death-gastroparesis/
- https://www.medicaldaily.com/pulse/digestive-health-ex-model-chronic-stomach-pain-slowly-starving-death-rare-disease-350072
- https://www.youtube.com/watch?v=lAC5TtEdyKc
- https://www.desmoinesregister.com/story/news/local/daniel-finney/2015/08/16/starvation-disease-living-nightmare-woman/31746463/
Read full bio of Sneha Tete












