Ischemia-Reperfusion Skincare: Revolutionary Principles for Skin Healing
Managing blood flow properly can lessen skin damage and boost healing after fillers.
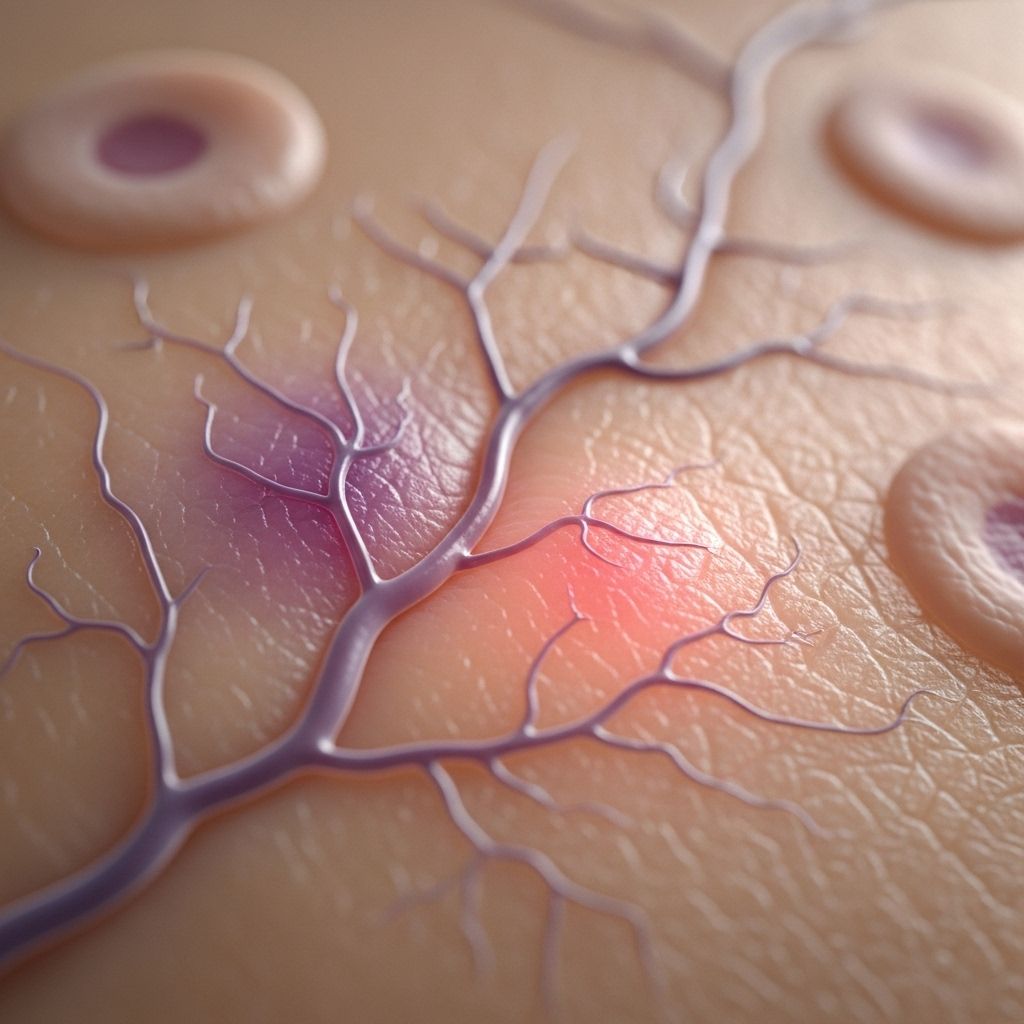
Table of Contents
- Understanding Ischemia-Reperfusion in Skincare
- The Science Behind Ischemia-Reperfusion Injury
- Clinical Applications in Skincare
- Treatment Protocols and Management
- Wound Healing and Recovery
- Prevention Strategies
- Future Directions
- Frequently Asked Questions
Understanding Ischemia-Reperfusion in Skincare
Ischemia-reperfusion injury (IRI) represents a complex biological phenomenon that has profound implications for modern skincare and aesthetic medicine. This condition occurs when blood supply returns to tissue after a period of oxygen deprivation, paradoxically causing additional tissue damage beyond the initial ischemic insult. In the context of skincare, understanding these principles has become crucial for practitioners working with dermal fillers, wound healing treatments, and various aesthetic procedures.
The concept of ischemia-reperfusion in skincare emerged from observations in cardiovascular and organ transplant medicine, where researchers discovered that restoring blood flow to oxygen-starved tissues could cause more damage than the initial lack of oxygen itself. This counterintuitive finding has revolutionized how we approach skin treatments, particularly in managing complications from cosmetic procedures and optimizing wound healing protocols.
Modern skincare applications of ischemia-reperfusion principles focus primarily on three key areas: managing vascular complications from dermal filler injections, optimizing wound healing processes, and developing preventive strategies for tissue damage. The integration of these principles into clinical practice has led to significant improvements in patient outcomes and has opened new avenues for therapeutic interventions.
The Science Behind Ischemia-Reperfusion Injury
Cellular Energy Depletion and Hypoxia
During the ischemic phase, cells experience severe oxygen and nutrient deprivation, leading to rapid depletion of cellular energy stores. The absence of oxygen forces cells to switch from aerobic to anaerobic metabolism, resulting in the accumulation of toxic metabolites and a dramatic decrease in ATP production. This metabolic shift triggers a cascade of cellular events that compromise the tissue’s ability to maintain normal function.
Calcium acts as a crucial second messenger during this phase, triggering the activation of multiple enzyme systems that become central to the subsequent injury process. The conversion of xanthine dehydrogenase to xanthine oxidase during ischemia sets the stage for massive oxygen radical production once blood flow is restored.
Reperfusion and Oxygen Radical Generation
The restoration of blood supply, while necessary for tissue survival, initiates a destructive sequence of events. Oxygen replenishment promotes enzymatic reactions that generate harmful free radicals, including superoxide radicals, hydrogen peroxide, and hydroxyl radicals. These reactive oxygen species cause direct damage to cellular structures, particularly endothelial cells lining blood vessels.
The production of these radicals is not merely a byproduct of reperfusion but represents an active pathological process that can cause more tissue damage than the original ischemic event. This phenomenon explains why immediate restoration of blood flow, while beneficial in principle, must be carefully managed to minimize additional injury.
Inflammatory Cascade Activation
Free radical production triggers the release of numerous inflammatory mediators, including histamine, platelet activating factor, leukotriene B4, thromboxane A2, tumor necrosis factor-alpha, and interleukin-1. These mediators orchestrate a complex inflammatory response that involves multiple cellular components and signaling pathways.
The inflammatory cascade leads to increased vascular permeability, activation of complement systems, and recruitment of inflammatory cells to the affected area. While inflammation is a necessary component of tissue repair, excessive or prolonged inflammatory responses can significantly impair healing and lead to chronic wound formation.
Leukocyte Rolling and Adherence
One of the most critical aspects of reperfusion injury involves the sequential interaction between circulating leukocytes and the vascular endothelium. This process occurs in distinct phases, each mediated by specific adhesion molecules expressed on endothelial surfaces.
| Phase | Adhesion Molecule | Timing | Function |
|---|---|---|---|
| Early Rolling | P-selectin | Within 1 minute | Initial leukocyte capture |
| Late Rolling | E-selectin | 2-6 minutes | Sustained rolling interaction |
| Adherence | ICAM/VCAM | 3-5 minutes | Firm leukocyte attachment |
The adherence of leukocytes to venular endothelium is associated with decreased local production of nitric oxide, leading to arteriolar vasoconstriction and creating a low-flow state that predisposes to intravascular thrombosis.
Clinical Applications in Skincare
Dermal Filler Complications Management
One of the most significant applications of ischemia-reperfusion principles in skincare involves managing vascular complications from dermal filler injections. When hyaluronic acid fillers inadvertently occlude blood vessels, they create an ischemic environment that can rapidly progress to tissue necrosis if not promptly addressed.
The management of these complications requires immediate recognition of ischemic signs and rapid intervention with hyaluronidase to dissolve the offending filler. However, practitioners must understand that simply restoring blood flow may not be sufficient and may even exacerbate tissue damage due to reperfusion injury mechanisms.
Successful management protocols now incorporate strategies to minimize reperfusion injury, including the use of antioxidants, anti-inflammatory agents, and careful monitoring of tissue response during the recovery phase. The timing of intervention is critical, as prolonged ischemia increases the severity of subsequent reperfusion injury.
Aesthetic Treatment Optimization
Understanding ischemia-reperfusion principles has led to the development of optimized treatment protocols for various aesthetic procedures. Practitioners now recognize that certain treatments may create temporary ischemic conditions that, while therapeutic in intent, must be carefully managed to prevent unwanted reperfusion effects.
This knowledge has influenced technique modifications, patient selection criteria, and post-treatment care protocols across multiple aesthetic modalities. The integration of these principles has resulted in improved safety profiles and enhanced treatment outcomes for patients undergoing cosmetic procedures.
Treatment Protocols and Management
Immediate Intervention Strategies
When ischemic injury is suspected, immediate intervention is crucial to minimize tissue damage and prevent progression to necrosis. The primary goals include rapid restoration of perfusion while simultaneously implementing measures to reduce reperfusion injury.
Hyaluronidase administration remains the gold standard for dissolving hyaluronic acid fillers causing vascular occlusion. However, the quantity, concentration, and injection technique must be carefully considered to optimize outcomes while minimizing additional tissue trauma from the injections themselves.
Concurrent administration of vasodilators, such as topical nitroglycerin or phosphodiesterase inhibitors, can help improve microcirculation and reduce the severity of ischemic injury. These agents work synergistically with hyaluronidase to restore tissue perfusion more effectively than either treatment alone.
Adjuvant Therapeutic Approaches
The management of ischemia-reperfusion injury in skincare extends beyond acute intervention to include comprehensive supportive care. Systemic therapies may include anti-inflammatory medications to reduce the inflammatory cascade, antibiotics to prevent secondary infection, and analgesics to manage patient discomfort.
Topical treatments play a crucial role in optimizing recovery outcomes. The application of appropriate wound dressings and topical agents that support the wound healing process while minimizing infection risk is essential for optimal patient recovery.
Hyperbaric oxygen therapy has emerged as a potential adjuvant treatment for severe cases of tissue ischemia. This treatment modality can help improve tissue oxygenation and may reduce the extent of tissue damage in selected cases.
Wound Healing and Recovery
Moist Wound Healing Principles
The application of moist wound healing principles has become fundamental to managing ischemic wounds resulting from reperfusion injury. Decades of research have demonstrated that maintaining an optimal moisture balance in wounds significantly accelerates healing, reduces infection rates, and minimizes scarring.
Appropriate wound dressings that maintain moisture while allowing gas exchange are essential for optimal healing outcomes. These dressings should also provide protection from external contamination while allowing for easy monitoring of healing progress.
The selection of topical agents should focus on products that facilitate collagen restoration, support elastin production, and enhance extracellular matrix formation. These components are crucial for restoring normal skin architecture and function following ischemic injury.
Factors Affecting Healing Outcomes
Multiple factors can influence the healing process following ischemia-reperfusion injury, and understanding these variables is crucial for optimizing patient outcomes. Patient-specific factors such as age, underlying health conditions, smoking status, and nutritional state can significantly impact healing capacity.
The extent and duration of initial ischemia directly correlate with healing complexity and time requirements. Longer periods of tissue hypoxia result in more extensive cellular damage and correspondingly longer recovery times.
Environmental factors, including wound care compliance, infection prevention measures, and appropriate activity modification, play important roles in determining final outcomes. Patient education and support are essential components of successful treatment protocols.
Monitoring and Assessment
Regular monitoring of healing progress is essential for identifying complications early and adjusting treatment protocols as needed. Clinical assessment should include evaluation of wound characteristics, signs of infection, and evidence of healing progression.
Photographic documentation provides valuable objective assessment tools and allows for systematic tracking of healing progress over time. This documentation is particularly important for complex cases that may require extended treatment periods.
Patient-reported outcomes, including pain levels, functional limitations, and cosmetic satisfaction, should be systematically evaluated throughout the treatment process to ensure comprehensive care delivery.
Prevention Strategies
Risk Assessment and Patient Selection
Preventing ischemia-reperfusion injury begins with thorough risk assessment and appropriate patient selection for aesthetic procedures. Understanding individual patient risk factors, including vascular anatomy variations, previous treatment history, and underlying health conditions, is crucial for minimizing complication risks.
Pre-treatment consultation should include detailed discussion of potential complications and their management, ensuring patients understand both the benefits and risks associated with their chosen treatments. This informed consent process should specifically address the possibility of vascular complications and their potential consequences.
Technique modifications based on individual patient anatomy and risk factors can significantly reduce the likelihood of vascular complications. This personalized approach to treatment planning represents best practice in modern aesthetic medicine.
Technique Optimization
Injection techniques that minimize the risk of vascular compromise have been developed based on understanding of facial vascular anatomy and ischemia-reperfusion principles. These techniques emphasize careful injection placement, appropriate needle selection, and constant awareness of vascular landmarks.
The use of blunt-tip cannulas in high-risk areas can reduce the likelihood of vessel puncture and subsequent filler embolization. However, practitioners must understand that these safety measures, while helpful, do not eliminate all risks of vascular complications.
Aspiration techniques, while controversial in their effectiveness, may provide additional safety measures when performing injections in high-risk vascular areas. The integration of multiple safety strategies provides the best approach to complication prevention.
Future Directions and Research
Emerging Therapeutic Approaches
Research into novel therapeutic approaches for preventing and treating ischemia-reperfusion injury continues to evolve. Antioxidant therapies, including both topical and systemic applications, show promise for reducing the severity of reperfusion injury when used as part of comprehensive treatment protocols.
Stem cell therapies and growth factor applications represent exciting frontiers in wound healing and tissue regeneration following ischemic injury. These biological therapies may offer enhanced healing capacity and improved cosmetic outcomes for affected patients.
Advanced wound dressings incorporating bioactive compounds and controlled-release drug delivery systems are being developed to optimize the wound healing environment and accelerate recovery processes.
Technology Integration
The integration of advanced imaging technologies and monitoring systems may improve early detection of ischemic complications and guide more precise treatment interventions. Real-time assessment tools could enable practitioners to identify problems earlier and implement corrective measures more effectively.
Artificial intelligence applications in risk assessment and treatment planning may help identify high-risk patients and optimize treatment protocols based on individual characteristics and historical outcome data.
Frequently Asked Questions
Q: How quickly does ischemia-reperfusion injury occur after dermal filler injection?
A: Ischemia-reperfusion injury can begin within minutes of vascular occlusion. The initial ischemic phase starts immediately upon vessel blockage, while reperfusion injury occurs when blood flow is restored, typically during treatment with hyaluronidase.
Q: What are the early warning signs of vascular compromise during aesthetic treatments?
A: Early signs include sudden severe pain, skin blanching or discoloration, decreased skin temperature, and loss of capillary refill. Any of these symptoms require immediate evaluation and potential intervention.
Q: Can ischemia-reperfusion injury be completely prevented during cosmetic procedures?
A: While risks can be significantly minimized through proper technique, anatomical knowledge, and safety protocols, complete elimination of risk is not possible. However, understanding these principles allows for rapid recognition and effective management when complications occur.
Q: How long does recovery typically take after ischemic skin injury?
A: Recovery time varies significantly based on the extent of initial injury, promptness of treatment, and individual patient factors. Minor ischemic events may resolve within days to weeks, while more severe injuries requiring wound care may take months for complete healing.
Q: Are there specific skincare products that help with ischemia-reperfusion recovery?
A: Products containing antioxidants, growth factors, and ingredients that support collagen synthesis can be beneficial during recovery. However, specific product selection should always be guided by healthcare professionals familiar with the patient’s condition and treatment history.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8903221/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3792800/
- https://en.wikipedia.org/wiki/Reperfusion_injury
- https://www.bmglabtech.com/en/blog/ischemia-reperfusion-research/
- https://www.escardio.org/static-file/Escardio/Education/Courses/Basic%20science%20summer%20school/Revised_Pagliaro.pdf
Read full bio of Sneha Tete












