Intermittent Fasting and Intestinal Tight Junctions: Mechanisms, Benefits, and Risks
Meal timing influences microbial harmony to strengthen your gut’s protective barrier.
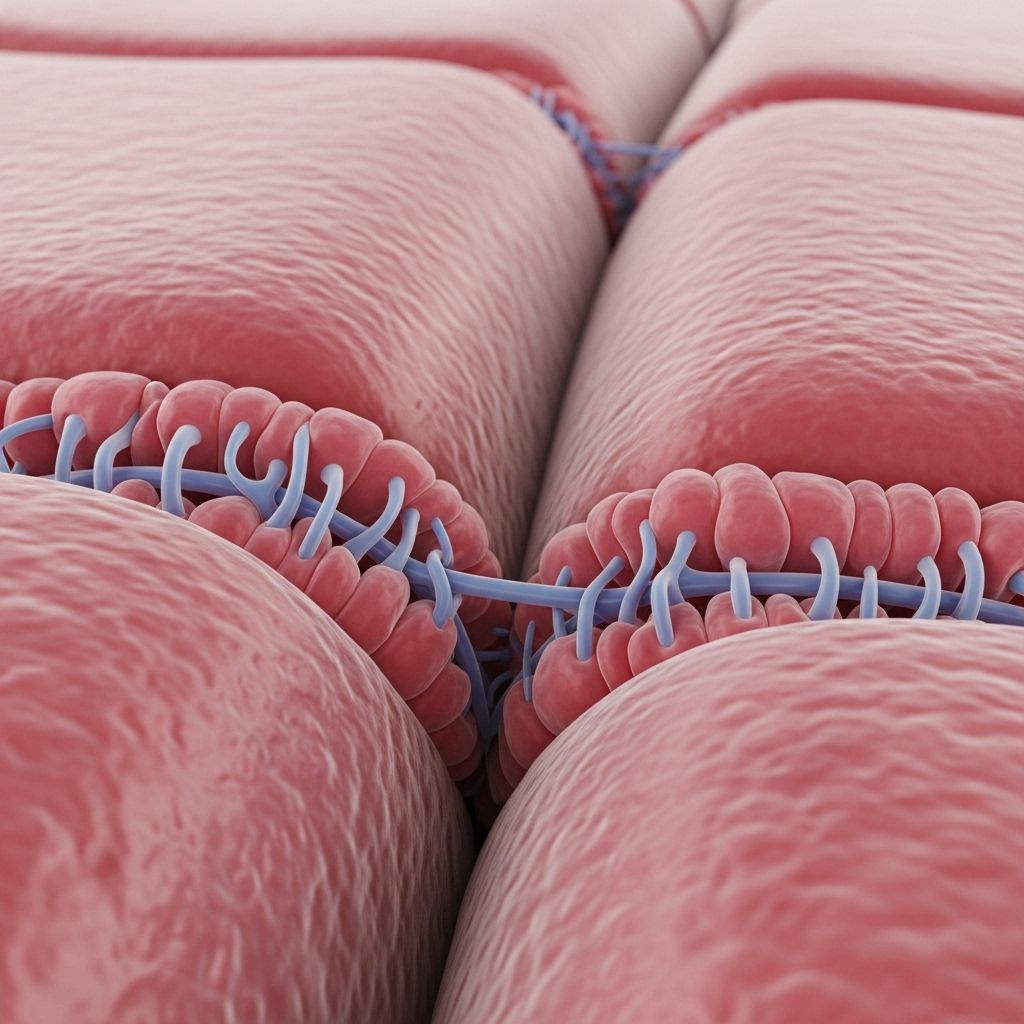
Table of Contents
- Introduction
- Understanding Intestinal Tight Junctions
- What is Intermittent Fasting?
- The Interplay Between Intermittent Fasting and the Gut Barrier
- Mechanisms: How Intermittent Fasting Impacts Tight Junctions
- Role of Gut Microbiota in Mediating Effects
- Benefits of Intermittent Fasting for Intestinal Barrier Function
- Risks and Potential Adverse Effects
- Clinical Implications and Future Directions
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction
Intermittent fasting (IF) has emerged as a popular nutritional intervention, with claims of benefits ranging from weight loss to improved metabolic health. However, research into its deeper cellular effects—especially on the integrity of the intestinal epithelium—remains ongoing. Central to gut health are tight junctions, protein complexes that regulate permeability in the intestinal barrier. Recent evidence highlights the intricate relationship between IF, tight junction function, and the gut microbiota, making this an area of critical interest for both clinicians and health-conscious individuals.
Understanding Intestinal Tight Junctions
Tight junctions are multiprotein complexes located at the apical region of epithelial cells lining the gut. They serve several essential functions:
- Regulate Paracellular Permeability: Tightly control movement of water, ions, and macromolecules between intestinal cells.
- Maintain Barrier Integrity: Prevent the translocation of harmful substances, such as toxins and pathogens, from the gut lumen into the bloodstream.
- Support Homeostasis: Play a critical role in maintaining immune balance and nutrient absorption.
Key proteins include claudins, occludin, and zonula occludens (ZO)-1. Any disruption in their expression or localization can lead to increased intestinal permeability (commonly referred to as “leaky gut”), predisposing to inflammation, metabolic disorders, and susceptibility to disease.
Table: Important Tight Junction Proteins and Functions
| Protein | Function |
|---|---|
| Claudin-1 | Primary barrier component; seals space between cells |
| Occludin | Regulates paracellular permeability and tight junction stability |
| ZO-1 | Anchors junctional components to the actin cytoskeleton |
What is Intermittent Fasting?
Intermittent fasting refers to various dietary patterns that alternate between periods of restricted or no caloric intake and periods of normal eating. Common regimens include:
- Time-restricted feeding (e.g., 16 hours fasting/8 hours eating each day)
- Alternate-day fasting (ADF: fasting every other day)
- 5:2 fasting (2 days per week of caloric restriction, 5 days normal eating)
IF has been studied primarily for its role in weight reduction and improvements in metabolic health (insulin sensitivity, glucose tolerance, lipid profiles), but recent focus has turned to its impacts on cellular and organ system physiology, particularly in the gut.
The Interplay Between Intermittent Fasting and the Gut Barrier
A healthy intestinal barrier depends on the proper functioning of tight junctions, robust epithelial cell regeneration, and a balanced microbiota. Both the metabolic milieu and the composition of gut microbes exert powerful influences on barrier integrity. Disruptions—whether from diet, stress, or dysbiosis—can compromise tight junctions and increase permeability.
IF, by modulating both host metabolism and gut microbial communities, introduces significant changes in the local environment experienced by epithelial cells, which may in turn affect tight junction dynamics.
Mechanisms: How Intermittent Fasting Impacts Tight Junctions
The relationship between IF and tight junctions operates on multiple levels—through direct effects on epithelial cell metabolism, modulation of signaling pathways, and alterations in the gut microbial ecosystem. The major mechanisms identified by research include:
- Reductions in Oxidative Stress: IF has been shown to decrease mitochondrial respiration and the production of reactive oxygen species (ROS) in the colon, mitigating obesity-driven damage and supporting barrier function.
- Modulation of Gene Expression: IF can influence the expression of tight junction genes such as claudin-1, occludin, and ZO-1, supporting their assembly and maintenance.
- Activation of Cellular Signaling Pathways: Short-chain fatty acids (SCFAs) produced by microbial fermentation, particularly butyrate, facilitate tight junction assembly via activation of AMP-activated protein kinase (AMPK).
- Promotion of Epithelial Renewal: The fasting state favors a metabolic environment conducive to epithelial cell regeneration and enhances barrier renewal capacity.
Figure: Pathways by Which IF May Reinforce Tight Junction Integrity
- Decrease in colonic mitochondrial oxygen consumption
- Reduction of ROS production, limiting oxidative damage
- Alteration in gut microbial composition, promoting beneficial species
- Increased SCFA production (notably butyrate)
Role of Gut Microbiota in Mediating Effects
The gut microbiota acts as a key intermediary in the relationship between IF and intestinal barrier function. Research demonstrates that:
- Microbial Metabolites: Commensal bacteria produce SCFAs (e.g., butyrate) that directly strengthen tight junctions and promote barrier integrity.
- Bacterial Diversity: IF leads to an increase in microbial diversity, favoring beneficial species (e.g., Lactobacillus intestinalis).
- Protection Against Pathogens: A balanced microbiome outcompetes pathogenic bacteria, whose toxins can disrupt tight junctions.
- Antibiotic Sensitivity: Elimination of the microbiota through antibiotics abolishes the beneficial effects of IF on antioxidative stress reduction and barrier protection.
Disruption or depletion of beneficial microbes, however, reverses these positive outcomes, increasing susceptibility to inflammation and metabolic disease.
Benefits of Intermittent Fasting for Intestinal Barrier Function
- Improved Epithelial Renewal: IF aids in restoring the renewal process of colonic epithelial cells, enhancing overall barrier integrity.
- Reduced Oxidative Damage: Decreased mitochondrial respiration and ROS in the colon reduce the oxidative burden, supporting tight junction maintenance.
- Enhanced Tight Junction Protein Expression: SCFA-mediated signaling promotes the assembly and function of tight junction proteins such as claudin-1 and occludin.
- Improved Glucose and Lipid Metabolism: By preserving barrier function, IF contributes to better metabolic profiles, lowering the risk of obesity, diabetes, and hepatic steatosis.
- Alleviation of Age-related Barrier Damage: Alternate day fasting may protect against aging-induced deterioration in intestinal epithelial integrity.
Risks and Potential Adverse Effects
While intermittent fasting offers multiple benefits, it may also pose risks, especially under certain physiological conditions:
- Disruption in Offspring: Maternal IF prior to and during pregnancy may negatively impact the development and maintenance of tight junctions in offspring, especially when followed by high-fat diets. This is evidenced by reduced claudin-1 expression, increased intestinal permeability, elevated circulating LPS (a marker of barrier dysfunction), and greater inflammatory activity.
- Dependence on Microbiota: The protective effect of IF relies on a balanced microbiota. Disruption through antibiotics or poor microbial diversity can negate beneficial outcomes and impair barrier integrity.
- Potential for Inflammatory Activation: In certain contexts—particularly when IF leads to microbial dysbiosis—intestinal inflammatory markers such as TNF-α and IL-6 may increase.
These observations underscore the importance of context, duration, and individual gut microbial health in determining the net outcome of IF on intestinal tight junctions.
Table: Potential Benefits and Risks of IF for Tight Junction Health
| Benefits | Risks |
|---|---|
| Reduced oxidative stress, enhanced barrier function, improved metabolic homeostasis | Disrupted barrier in offspring from maternal IF, loss of benefit with antibiotic use, risk of inflammation in dysbiosis |
Clinical Implications and Future Directions
Given the evidence, integrating intermittent fasting as a therapeutic intervention for metabolic and inflammatory disorders should be approached with consideration of individual microbiota status, life stage, and existing metabolic health. Suggested avenues include:
- Screening for gut microbiota composition prior to starting IF, especially in vulnerable populations.
- Combining IF with probiotic or prebiotic therapy to support beneficial microbial populations.
- Special caution with IF during pregnancy and lactation, given demonstrated adverse effects on offspring intestinal barrier function.
- Personalization of IF regimens (duration, pattern) to maximize benefits and minimize risks.
- Further research into sex- and age-specific responses, long-term outcomes, and transgenerational effects.
Frequently Asked Questions (FAQs)
Q: How does intermittent fasting improve gut barrier function?
A: IF reduces oxidative stress and supports the renewal of epithelial cells while promoting production of beneficial metabolites by the gut microbiota, all of which strengthen tight junction integrity.
Q: Can intermittent fasting ever damage the intestinal barrier?
A: In certain contexts, especially when combined with high-fat diets or during critical developmental windows like pregnancy, IF may disrupt tight junction protein expression and increase gut permeability, particularly in offspring.
Q: Is the positive effect of IF on tight junctions dependent on the microbiome?
A: Yes. Loss of beneficial bacteria—such as through antibiotic use—eliminates many of IF’s advantages for gut barrier integrity.
Q: Which tight junction proteins are most impacted by fasting?
A: Research highlights claudin-1 as the most sensitive to changes in metabolic state and microbial signaling. Its expression can increase with healthy fasting or decrease under adverse conditions, impacting barrier tightness.
Q: Should pregnant women practice intermittent fasting?
A: Current research suggests caution, as maternal IF prior to and during pregnancy can negatively impact offspring’s gut barrier development. Always consult with a healthcare provider before adopting such dietary patterns during pregnancy or lactation.
Conclusion
Intermittent fasting exerts multifaceted effects on intestinal tight junctions, primarily through modulating oxidative stress, epithelial metabolism, and—most crucially—gut microbial composition. While IF generally supports barrier function and metabolic health, special care is necessary under specific conditions such as pregnancy, dysbiosis, or chronic inflammation. The net impact depends on the balance between beneficial microbial metabolites, genetic regulation of tight junction proteins, and host metabolic state. Attention to personalized nutrition and comprehensive microbiome management will be essential in safely leveraging the health potential of intermittent fasting for maintaining and restoring gut barrier integrity.
References
Read full bio of medha deb












