Inflammation: The Root Cause of Heart Disease and Metabolic Syndrome Explained
Every meal, workout, and habit can shape your body's defense and support lasting health.
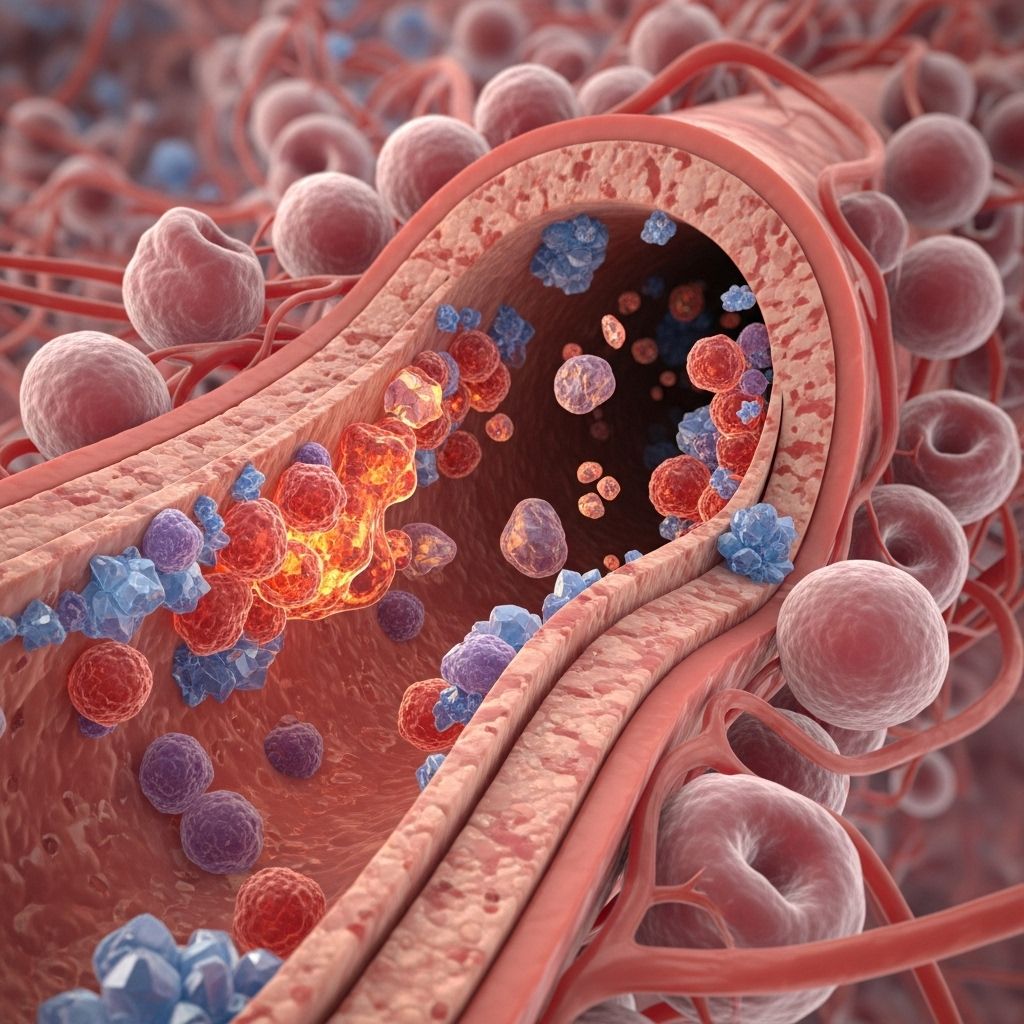
Table of Contents
- Understanding Inflammation
- Acute vs. Chronic Inflammation
- Inflammation and Heart Disease
- Inflammation and Metabolic Syndrome
- Shared Mechanisms Between Heart Disease and Metabolic Disorders
- Inflammatory Biomarkers and Risk Assessment
- Therapeutic Strategies to Reduce Inflammation
- Lifestyle Interventions to Combat Chronic Inflammation
- Emerging Research and Future Directions
- Frequently Asked Questions (FAQs)
Understanding Inflammation
Inflammation is the body’s natural defense mechanism against injury, infection, or harmful stimuli. When you sprain your ankle or catch a cold, your immune system sends white blood cells to the affected area, causing redness, swelling, and heat—classic signs of acute inflammation. This process is vital for healing and protecting the body from further harm.
However, when inflammation becomes persistent or exaggerated, it can turn from a protective response into a destructive force. Chronic inflammation lingers for weeks, months, or even years, silently damaging tissues and organs and contributing to the development of numerous diseases, including heart disease and metabolic disorders.
Acute vs. Chronic Inflammation
Acute inflammation is short-lived, typically resolving within days as the immune system clears the threat and repairs tissue. It is characterized by the rapid recruitment of immune cells, such as neutrophils and macrophages, to the site of injury or infection.
Chronic inflammation, in contrast, is a prolonged state of immune activation. It can result from unresolved acute inflammation, persistent infections, autoimmune reactions, or exposure to environmental toxins such as cigarette smoke and excess fat. Over time, chronic inflammation damages healthy tissues, disrupts normal organ function, and is now recognized as a root cause of many chronic diseases.
The transition from acute to chronic inflammation is not always clear-cut. In some cases, the immune system fails to resolve the inflammatory response properly, leading to a vicious cycle of tissue damage and further immune activation.
Inflammation and Heart Disease
Heart disease, particularly atherosclerosis, is fundamentally an inflammatory condition. Atherosclerosis develops when cholesterol-rich plaques build up in the walls of arteries, narrowing them and restricting blood flow. Inflammation plays a central role in every stage of this process:
- Initiation: Damage to the endothelial lining of arteries (from high blood pressure, smoking, or high cholesterol) triggers an inflammatory response. Immune cells, especially monocytes, migrate into the artery wall and transform into macrophages, which engulf oxidized low-density lipoprotein (LDL) cholesterol particles.
- Plaque Formation: These lipid-laden macrophages, called foam cells, accumulate and form fatty streaks. Smooth muscle cells migrate into the area, forming a fibrous cap over the plaque.
- Plaque Rupture: Chronic inflammation destabilizes the plaque. Inflammatory cytokines, such as interleukin-1β (IL-1β), IL-6, and tumor necrosis factor-alpha (TNF-α), weaken the fibrous cap, making it more likely to rupture. When a plaque ruptures, it can trigger blood clot formation, leading to a heart attack or stroke.
Notably, even in individuals with well-controlled cholesterol levels, persistent inflammation remains a significant risk factor for cardiovascular events. Blood tests measuring inflammatory markers, such as C-reactive protein (CRP), are now recognized as powerful predictors of heart disease risk—sometimes even more so than traditional cholesterol measurements.
After a heart attack, inflammation is initially beneficial, helping to clear dead tissue and initiate repair. However, if the inflammatory response is not properly resolved, it becomes chronic, impairing cardiac healing and contributing to heart failure.
Inflammation and Metabolic Syndrome
Metabolic syndrome is a cluster of conditions—including obesity, insulin resistance, high blood pressure, and dyslipidemia—that increase the risk of heart disease, stroke, and type 2 diabetes. Chronic inflammation is a key driver of these metabolic disturbances.
- Obesity: Excess fat, especially visceral fat, produces pro-inflammatory cytokines (adipokines) such as leptin and resistin, which promote systemic inflammation.
- Insulin Resistance: Inflammation interferes with insulin signaling, leading to impaired glucose uptake by cells and elevated blood sugar levels.
- Dyslipidemia: Chronic inflammation alters lipid metabolism, increasing levels of triglycerides and decreasing high-density lipoprotein (HDL) cholesterol.
These metabolic changes create a vicious cycle: inflammation worsens metabolic dysfunction, which in turn amplifies inflammation. Over time, this cycle damages blood vessels, promotes atherosclerosis, and increases the risk of cardiovascular complications.
Shared Mechanisms Between Heart Disease and Metabolic Disorders
Both heart disease and metabolic syndrome share underlying inflammatory pathways. Key mechanisms include:
- Immune Cell Activation: Macrophages and other immune cells release inflammatory cytokines that promote insulin resistance and vascular dysfunction.
- Oxidative Stress: Reactive oxygen species (ROS) generated during inflammation damage cells, lipids, and DNA, exacerbating both metabolic and cardiovascular disease.
- Endothelial Dysfunction: Inflammation impairs the function of the endothelial lining of blood vessels, reducing their ability to dilate and increasing the risk of clot formation.
- Hormonal Imbalance: Chronic inflammation disrupts the balance of hormones involved in metabolism and vascular health, such as insulin, adiponectin, and cortisol.
| Condition | Key Inflammatory Mechanisms | Health Consequences |
|---|---|---|
| Heart Disease | Plaque formation, immune cell infiltration, cytokine release | Atherosclerosis, heart attack, stroke |
| Metabolic Syndrome | Adipokine release, insulin resistance, oxidative stress | Type 2 diabetes, obesity, hypertension |
Inflammatory Biomarkers and Risk Assessment
Identifying individuals at risk for inflammation-driven diseases relies on measuring specific biomarkers:
- C-reactive protein (CRP): A widely used marker of systemic inflammation. Elevated CRP levels predict cardiovascular events independently of cholesterol levels.
- Interleukins (IL-6, IL-1β): Cytokines that promote inflammation and are associated with both heart disease and metabolic disorders.
- Tumor Necrosis Factor-alpha (TNF-α): A key mediator of inflammation in obesity and insulin resistance.
These biomarkers, along with traditional risk factors like cholesterol and blood pressure, provide a more comprehensive assessment of cardiovascular and metabolic risk.
Therapeutic Strategies to Reduce Inflammation
Targeting inflammation offers a promising approach to preventing and treating heart disease and metabolic syndrome. Current and emerging strategies include:
- Statins: While primarily used to lower cholesterol, statins also have anti-inflammatory effects and can reduce CRP levels.
- Anti-cytokine Therapies: Drugs targeting specific inflammatory cytokines (e.g., IL-1β inhibitors) have shown benefit in reducing cardiovascular events, though they may increase infection risk.
- Specialized Pro-resolving Mediators (SPMs): These are naturally occurring molecules that help resolve inflammation without suppressing the immune system. Research suggests that boosting SPMs could promote healing after a heart attack and prevent chronic inflammation.
However, simply blocking all inflammation is not the answer—acute inflammation is essential for healing. The goal is to restore balance, ensuring that inflammation resolves appropriately after serving its purpose.
Lifestyle Interventions to Combat Chronic Inflammation
Lifestyle modifications are foundational for reducing chronic inflammation:
- Healthy Diet: Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats (e.g., omega-3 fatty acids). Avoid processed foods, trans fats, and excessive sugar.
- Regular Exercise: Physical activity reduces inflammatory markers and improves metabolic health.
- Weight Management: Losing excess weight, particularly abdominal fat, reduces the production of pro-inflammatory adipokines.
- Smoking Cessation: Smoking is a major source of oxidative stress and inflammation.
- Stress Reduction: Chronic stress increases sympathetic nervous system activity and inflammatory cytokine release. Mindfulness, yoga, and adequate sleep can help manage stress.
Emerging Research and Future Directions
Research continues to uncover new links between inflammation, heart disease, and metabolic disorders:
- Microbiome: The gut microbiome influences systemic inflammation and may play a role in cardiovascular and metabolic health.
- Personalized Medicine: Identifying individuals with a high inflammatory burden could allow for targeted therapies.
- Resolution Pharmacology: Developing drugs that enhance the resolution of inflammation (rather than merely suppressing it) represents a novel therapeutic approach.
Future clinical trials will likely focus on combining anti-inflammatory therapies with lifestyle interventions to achieve optimal outcomes.
Frequently Asked Questions (FAQs)
Q: What is the difference between acute and chronic inflammation?
A: Acute inflammation is a short-term, protective response to injury or infection, while chronic inflammation is a prolonged state that can damage tissues and contribute to disease.
Q: How does inflammation cause heart disease?
A: Inflammation drives the development and progression of atherosclerosis by promoting plaque formation, destabilizing plaques, and increasing the risk of heart attack and stroke.
Q: Can inflammation cause metabolic problems like diabetes?
A: Yes, chronic inflammation contributes to insulin resistance, obesity, and dyslipidemia, all key components of metabolic syndrome.
Q: Are there blood tests for inflammation?
A: Yes, tests such as C-reactive protein (CRP) and certain interleukins can measure systemic inflammation and predict cardiovascular risk.
Q: What lifestyle changes can reduce chronic inflammation?
A: A healthy diet, regular exercise, weight management, smoking cessation, and stress reduction are all effective strategies for lowering inflammation.
Q: Are anti-inflammatory drugs safe for heart disease prevention?
A: Some drugs that target specific inflammatory pathways have shown benefit, but they can increase infection risk. Lifestyle interventions remain the cornerstone of prevention.
Q: Can inflammation be reversed?
A: In many cases, reducing exposure to inflammatory triggers (e.g., poor diet, lack of exercise, smoking) and adopting a healthier lifestyle can significantly lower chronic inflammation and its associated risks.
Chronic inflammation is now recognized as a root cause of heart disease and metabolic disorders. Understanding its mechanisms, recognizing its biomarkers, and implementing targeted therapies and lifestyle changes can help break the cycle of inflammation and reduce the burden of these chronic diseases.
References
- https://hscweb3.hsc.usf.edu/blog/2020/09/30/focused-on-the-root-causes-of-cardiac-inflammation/
- https://www.health.harvard.edu/heart-health/new-insights-about-inflammation
- https://www.bhf.org.uk/informationsupport/heart-matters-magazine/research/what-is-inflammation
- https://pubmed.ncbi.nlm.nih.gov/36361701/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8315628/
- https://www.nature.com/articles/d41586-021-01453-6
Read full bio of Sneha Tete












