Identifying and Treating Swollen Lymph Nodes: Causes, Diagnosis, and Management Across Ages and Conditions
Recognizing gland enlargement early can prevent complications and guide proper care.
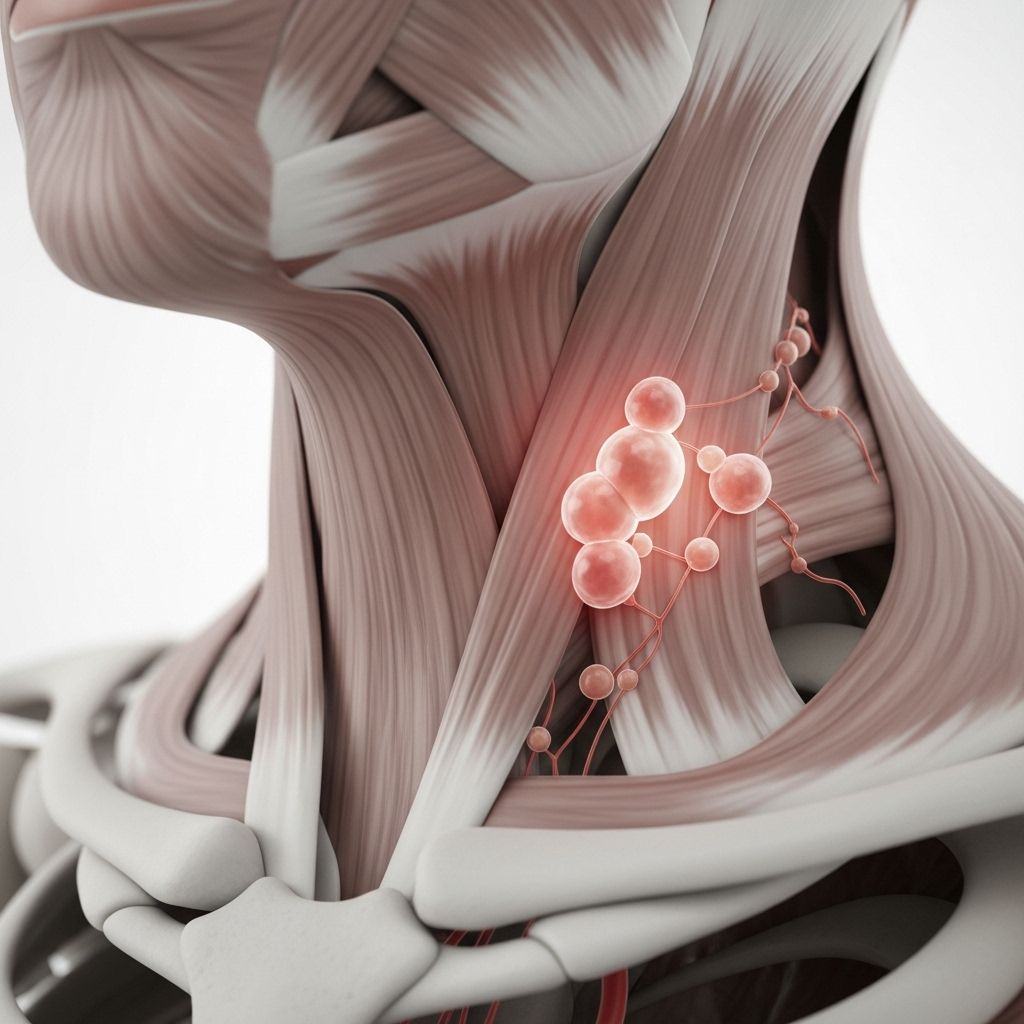
Table of Contents
- Overview: The Role of Lymph Nodes in Health
- Symptoms and Signs of Swollen Lymph Nodes
- Causes: Why Do Lymph Nodes Swell?
- Diagnosis: Tests and Physical Examination
- Treatment Options for Swollen Lymph Nodes
- Prevention and Self-Care
- Potential Complications and When to See a Doctor
- Frequently Asked Questions (FAQ)
Overview: The Role of Lymph Nodes in Health
Lymph nodes are small, bean-shaped organs distributed strategically throughout the body, primarily in the neck, armpits, chest, abdomen, and groin. They act as critical hubs within the lymphatic system, filtering lymph fluid and housing infection-fighting immune cells. When infection or inflammation occurs, lymph nodes can become swollen—a condition referred to as lymphadenopathy.
Swollen lymph nodes themselves are not a disease; instead, they signal that the body’s immune system is responding to some underlying issue, such as infection, inflammation, or, less commonly, cancer.
Symptoms and Signs of Swollen Lymph Nodes
Recognizing swollen lymph nodes can be pivotal for early intervention and appropriate care. The most common features include:
- Visible or palpable lumps: Swollen lymph nodes may feel like soft, round bumps under the skin, often the size of a pea or grape.
- Pain or tenderness: Swelling is often accompanied by tenderness, especially when touched or during movement (e.g., turning the neck, bending limbs).
- Redness and warmth: Skin overlying swollen lymph nodes may be red or warm due to underlying inflammation.
- Additional symptoms: Depending on the underlying cause, symptoms may include fever, coughing, fatigue, chills, sore throat, runny nose, night sweats, or unexplained weight loss.
The location of the swelling often points to the area of infection or inflammation—for example, swollen nodes in the neck may follow a throat or ear infection, while those in the groin may relate to pelvic diseases or infections.
Causes: Why Do Lymph Nodes Swell?
Understanding why lymph nodes swell is essential for guiding further evaluation and treatment. Causes fall into three broad categories:
1. Infections
- Viral infections: Common cold, influenza, mononucleosis, rubella, HIV.
- Bacterial infections: Strep throat, sinusitis, bacterial pharyngitis, tuberculosis, cat scratch fever, tooth abscesses.
- Other infectious agents: Toxoplasmosis, Lyme disease, herpes simplex.
- Sexually transmitted infections (STIs): Syphilis, gonorrhea (typically swelling in the groin).
2. Immune System Disorders
- Autoimmune diseases: Systemic lupus erythematosus, rheumatoid arthritis, Sjogren’s syndrome.
3. Cancers
- Cancer spreading to lymph nodes: Malignancies such as leukemia, Hodgkin’s lymphoma, non-Hodgkin’s lymphoma, Sézary syndrome, metastatic carcinoma.
4. Other Causes
- Allergic reactions: Strong immune responses to allergens can cause temporary swelling.
- Medications: Certain drugs (antiseizure, antimalarial, etc.) or allergic reactions to medications.
- Mouth conditions: Gingivitis, mouth sores.
- Other inflammatory disorders: Sarcoidosis, stress.
Diagnosis: Tests and Physical Examination
Tackling the underlying cause of swollen lymph nodes starts with a systematic approach to diagnosis:
- Medical history: Providers gather information about the onset, duration, and associated symptoms (e.g., fever, night sweats, recent infections).
- Physical examination: Physicians palpate lymph nodes to assess location, size, tenderness, mobility, and warmth.
- Blood tests: A complete blood count (CBC) and other lab tests check for infection, inflammation, or malignancy.
- Imaging studies: X-rays, CT scans, or ultrasounds may be done to look for deep-seated infection, tumors, or involvement in organs such as the chest or abdomen.
- Biopsy: A needle or excisional biopsy may be performed to analyze lymph node tissue for signs of cancer or specific infectious agents.
| Diagnostic Tool | Purpose | When Used |
|---|---|---|
| Medical history | Identifies cause, symptom progression | First visit |
| Physical examination | Assesses location, size, pain, warmth | First visit |
| Blood tests | Infection, inflammation, cancer markers | If cause unclear or serious suspicion |
| Imaging studies | Views deep nodes, underlying mass | Persistent or unexplained swelling |
| Biopsy | Definitive diagnosis (cancer, infection) | Persistent, hard, or atypical swelling |
Treatment Options for Swollen Lymph Nodes
The choice of treatment depends entirely on the underlying cause of swelling:
- Viral infections: Most cases resolve on their own as the infection subsides. Supportive care (rest, fluids, pain relief) may be recommended.
- Bacterial infections: Treated with appropriate antibiotics, which often lead to rapid reduction in swelling once the bacteria are controlled.
- HIV or other chronic infections: Require disease-specific therapy and sometimes long-term management.
- Autoimmune disorders: Treated with medications that suppress the overactive immune system, such as corticosteroids, immunosuppressive therapy, or biologics.
- Cancer: Treatment focuses on the primary malignancy and can involve surgery (removal of affected nodes), radiation therapy, chemotherapy, or combinations thereof.
- Medication-induced swelling: Stopping or switching the offending drug may resolve swelling after consulting a physician.
- Allergic reactions: Symptoms usually subside once the allergen is removed; antihistamines or corticosteroids might be required for severe reactions.
At-Home Care for Mild Cases
- Apply a warm, moist compress to relieve discomfort.
- Over-the-counter pain relievers such as acetaminophen or ibuprofen can help pain and inflammation.
- Increase fluid intake and rest.
- Monitor for changes in size, pain, or systemic symptoms.
Prevention and Self-Care
While not all cases are preventable, overall health measures can lower risk:
- Practice good hygiene to reduce risk of infection.
- Keep up with vaccinations (e.g., influenza, COVID-19, HPV).
- Avoid contact with known allergens and practice allergy management if needed.
- Manage chronic conditions (diabetes, autoimmune diseases) under a physician’s guidance.
- Attend regular check-ups, especially for those with cancer risk factors.
Potential Complications and When to See a Doctor
Most swollen lymph nodes are harmless and resolve with time or minimal intervention. However, seek medical attention if:
- Nodes are significantly enlarged (>2 cm), hard, fixed, or rubbery.
- Swelling persists beyond 2-4 weeks without improvement.
- You experience systemic symptoms: persistent fever, night sweats, unexplained weight loss.
- Mucosal or skin changes over swollen nodes appear (redness, warmth, ulceration).
- Difficulty breathing, swallowing, or severe throat swelling develops.
Complications can range from localized pus formation (abscess) to signaling serious underlying disease, such as lymphoma or metastatic cancer. Early evaluation is key for effective management.
Frequently Asked Questions (FAQ)
Q: How do I know if my swollen lymph node is serious?
A: Seek medical advice if a node is hard, growing rapidly, persistently swollen for weeks, or associated with fever, night sweats, weight loss, or other concerning symptoms.
Q: Can allergies cause swollen lymph nodes?
A: Yes, especially in individuals with strong reactions to allergens. Swelling is usually temporary and associated with exposure to the specific allergen.
Q: Are swollen lymph nodes always a sign of cancer?
A: No. The vast majority of cases are related to infection or immune response. Cancer is a rare cause, but should be considered in persistent or atypical cases.
Q: Should I treat swollen lymph nodes at home?
A: Many mild cases related to infections resolve with rest, fluids, warm compresses, and pain relief. Consult a doctor if swelling persists, worsens, or is accompanied by systemic symptoms.
Q: What does a lymph node biopsy involve?
A: A healthcare provider uses a needle or small incision to remove tissue from a lymph node for microscopic examination. This helps diagnose the cause, including cancer or specific infections.
Q: What are risk factors for malignant lymph node problems?
A: Age over 40, male sex, family history of lymphoma, persistent unexplained swelling, and associated symptoms (fever, weight loss, night sweats) increase risk.
Conclusion
Swollen lymph nodes are a common clinical finding signaling the body’s efforts to fight infection, inflammation, or, rarely, malignancy. Systematic identification, thorough evaluation, and targeted therapy ensure optimal outcomes for patients across all ages and health conditions. Awareness of complications and timely medical consultation are essential for preserving health. The guide above provides a thorough, authoritative framework for patients and caregivers to understand and manage this condition responsibly.
References
- https://www.healthline.com/health/swollen-lymph-nodes
- https://www.medicalnewstoday.com/articles/324105
- https://www.mayoclinic.org/diseases-conditions/swollen-lymph-nodes/diagnosis-treatment/drc-20353906
- https://www.unitypoint.org/news-and-articles/swollen-lymph-nodes-causes-treatments-and-when-to-go-to-the-doctor
- https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/lymphatic-disorders/swollen-lymph-nodes
- https://my.clevelandclinic.org/health/symptoms/15219-swollen-lymph-nodes
- https://www.mountsinai.org/health-library/symptoms/swollen-lymph-nodes
- https://my.clevelandclinic.org/health/diseases/21695-swollen-lymph-nodes-in-the-groin
- https://www.aafp.org/pubs/afp/issues/1998/1015/p1313.html
Read full bio of Sneha Tete












