Identifying and Managing Herpangina (Coxsackievirus): A Comprehensive Guide to Diagnosis, Symptoms, Treatment, and Prevention
Recognizing early signs and gentle home care can ease discomfort and speed recovery.
Identifying and Managing Herpangina (Coxsackievirus): A Comprehensive Guide
Herpangina is an acute viral illness most frequently seen in children, characterized by painful ulcers and sores inside the mouth, high fever, and sore throat. It is most commonly caused by Coxsackievirus A — a member of the enterovirus family. This guide provides an in-depth overview of the disease, including its causes, symptoms, diagnosis, management, and essential prevention strategies for both children and adults.
Table of Contents
- What is Herpangina?
- Causes & Risk Factors
- Transmission of Herpangina
- Signs and Symptoms
- Diagnosis
- Differential Diagnosis
- Treatment and Management
- Home Care Recommendations
- Complications
- Prevention Strategies
- Frequently Asked Questions (FAQs)
What is Herpangina?
Herpangina is an acute, self-limiting illness caused by enteroviruses, most commonly by strains of Coxsackie A virus. Rarely, enterovirus 71 and echoviruses can also be responsible. It is characterized by the sudden onset of high fever, sore throat, headache, and distinctive ulcerative lesions in the mouth and throat. Herpangina is especially prevalent in children aged 3 to 10 years, but cases have also been documented in infants, teenagers, and adults.
Causes & Risk Factors
The primary causative agent is the Coxsackie A virus, although other enteroviruses can also trigger the infection. The illness is highly contagious and spreads primarily through oral-oral or fecal-oral routes. The highest incidence occurs during the summer and early fall months. Key risk factors include:
- Close contact with an infected individual, especially in group settings (daycares, schools)
- Poor hand hygiene
- Exposure to respiratory droplets or fecal contamination
- Younger age (especially children)
- Weakened immune systems or underlying conditions
Transmission of Herpangina
The virus is shed in saliva, nasal mucus, and stool of infected individuals. Transmission can occur via:
- Direct person-to-person contact: Kissing, hugging, or caring for sick children.
- Contaminated objects: Toys, eating utensils, and surfaces.
- Respiratory droplets: Coughing or sneezing.
- Fecal-oral route: Improper handwashing after diaper changes or using the bathroom.
Herpangina is most contagious during the first week of illness, but the viruses can be excreted for weeks, particularly in stool.
Signs and Symptoms
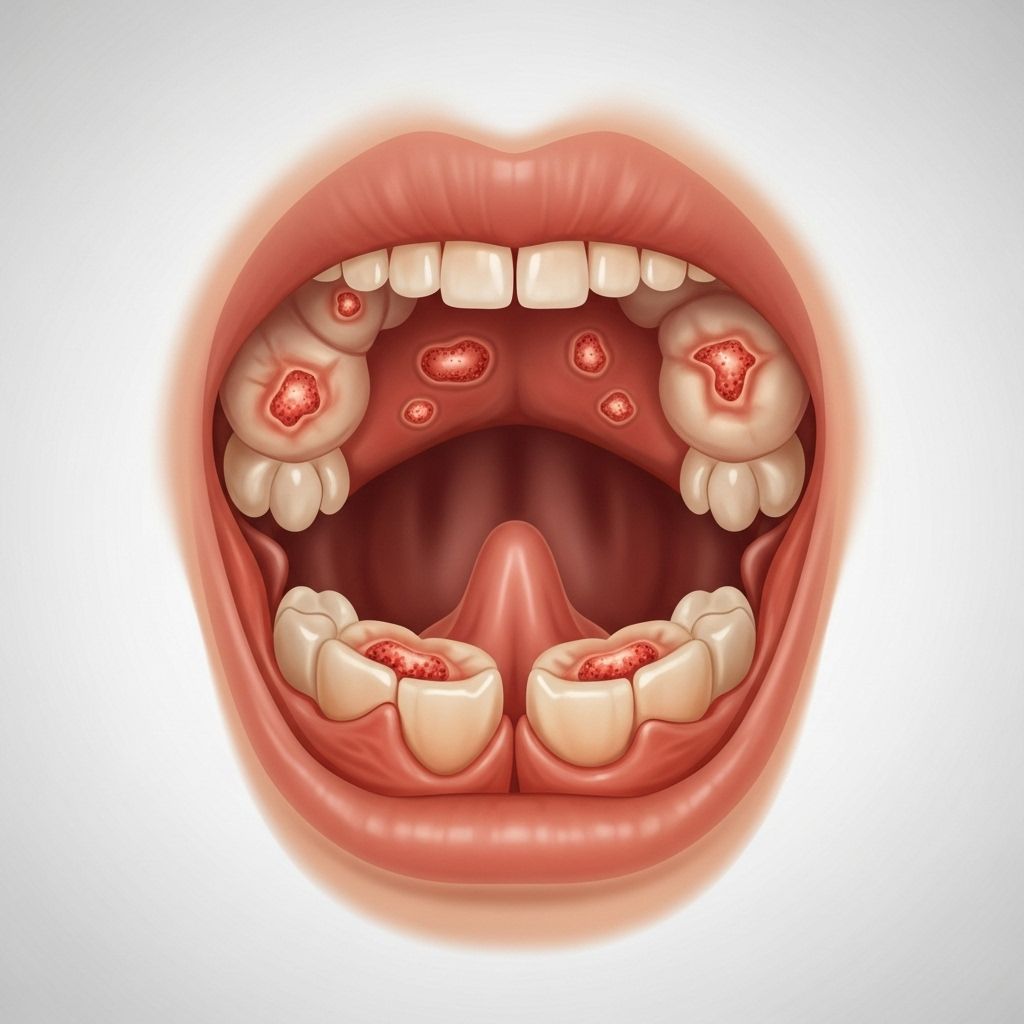
Symptoms typically start abruptly and vary in severity. The classic sequence involves a sudden high fever, followed by oral discomfort and vesicular lesions. The course usually lasts 3 to 7 days.
- Fever: Often high (up to 40°C/104°F), lasting 1–4 days
- Sore throat: Severe pain, especially on swallowing
- Headache and malaise
- Loss of appetite and poor feeding
- Vesicles and ulcers: Small (2–4 mm diameter) grayish or yellowish blisters, surrounded by a red halo, usually on the soft palate, tonsillar pillars, uvula, or posterior pharynx. These vesicles rupture and form shallow, discrete ulcers
- Neck pain or stiffness (occasionally)
- Cervical lymphadenopathy: Swollen neck lymph nodes
- Irritability, fussiness (in young children)
Most patients will have between 2 to 12 characteristic ulcers in the back of the mouth. Some children experience mild or no symptoms, while others may become significantly ill—especially those with compromised immune systems.
Diagnosis
Herpangina is best diagnosed by a thorough clinical history and physical examination. Laboratory tests and throat swabs are not typically required, as the ulcers have a unique appearance.
- Distinctive oral ulcers: Key feature for diagnosis
- Location of lesions: Soft palate, tonsillar pillars, posterior pharynx
- No routine blood tests: Laboratory diagnostics only if severe, atypical, or immunocompromised cases are suspected
- Clinical differential: Exclusion of similar conditions (see below)
Herpangina can sometimes resemble other viral illnesses (see differential diagnosis below), so accurate identification is essential for appropriate management.
Differential Diagnosis
Several illnesses can mimic herpangina; careful inspection and history-taking help distinguish them:
- Hand, foot, and mouth disease (HFMD): Caused by similar viruses, but presents with additional lesions on hands, feet, or buttocks
- Herpetic gingivostomatitis: More widespread, possibly involving lips, gums, and buccal mucosa with tender, clustered ulcers caused by herpes simplex virus
- Streptococcal pharyngitis: Typically lacks ulcerative mouth lesions; tonsillar exudate is more common
- Herpes zoster: Uncommon in children; lesions follow a dermatomal pattern
Treatment and Management
Herpangina is self-limited, and most children recover without complications in roughly 7 days. Supportive care is the cornerstone of treatment.
Medications for Symptom Relief
- Antipyretics: Acetaminophen (paracetamol) or ibuprofen for fever and pain. Adjust dosing by patient age and consult a healthcare provider if unsure.
- Avoid aspirin: Especially for children and teenagers, due to the risk of Reye’s syndrome.
- Topical anesthetics: Throat lozenges, gels, or mouthwashes containing mild anesthetics (numbing agents) may help, but avoid strong anesthetics in young children due to potential toxicity risks.
- Saltwater or saline rinses: Helpful for oral comfort and hygiene. For infants, use a soft saline wipe.
Dietary and Fluid Recommendations
- Encourage fluids: Cold water, milk, and ice pops are soothing; prevent dehydration
- Avoid irritants: Citrus juices, carbonated drinks, spicy, salty, or acidic foods; these may increase oral discomfort
- Offer soft, bland foods: Yogurt, applesauce, smoothies, or puddings
Additional Supportive Measures
- Rest: Ample rest helps the body recover
- Monitor for signs of dehydration: Decreased urination, dry mouth, listlessness, sunken eyes—seek medical advice if suspected
- Good oral hygiene: Maintain gentle oral care to prevent secondary infection
- Isolation: Keep affected children home from school or daycare until fever and active sores have resolved to minimize spread
Antibiotics are not effective because herpangina is a viral, not a bacterial, infection.
Home Care Recommendations
- Ensure regular intake of fluids—small sips throughout the day are best if swallowing is difficult
- Try cold, bland foods; avoid giving foods that are too hot or require much chewing
- Consider cool compresses for fever reduction
- Use over-the-counter medication as advised by your healthcare provider
- Gentle saline mouth rinses after meals and before bed help maintain oral hygiene
Complications
Most cases resolve without lasting effects. However, rare complications can arise, particularly in vulnerable groups (infants, immunocompromised, those with underlying health issues).
- Dehydration: Most common complication, due to difficulty swallowing and reduced fluid intake
- Febrile seizures: Sometimes seen in children with high fevers
- Viral meningitis or encephalitis: Extremely rare but serious
Seek immediate care if there are signs of persistent vomiting, severe headache, confusion, stiff neck, difficulty breathing, or other neurologic symptoms.
Prevention Strategies
No vaccine currently exists for herpangina. Prevention hinges on interrupting viral transmission:
- Thorough handwashing: Soap and water, especially after bathroom use, diaper changes, before eating, and after caring for sick children
- Hygiene in communal settings: Disinfect toys, eating areas, and frequently touched surfaces
- Avoid sharing utensils, cups, towels with someone who is ill
- Keep symptomatic children at home until fever and mouth sores resolve
- Teach children to cover mouths and noses when coughing or sneezing and to dispose of tissues properly
Frequently Asked Questions (FAQs)
Q: Can adults get herpangina?
A: Yes, while most cases occur in children, adults can contract herpangina, though the illness is often milder and may go unnoticed in healthy adults.
Q: How long is herpangina contagious?
A: Herpangina is most contagious during the first week of illness, but viral shedding in stool can continue for several weeks after symptoms resolve.
Q: How can I tell the difference between herpangina and hand, foot, and mouth disease?
A: Both are caused by related viruses and present with mouth sores, but hand, foot, and mouth disease also causes a rash or lesions on the palms, soles, and buttocks, which herpangina does not.
Q: Should my child see a doctor for herpangina?
A: Most cases can be managed at home, but you should consult a healthcare provider if your child shows signs of dehydration, is very young, has certain health conditions, or if you have concerns about severe symptoms.
Q: Is recurrence possible?
A: Yes, but it is uncommon. Immunity develops to the specific viral strain, but other strains can still cause infection in the future.
Conclusion
Herpangina is an uncomfortable but usually benign viral illness in children, caused mainly by coxsackievirus. With supportive care focused on relieving symptoms and preventing dehydration, most children recover within a week. Practicing good hygiene and keeping sick children at home remain the most effective preventive measures. If you notice any warning signs or complications, seek medical advice promptly to ensure a full and rapid recovery.
References
- https://ada.com/conditions/herpangina/
- https://www.mountsinai.org/health-library/diseases-conditions/herpangina
- https://www.ncbi.nlm.nih.gov/books/NBK507792/
- https://www.coxhealth.com/condition/herpangina-in-children/
- https://www.northwestfamilyclinics.com/blog/understanding-hand-foot-and-mouth-disease-and-herpangina
- https://my.clevelandclinic.org/health/diseases/22508-herpangina
- https://www.childrenshospital.org/conditions/herpangina
- https://www.stlouischildrens.org/conditions-treatments/herpangina
- https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=uh3752
Read full bio of medha deb












