How to Repair Leaky Gut Syndrome: A Comprehensive 5-Step Protocol for Restoring Digestive Health
Strengthen the intestinal barrier to support digestion and boost well-being.
How to Repair Leaky Gut Syndrome: A 5-Step Protocol
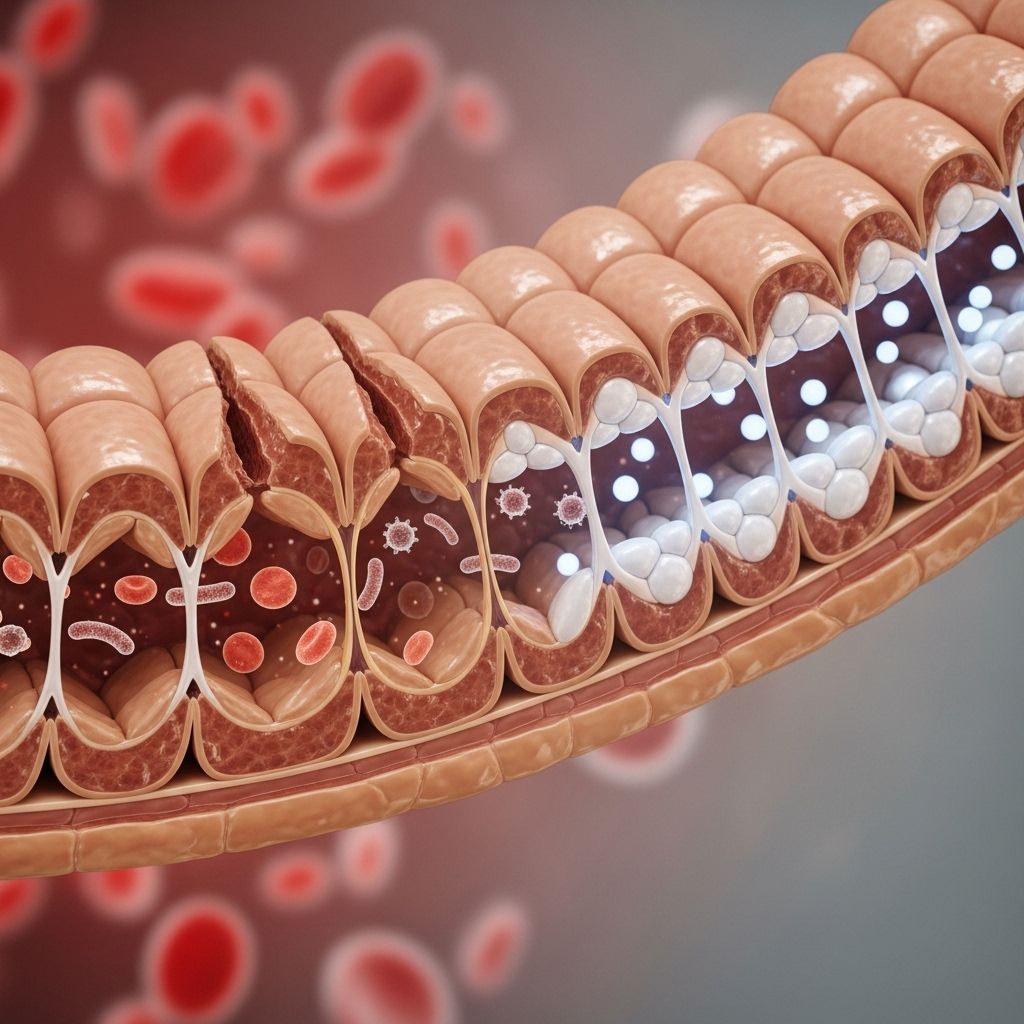
Leaky gut syndrome—also known as increased intestinal permeability—is a condition in which the lining of the digestive tract becomes damaged, allowing toxins, microbes, and partially digested food particles to pass through and enter the bloodstream. This can trigger systemic inflammation, immune system activation, and a broad range of symptoms from digestive discomfort to skin issues, fatigue, and even autoimmune conditions.
Fortunately, a science-supported, stepwise strategy—widely known as the 5-R Protocol—is frequently recommended by integrative and functional medicine practitioners to address and repair leaky gut. This article explores the protocol, essential evidence, best practices, and tips for long-term gut health.
Table of Contents
- What is Leaky Gut Syndrome?
- Signs and Symptoms of Leaky Gut
- The 5-Step Protocol to Repair Leaky Gut
- Step 1: Remove Irritants and Triggers
- Step 2: Replace Digestive Support
- Step 3: Reinoculate Gut Flora
- Step 4: Repair the Gut Lining
- Step 5: Rebalance Lifestyle and Long-Term Health
- Frequently Asked Questions
What is Leaky Gut Syndrome?
The intestinal lining is designed to allow the absorption of nutrients while providing a barrier against toxins and harmful microbes. In leaky gut syndrome, this barrier becomes compromised, letting substances into the bloodstream that would normally be contained within the gut. This phenomenon is associated with chronic inflammation, immune activation, and a wide range of symptoms and diseases including food sensitivities, irritable bowel syndrome, skin disorders, joint pain, and even mood disturbances.
Signs and Symptoms of Leaky Gut
- Chronic digestive discomfort (bloating, gas, diarrhea, or constipation)
- Food sensitivities or allergies
- Unexplained fatigue or brain fog
- Joint or muscle pain
- Skin problems (eczema, acne, rashes)
- Mood changes, anxiety, or depression
- Autoimmune conditions
- Chronic headaches or migraines
While these symptoms are nonspecific, persistent presence—especially with digestive complaints—should lead to a comprehensive evaluation by a healthcare provider.
The 5-Step Protocol to Repair Leaky Gut
The most recommended, evidence-based approach to repairing leaky gut is the 5-R protocol. The five steps are:
- Remove
- Replace
- Reinoculate
- Repair
- Rebalance
Each step addresses a key source of gut dysfunction and lays the foundation for optimal intestinal barrier health.
Step 1: Remove Irritants and Triggers
The first stage focuses on identifying and eliminating factors that contribute to gut inflammation, damage, or microbial imbalance:
- Dietary triggers: Eliminate foods most likely to cause irritation, sensitivity, or inflammation. These typically include gluten (wheat), dairy, processed grains, refined sugars, food additives, artificial sweeteners, alcohol, and caffeine.
- Allergens and sensitivities: Conduct an elimination diet to identify personal food triggers, such as eggs, soy, corn, nuts, nightshades (e.g., tomatoes, peppers), and shellfish.
- Medications and supplements: Minimize use of gut-irritating drugs such as NSAIDs (ibuprofen, naproxen), antibiotics, acid-suppressing medications (proton pump inhibitors, H2 blockers), and corticosteroids, under physician guidance.
- Environmental toxins: Reduce exposure to food-borne chemicals (preservatives, pesticides), smoking, recreational drugs, and unnecessary pharmaceuticals.
- Infections: Identify and treat underlying gut infections (bacterial overgrowth, parasites, yeast).
- Stress: Manage psychological stress, which significantly impacts digestive function and barrier integrity.
Tip: Consider working with a registered dietitian, nutritionist, or functional medicine practitioner to customize your elimination plan and safely address medications or chronic conditions.
Step 2: Replace Digestive Support
Chronic inflammation and poor digestion can reduce stomach acid, bile, and digestive enzymes, leading to malabsorption and further tissue damage. The replace phase focuses on optimizing digestion and nutrient absorption:
- Digestive enzymes: Supplement with comprehensive digestive enzyme blends, which may include amylase, protease, lipase, lactase, bromelain, and ox bile, as guided by a healthcare professional.
- Stomach acid: Betain HCl supplements may be used in cases of low stomach acid, improving protein digestion and reducing infection risk.
- Bile acids: Ox bile or other bile acid supplements may assist in fat digestion for those with removed gallbladders or impaired bile flow.
- Micronutrients: Supplement with a high-quality multivitamin and mineral formula to address nutritional deficiencies (e.g., vitamins A, D, E, C, B-complex, zinc, magnesium) common with impaired gut function.
Note: Always consult a qualified healthcare provider before initiating enzyme or acid supplements, as underlying gastrointestinal conditions should first be ruled out.
Step 3: Reinoculate Gut Flora
Restoring and diversifying the beneficial bacteria in the gut microbiome is essential for healthy digestion, nutrient assimilation, and immune regulation:
- Probiotics: Supplement with a multi-strain probiotic featuring Lactobacillus, Bifidobacterium, and/or Saccharomyces boulardii. High-dose, clinically tested formulas, preferably with at least 5–15 billion CFUs per day, are often recommended.
- Fermented foods: Incorporate yogurt (with live cultures), kefir, kimchi, sauerkraut, miso, tempeh, pickles (in brine), and kombucha.
- Prebiotics: Feed the beneficial bacteria with prebiotic-rich foods like bananas, artichokes, onions, garlic, leeks, chicory, barley, flaxseed, and oats. Some supplement with prebiotic fibers like fructooligosaccharides (FOS) or inulin.
- Diversity: Consume a wide range of fiber-rich, plant-based foods to support a diverse and resilient microbiome.
Research shows that a balanced microbiome supports mucosal repair and reduces harmful inflammation in the gut lining.
Step 4: Repair the Gut Lining
To address existing damage, focus on foods and nutrients that help heal and regenerate the intestinal mucosa:
- Glutamine: This amino acid is the preferred fuel for gut cells and is shown to promote healing of the intestinal barrier.
- Collagen and bone broth: Rich in amino acids (glycine, proline), collagen and slow-cooked bone broth support tissue repair and reduce inflammation.
- Soothing botanicals: Slippery elm, marshmallow root, licorice root (DGL), and aloe vera can protect and soothe the mucosa.
- Antioxidants: Increase intake of vitamins C, A, E, and polyphenols (found in berries, leafy greens, nuts) to counter oxidative stress and enhance tissue healing.
- Zinc: This mineral is critical for cellular repair and immune regulation; deficiencies are common in chronic intestinal disorders.
- Omega-3 fatty acids: Fish oil and flaxseed provide anti-inflammatory effects that promote mucosal repair and cell membrane health.
- Fiber: Soluble fibers and resistant starches support mucous production and feed beneficial bacteria.
Practical tips: Prioritize diverse, whole-food, anti-inflammatory eating. Avoid ultra-processed foods and consider strategic supplementation when advised by a healthcare professional.
Step 5: Rebalance Lifestyle and Long-Term Health
Lasting results require changes that continue to support gut and overall health well into the future:
- Manage stress: Chronic psychological stress can worsen barrier dysfunction and lower immune resilience. Mindfulness, meditation, breathwork, exercise, and quality social connections are highly beneficial.
- Sleep: Aim for 7–9 hours of restorative sleep nightly, as poor sleep directly impairs gut health and immune balance.
- Physical activity: Regular moderate movement supports bowel motility, healthy microbiome composition, and systemic anti-inflammation.
- Healthy relationships: Social support and positive relationships have demonstrated benefits for immune and gut function.
- Avoid harmful habits: Minimize alcohol, quit smoking, and avoid unnecessary antibiotics or gut-damaging drugs unless medically required.
Long-term healing is rarely instantaneous; consistent application of these lifestyle factors is essential for lasting improvement.
Sample Foods and Supplements for Each Protocol Step
| Step | Foods | Supplements |
|---|---|---|
| Remove | Eliminate processed foods, gluten, dairy, alcohol, refined sugars | N/A |
| Replace | Papaya, pineapple (natural enzymes), leafy greens (micronutrients) | Digestive enzymes, betaine HCl, multivitamin, bile salts |
| Reinoculate | Yogurt, kefir, kimchi, sauerkraut, pickles, bananas, onions, garlic | Multi-strain probiotics, prebiotic fiber supplements (FOS, inulin) |
| Repair | Bone broth, berries, leafy greens, salmon, oranges | Glutamine powder, collagen, aloe vera, slippery elm, zinc, omega-3 oil |
| Rebalance | Varied whole foods, minimal sugar, adequate water | Adaptogens (for stress), sleep support (as needed) |
Frequently Asked Questions (FAQs)
Q: How long does it take to heal leaky gut?
Depending on individual factors (cause, severity, consistency with the protocol), healing can take from several weeks to several months. Some people notice improvements within days, while others with longstanding or complex cases may require longer.
Q: Is there a test for leaky gut?
While there are specialized tests (e.g., the lactulose-mannitol urine test) to assess intestinal permeability, these are not commonly used in routine clinical practice. Diagnosis is typically based on history, symptom patterns, and response to a gut-healing protocol.
Q: Are all probiotics the same for gut healing?
No. It is generally best to use high-quality, multi-strain probiotics containing well-studied species such as Lactobacillus, Bifidobacterium, and Saccharomyces boulardii. Individual requirements may vary depending on your health condition and tolerance.
Q: Can children have leaky gut syndrome?
Yes, children can experience increased intestinal permeability. Symptoms commonly overlap with food allergies, eczema, digestive issues, behavioral changes, and more. Always work closely with a pediatrician for appropriate diagnosis and management.
Q: What professional support should I seek?
Consult a healthcare provider (integrative or functional medicine, gastroenterologist, or dietitian) for expert guidance on creating and monitoring your protocol. Professional oversight ensures a safe, effective, and personalized approach—especially if you have chronic illnesses, take medication, or have complex dietary needs.
Key Takeaways for Gut Health
- Follow the full 5-R protocol for best results—don’t skip or rush steps.
- Focus on personalized strategies tailored to your triggers, deficiencies, and needs.
- Consistency and patience are vital for healing the gut lining and restoring resilience.
- Diverse, minimally processed whole foods promote long-term gut and immune health.
- Address stress and lifestyle factors as they are equally crucial as dietary change.
References
- https://www.fammed.wisc.edu/files/webfm-uploads/documents/outreach/im/handout_therapy_increased_intestinal_permeability_clinician.pdf
- https://allianceortho.com/gut-protocol-5-steps-to-enhance-your-digestive-health/
- https://experiencelife.lifetime.life/article/5-steps-to-heal-a-leaky-gut/
- https://www.rupahealth.com/post/a-functional-medicine-protocol-for-leaky-gut-syndrome
- https://maxwellclinic.com/the-5-rs-to-healing-leaky-gut/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9862683/
- https://www.healthline.com/nutrition/leaky-gut-diet
- https://jacquibryan.com/healing-your-gut-a-lifestyle-guide-to-leaky-gut-protocol/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9028931/
Read full bio of medha deb












