Histamine & Skin Blood Flow: Mechanisms of Allergic Reaction Disruption and Therapeutic Implications
Vascular shifts during allergic flare-ups reveal new paths for symptom relief.
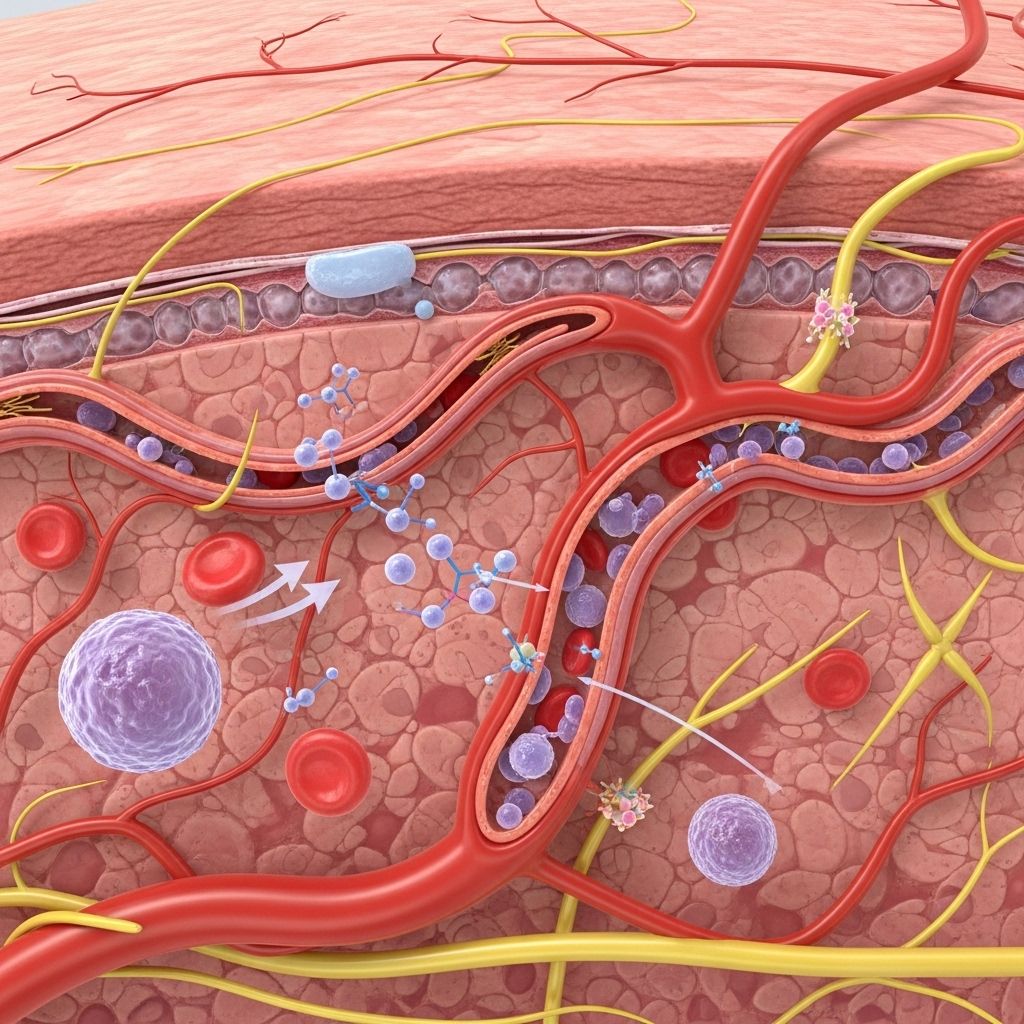
Histamine, a biogenic amine released predominantly from mast cells, is a critical mediator of allergic inflammation and skin blood flow alterations. The body’s finely tuned vascular responses to histamine play a dual role in physiological regulation and the manifestation of allergic diseases, making the interplay between histamine, skin blood flow, and vascular barrier function a central topic in allergy and immunology research. This article provides a comprehensive review of the cellular and molecular mechanisms by which histamine disrupts skin blood flow during allergic reactions, the consequences for vascular permeability, and contemporary insights into potential therapeutic interventions.
Table of Contents
- Introduction to Histamine and Skin Blood Flow
- Histamine Release During Allergic Reactions
- Histamine Receptors: H1 and H2 in Skin Vasculature
- Cellular Mechanisms of Vascular Hyperpermeability
- Role of Nitric Oxide in Histamine-Induced Vasodilation
- Endothelial Barrier Disruption
- Hemodynamic Changes: Blood Flow and Pressure
- Physiological Consequences: Urticaria, Edema, and More
- Impact of Skin Temperature on Histamine Response
- Therapeutic Implications: Antihistamines and Vasoconstrictors
- Frequently Asked Questions (FAQs)
- References
Introduction to Histamine and Skin Blood Flow
Histamine is a ubiquitous chemical messenger involved in various physiological and pathological processes. Upon release, especially during immune responses and allergic reactions, histamine profoundly influences vascular dynamics in the skin:
- Vasodilation: Expansion of blood vessels, leading to increased blood flow.
- Vascular permeability: Enhanced passage of fluids and immune cells through vessel walls.
- Tissue swelling: Manifestation of symptoms like redness, warmth, and edema.
This robust vascular response underlies many allergic skin symptoms, including urticaria (hives), angioedema, and local flare reactions.
Histamine Release During Allergic Reactions
The process of histamine release is tightly regulated and is central to the allergic cascade:
- Allergens (like pollen or food proteins) trigger immunoglobulin E (IgE)-mediated activation of mast cells.
- Mast cells degranulate, releasing preformed histamine into the local tissue environment.
- Rapid diffusion of histamine allows it to act on nearby vascular endothelial cells and smooth muscle.
In the skin, this immediate hypersensitivity reaction produces the classic “wheal and flare” response, characterized by localized swelling, redness, and itching.
Histamine Receptors: H1 and H2 in Skin Vasculature
Histamine mediates its vascular effects through specific cell surface receptors, prominently H1 and H2 receptors located on endothelial and smooth muscle cells in the skin:
| Receptor Type | Location | Mediated Effect | Clinical significance |
|---|---|---|---|
| H1 | Endothelial cells, smooth muscle, nerves | Vasodilation (via NO), increased permeability, pruritus | Primary target of most antihistamines |
| H2 | Vascular smooth muscle, gastric parietal cells | Vasodilation (direct smooth muscle relaxation), gastric acid secretion | Potentiates vascular response, target for certain antihistamines |
- H1-receptor activation is especially important in mediating nitric oxide (NO) release and subsequent vasodilation in the skin.
- H2-receptor activation causes direct relaxation of vascular smooth muscle and contributes to sustained vasodilation.
The synergistic action of these receptors is crucial for the full expression of histamine-induced blood flow changes during allergic reactions.
Cellular Mechanisms of Vascular Hyperpermeability
Histamine-induced vascular hyperpermeability underlies the characteristic tissue swelling seen in allergic skin reactions. Key cellular and molecular mechanisms include:
- Disruption of endothelial junctions: Histamine alters the localization and phosphorylation status of VE-cadherin, a critical protein at endothelial adherens junctions, weakening the vascular barrier.
- Increased intracellular calcium: Histamine increases intracellular Ca2+, leading to cytoskeletal changes and transient barrier opening.
- Signal pathway activation: Protein kinase C (PKC), Rho-associated kinase (ROCK), and nitric oxide synthase (NOS) play supportive roles in disrupting the endothelial barrier.
These mechanisms jointly promote the leakage of plasma proteins and immune mediators into surrounding tissues.
Role of Nitric Oxide in Histamine-Induced Vasodilation
Nitric oxide (NO) is a major mediator of vascular smooth muscle relaxation and plays a central role in histamine-induced vasodilation:
- Upon H1-receptor stimulation, endothelial cells release NO.
- NO diffuses to smooth muscle, activating guanylate cyclase and increasing cGMP, resulting in muscle relaxation and vessel dilation.
- This vasodilation raises local skin blood flow, heightening tissue permeability and fluid movement across vessel walls.
- Inhibitors of NOS (nitric oxide synthase) such as L-NAME markedly reduce histamine-induced vasodilation and hyperpermeability.
Therefore, the NO pathway is pivotal in both the acute and sustained vascular responses to histamine in the skin.
Endothelial Barrier Disruption
As histamine increases blood flow, it concurrently undermines the integrity of the endothelial barrier. This process involves:
- VE-cadherin phosphorylation and internalization: Weakening of cell-cell junctions facilitates plasma leakage.
- Cytoskeletal rearrangement: Induced by calcium influx and kinase signaling, leading to increased junctional gaps.
- Protein kinase involvement: PKC and ROCK contribute to endothelial contraction and barrier failure.
Disruption of the endothelial barrier is not only driven by intracellular signals but is also influenced by mechanical forces arising from increased blood flow and pressure.
Hemodynamic Changes: Blood Flow and Pressure
Alongside barrier disruption, histamine alters local hemodynamics:
- Vasodilation (expansion of blood vessels) increases regional blood flow and intravascular hydrostatic pressure, exerting physical stress on vessel walls.
- Blood flow increase is largely NO-dependent and is essential for the manifestation of vascular hyperpermeability in vivo.
These changes contribute significantly to plasma extravasation, tissue swelling, and the visual skin findings seen during allergic reactions.
Physiological Consequences: Urticaria, Edema, and More
The orchestrated effects of histamine-induced vasodilation and endothelial leakage lead to tangible clinical manifestations:
- Urticaria (Hives): Raised, red, and itchy welts due to plasma leakage and dermal edema.
- Angioedema: Deeper swelling of subcutaneous and submucosal tissues, frequently mediated by histamine and other vasoactive substances.
- Flare and redness: Increased local blood flow produces warmth and erythema (redness).
These symptoms, though uncomfortable or alarming, reflect the body’s protective efforts to localize and manage perceived threats.
Impact of Skin Temperature on Histamine Response
Skin temperature drastically influences the vascular response to histamine:
- Cooled skin exhibits reduced histaminergic vasodilation, especially via the H1 receptor.
- Combined antagonism of H1 and H2 receptors reduces the vascular response at both normal and low temperatures, but H1-blockade alone is particularly effective at lower temperatures.
- These findings help explain conditions like cold urticaria, where exposure to cold alters vascular responses and triggers exaggerated allergic symptoms.
Temperature-dependent modulation of histamine sensitivity underscores the dynamic regulation of skin blood flow and vessel reactivity.
Therapeutic Implications: Antihistamines and Vasoconstrictors
Understanding the dual mechanisms of histamine—through blood flow increase and barrier disruption—guides allergy management strategies:
- H1-antihistamines (e.g., cetirizine) target the primary pathway of histamine-induced vasodilation and permeability, providing symptomatic relief for urticaria and other allergic manifestations.
- H2-antihistamines (e.g., cimetidine) provide additive effects and are sometimes used in conjunction with H1-antagonists for more severe or refractory symptoms.
- Vasoconstrictors are effective in allergic rhinitis and may benefit other histamine-mediated symptoms by negating NO-driven blood flow increases.
Combination therapies and tailored pharmacological interventions may provide enhanced relief for patients with complex or chronic allergic disorders.
Frequently Asked Questions (FAQs)
Q1: How does histamine cause the classic redness and swelling of allergic skin reactions?
A1: Histamine triggers vasodilation (expanding blood vessels) and increases vascular permeability, allowing plasma and immune cells to leak into the skin, leading to redness, warmth, and swelling.
Q2: What role do antihistamines play in managing skin allergies?
A2: Antihistamines, especially H1-receptor blockers, inhibit histamine-induced vasodilation and leakage, reducing swelling, redness, and itchiness during allergic reactions.
Q3: Why do cold temperatures reduce allergic flare-ups in some people?
A3: Cold temperatures attenuate the sensitivity of histamine receptors (notably H1), reducing vasodilation and the resulting vascular effects, which can provide temporary relief in conditions like urticaria.
Q4: Are there different types of histamine receptors in the skin, and do they all play a role in allergies?
A4: The primary receptors involved in allergic skin reactions are H1 and H2; both contribute to vasodilation, but H1 also mediates permeability and itching. Targeting both may offer broader symptom control.
Q5: Can other substances besides histamine increase skin blood flow during allergic reactions?
A5: Yes, other mediators such as prostaglandins and bradykinin also affect skin blood flow and permeability, often working in concert with histamine during inflammation and allergy.
References
- Histamine Induces Vascular Hyperpermeability by Increasing Blood Flow and Disrupting Endothelial Barrier Formation
- Histamine response and local cooling in the human skin
References
Read full bio of medha deb












