Gut-Skin-Lung Axis: The Interconnected Barrier System Regulating Immunity and Health
Microbial crosstalk between your body's key defenses shapes overall immune resilience.
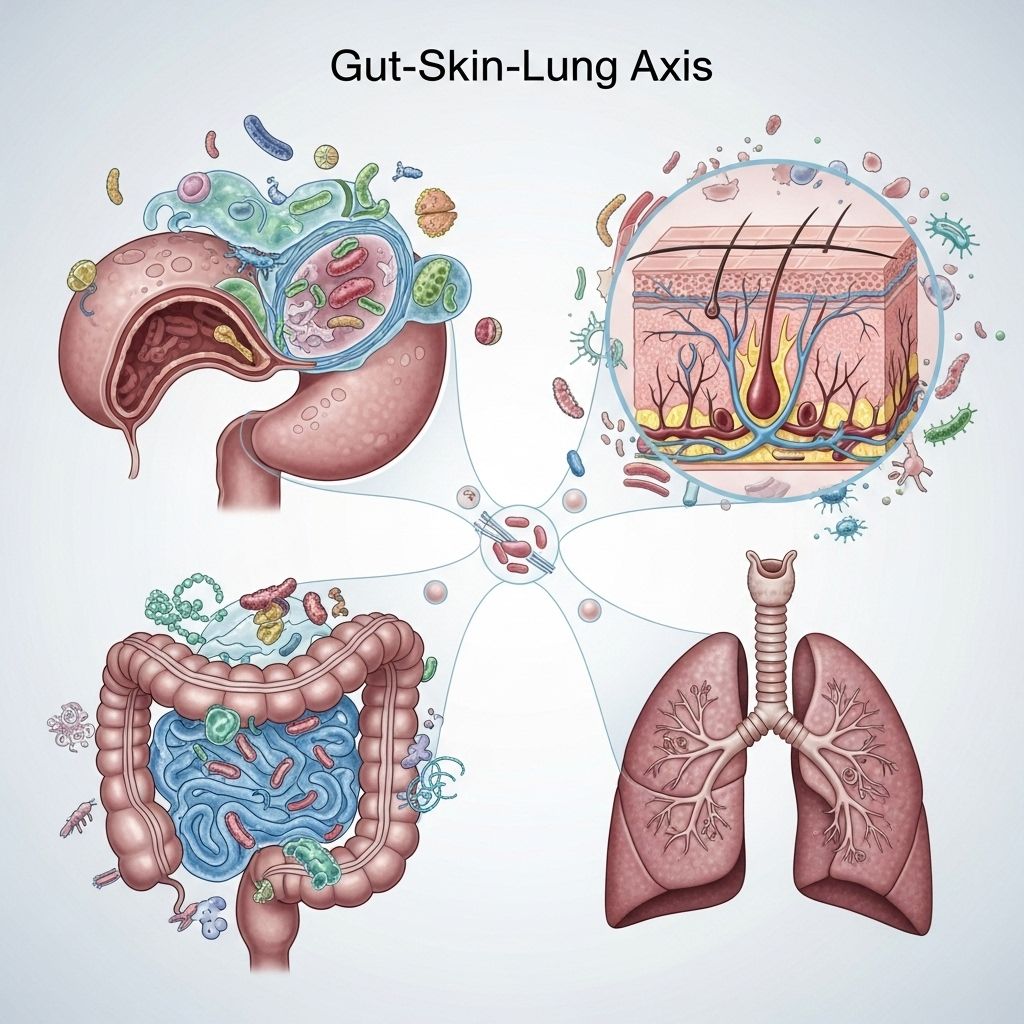
The emerging paradigm of the gut-skin-lung axis has shifted our understanding of human health. Traditionally viewed as three separate organ systems, new research illuminates their profound interconnection. The epithelial barriers—of the gut, skin, and lungs—communicate through immune, microbial, and metabolic pathways, forming a dynamic axis vital for immune homeostasis, inflammation control, and disease development.
Table of Contents
- Introduction
- Anatomy and Function of Gut, Skin, and Lung Barriers
- The Microbiome: Keystone of Barrier Crosstalk
- Immunological Pathways Linking Gut, Skin, and Lungs
- Gut-Skin and Gut-Lung Axes in Health
- Disruption of the Axis: Pathogenesis and Disease Examples
- Environmental Triggers and Modulators
- Therapeutic Implications and Intervention Strategies
- Challenges and Future Opportunities
- Frequently Asked Questions (FAQs)
Introduction
Humans rely on a trio of critical defense barriers—gut, skin, and lung—to maintain internal balance and protect against pathogens and toxins. Increasingly, research reveals that these barriers are not isolated; instead, they engage in intensive two-way communication, coordinated by microbiota, immune signaling, and environmental factors, forming the so-called “gut-skin-lung axis”.
Dysfunction in one barrier can manifest as disorders in another, highlighting the clinical importance of integrated barrier health. Examples include gastrointestinal diseases influencing skin conditions, gut microbiota affecting respiratory allergies, and systemic inflammation bridging the three organs. The axis offers novel avenues for disease prevention and treatment as well as personalized medicine.
Anatomy and Function of Gut, Skin, and Lung Barriers
Gut Barrier
The gastrointestinal (GI) tract is lined with a single layer of epithelial cells, reinforced by goblet-cell-synthesized mucus and antimicrobial molecules, forming a highly selective interface. Key features:
- Tight junction proteins—such as zonula occludens and claudins—regulate permeability and segregate harmful luminal contents from the body.
- Secretory immune components—like secretory IgA—neutralize pathogens before epithelial invasion.
- Mucosal immunity, with dendritic cells sampling antigens and priming immune responses.
Skin Barrier
The skin consists of three main layers: epidermis, dermis, and hypodermis. The outermost epidermis, with its corneocyte shield and appendageal structures (e.g., sweat glands, hair follicles), serves as a physical and immunological barrier. Key attributes include:
- Lipid-rich stratum corneum provides impermeability to many pathogens.
- Resident immune cells (Langerhans, dermal dendritic cells) detect and respond to microbial signals.
- Highly specialized skin microbiota modulate inflammation and participate in wound healing.
Lung Barrier
The respiratory tract is protected by a specialized epithelial lining and mucus layer, providing both physical defense and immunological readiness. Core features:
- Mucociliary escalator clears particles and microbes upward for expulsion.
- Alveolar macrophages serve as sentinel immune cells.
- Lung microbiota interact with host immune mechanisms and systemic metabolites from the gut or skin.
The Microbiome: Keystone of Barrier Crosstalk
Each barrier houses distinct, yet interconnected, microbial communities:
- Gut microbiota—the densest, dominated by Firmicutes, Bacteroidetes, Actinobacteria, and Proteobacteria.
- Skin microbiota—varies by body site, mainly Staphylococcus, Corynebacterium, Cutibacterium, and others.
- Lung microbiota—less dense, but increasingly recognized as crucial for pulmonary immunity and resilience.
Microbial metabolites, such as short-chain fatty acids (SCFAs), vitamin derivatives, and tryptophan catabolites, travel between organs, modulating barrier strength, immune responses, and systemic inflammation.
Immunological Pathways Linking Gut, Skin, and Lungs
Communication across these barriers relies upon intricate immune signaling:
- Cytokine migration: Cells in one barrier release signaling molecules like IL-22, IL-17, and IL-33, which influence distant sites.
- Immune cell trafficking: Lymphoid cells (e.g., innate lymphoid cells ILC2 and ILC3) are “trained” in the gut and migrate to the lungs (and potentially the skin), affecting allergy and infection responses.
- Pattern recognition receptors: Microbial products (e.g., peptidoglycans, LPS) sensed by toll-like receptors trigger systemic immune cascades.
For example, an increase in Proteobacteria in the gut triggers IL-33 production, mobilizing ILC2s to the lungs and regulating airway inflammation.
Gut-Skin and Gut-Lung Axes in Health
Gut-Skin Axis in Health
- Balanced gut and skin microbiota support tissue homeostasis and robust local immunity.
- Microbial neurotransmitters and metabolites influence skin hydration, elasticity, and host defense mechanisms.
- Nutritional inputs, such as fiber, stimulate beneficial bacteria to produce anti-inflammatory SCFAs impacting both gut and skin barrier function.
Gut-Lung Axis in Health
- Common embryonic and structural origins between gut and lung epithelium permit shared immunological strategies.
- SCFAs produced by gut microbiota circulate to the lungs, reducing pro-inflammatory signals and fortifying lung barrier integrity.
- Balanced gut microbiota dampens development of allergic airways responses, contributing to asthma prevention.
Disruption of the Axis: Pathogenesis and Disease Examples
| Axis Disrupted | Trigger/Event | Resulting Disease |
|---|---|---|
| Gut-Skin Axis | Dysbiosis, increased gut permeability (“leaky gut”) | Atopic dermatitis, psoriasis, acne flares |
| Gut-Lung Axis | Reduced SCFA, disruption of microbiota | Asthma, chronic obstructive pulmonary disease (COPD), allergic airway inflammation |
| Combined Barrier Dysfunction | Systemic inflammation, barrier leakage, viral or bacterial infection | Multi-organ inflammation, increased risk of sepsis and autoimmune disorders |
Mechanisms of disruption:
- Microbiota dysbiosis—shifts in dominant bacteria, loss of diversity.
- Barrier permeability—damage to tight junctions, leading to “leakiness” and translocation of toxins or pathogens.
- Immune imbalance—inappropriate activation or suppression, promoting chronic inflammation.
Environmental Triggers and Modulators
Many exogenous and lifestyle factors modulate the axis:
- Diet: High-fat, low-fiber diets encourage dysbiosis and reduce SCFAs.
- Antibiotics: Disrupt all three microbial communities, often with long-term impacts.
- UV Exposure: Ultraviolet B-light to the skin can beneficially alter both local and gut microbiota, with downstream health effects.
- Pollutants: Airborne toxins harm the lung microbiome, but can also prime gut and skin inflammation through systemic effects.
- Infections: Viral or bacterial invasions at one barrier can amplify immune responses at other sites.
Therapeutic Implications and Intervention Strategies
Microbiome Modulation
- Probiotics and Prebiotics: Supplementing specific beneficial bacteria or feeding endogenous strains can restore microbiome balance in the gut, with downstream skin and lung benefits.
- Dietary Fiber: Enhances SCFA production which reduces systemic inflammation and fortifies distant barriers.
Targeted Therapies
- Topical and oral agents: Medications that restore epithelial tight junctions and support barrier integrity (e.g., ceramide creams for skin; butyrate for gut).
- Fecal Microbiota Transplantation: Investigational for severe dysbiosis affecting all axis organs.
- Phototherapy: Medical use of UVB light to the skin to trigger beneficial systemic immune and microbial changes.
Emerging Strategies
- Immunomodulator drugs targeting cytokine pathways shared by the barriers.
- Personalized medicine based on individual microbiome signatures and environmental exposures.
Challenges and Future Opportunities
- Deciphering the full network of communication between the gut, skin, and lungs, given individual variability.
- Identifying biomarkers for early detection of axis disruption.
- Developing safe, effective interventions that address all system components rather than isolated symptoms.
- Leveraging advances in multi-omics and machine learning to map complex microbial and immune interplay.
Frequently Asked Questions (FAQs)
Q: What exactly is the gut-skin-lung axis?
A: It is the integrated communication and functional connection among the gut, skin, and lung barriers, largely orchestrated by the microbiome and immune system, influencing systemic health and disease risk.
Q: How does my diet affect all three barriers?
A: A balanced, fiber-rich diet supports a healthy gut microbiome; its metabolites circulate systemically, strengthening skin and lung barriers and tuning immune responses.
Q: Can treating one organ improve conditions in another?
A: Research shows that improving gut health with probiotics or prebiotics can benefit skin and lung conditions, particularly those with an inflammatory or allergic component.
Q: What are signs my barrier system is disrupted?
A: Symptoms may include frequent GI upsets, persistent skin irritation or rashes, and respiratory issues such as allergies or asthma.
Q: Are antibiotics harmful to this axis?
A: Broad-spectrum antibiotics disrupt the microbial communities in the gut, skin, and lungs, often leading to increased vulnerability to infection, allergies, or inflammation. Judicious use is essential.
Key takeaway: The gut-skin-lung axis is a frontier in medicine, emphasizing holistic, cross-organ approaches to maintaining health and preventing disease through barrier integrity and microbial harmony.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11901370/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10508358/
- https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1346923/full
- https://www.biocodexmicrobiotainstitute.com/en/pro/gut-lung-axis-viral-respiratory-infections
- https://www.danoneresearch.com/nutrition-for-all-needs/gut-health/gut-organ-axis/
Read full bio of medha deb












