Gut Microbiome & Peripheral Skin Circulation Link: Understanding the Gut-Skin Axis and Vascular Health
Intestinal flora tune tiny vessels to boost tissue vitality and a healthy glow.
The intricate interplay between the trillions of microbes in our gut and the health of our skin is one of the most fascinating frontiers in modern biomedicine. Recent research has revealed that the gut microbiome not only influences skin appearance and disease but may also play a critical role in regulating peripheral skin circulation. This expansive review explores the core science, mechanisms, and therapeutic implications linking the gut, skin, and vascular systems.
Table of Contents
- Introduction: The Gut-Skin-Vascular Paradigm
- Defining the Gut-Skin Axis
- Core Mechanisms: Immune, Metabolic, and Vascular Pathways
- Microbial Metabolites: The Messengers of the Axis
- Peripheral Skin Circulation—Why It Matters
- Clinical and Experimental Evidence Linking Gut Microbiome and Skin Perfusion
- Dysbiosis, Disease, and Circulatory Consequences
- Therapeutic Strategies and Future Directions
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction: The Gut-Skin-Vascular Paradigm
The human gut microbiome comprises a diverse ecosystem of bacteria, fungi, viruses, and other microorganisms residing mainly in the lower gastrointestinal tract. These microbes play crucial roles in digestion, immune system education, and synthesis of key nutrients and signaling molecules. The health of our peripheral skin—including its appearance, wound healing capacity, and circulation—is now known to be deeply linked to the health and composition of our gut microbiota.
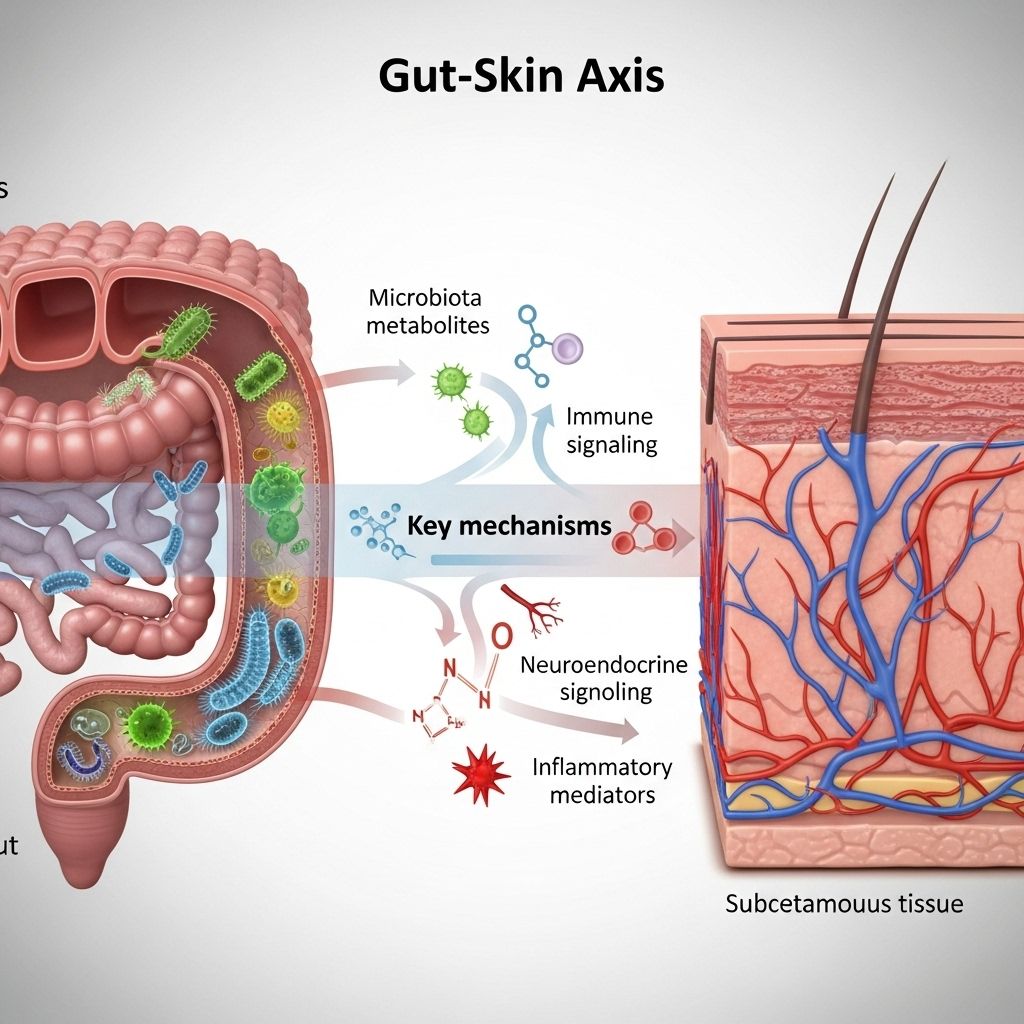
The concept of a gut-skin axis describes the complex, bidirectional communication between the digestive tract and the skin, mediated through immune cells, metabolites, hormonal signals, and the vascular system. Emerging research suggests that disruptions in the gut microbiome can impact not only skin pathology but also microvascular tone and perfusion, potentially affecting a wide range of skin functions.
Defining the Gut-Skin Axis
The gut-skin axis extends beyond simple dietary effects on skin. Rather, it describes the molecular, immune, metabolic, and neuroendocrine interactions connecting the gut environment and the skin’s health and function. Core elements include:
- Shared barrier functions: Both the gut and the skin serve as critical barriers against environmental insults and pathogens.
- Immune system cross-talk: Roughly 70–80% of the body’s immune cells are located within the gut-associated lymphoid tissue. These cells communicate with systemic and local skin immunity.
- Transported microbial metabolites: Short-chain fatty acids (SCFAs), neurotransmitters, and other compounds generated by gut microbes can circulate and influence skin cells and vessels.
Bidirectional Influence Between Gut and Skin
The relationship is reciprocal—skin disorders can reflect changes in gut health, while gut dysfunction can exacerbate skin issues. Inflammation and oxidative stress originating in one system can propagate to the other, perpetuating disease.
Core Mechanisms: Immune, Metabolic, and Vascular Pathways
The pathways connecting the gut microbiome and peripheral skin circulation involve several layers of connectivity, summarized below:
- Immune modulation: Gut microbes shape the development and function of innate and adaptive immune responses, affecting both local (gut) and systemic (including skin) immunity.
- Metabolic communication: Microbes ferment dietary fibers and proteins, generating SCFAs and other molecules that impact skin cell proliferation, differentiation, and barrier integrity.
- Endothelial signaling: Certain microbial metabolites directly or indirectly influence endothelial cell function, which controls blood flow to the skin.
- Neuroendocrine links: Gut microbes can synthesize or regulate neurotransmitters and hormone-like compounds, altering systemic stress responses and vascular tone.
Table: Pathways Linking Gut Microbiome, Immune Modulation, and Skin Circulation
| Pathway | Description | Examples of Key Molecules |
|---|---|---|
| Immune Modulation | Gut-derived immune cells and cytokines circulate, influencing skin inflammation and vessel tone | Regulatory T-cells, IL-10, TNF-α |
| Metabolic Products | Fermentation and metabolism of nutrients yield compounds affecting skin health and perfusion | SCFAs (butyrate, propionate, acetate), p-cresol, phenols |
| Neuroendocrine Signaling | Microbial generation of neurotransmitters impacts vascular responses | Serotonin, GABA, catecholamines |
| Barrier Integrity | Gut barrier function influences systemic toxin and metabolite levels that can disrupt skin and vessels | Tight junction proteins, lipopolysaccharides (LPS) |
Microbial Metabolites: The Messengers of the Axis
The human colon is a fermentation hub, producing a range of compounds that enter systemic circulation. The following metabolites are especially important for the gut-skin-vascular link:
- Short-Chain Fatty Acids (SCFAs): Molecules like butyrate, acetate, and propionate modulate skin immune responses, barrier function, and may influence vascular dilation/constriction within the skin. Propionate, notably, has antimicrobial effects on common skin pathogens.
- Phenolic and aromatic compounds: When present in excess, products such as p-cresol and free phenol can damage skin barrier integrity and impair keratinization, affecting hydration and function.
- Neurotransmitters and hormones: Gut microbes can create or modulate levels of serotonin, GABA, dopamine, and even cortisol, which influence inflammatory tone and vascular activity in the skin.
Peripheral Skin Circulation—Why It Matters
Peripheral skin circulation refers to the blood flow through the small vessels (arterioles, capillaries, venules) supplying the skin and subcutaneous tissues. Robust skin circulation is central to:
- Temperature regulation
- Delivery of oxygen and nutrients to skin tissue
- Efficient wound healing
- Removal of metabolic waste
- Maintaining a healthy, hydrated, and youthful skin appearance
Disruptions in skin circulation can exacerbate inflammatory skin disorders, delay wound healing, and contribute to dullness, dryness, and other cosmetic concerns.
Clinical and Experimental Evidence Linking Gut Microbiome and Skin Perfusion
Increasingly, both animal and human studies report that gut microbes and their metabolites can impact microvasculature throughout the body, including the skin. Central findings include:
- Gut dysbiosis is linked to impaired skin barrier and increased skin inflammation, often involving changes in skin blood flow. Inflammatory cytokines and harmful metabolites produced in the gut can access systemic circulation and disrupt cutaneous vascular dynamics.
- SCFAs maintain gut and skin barrier integrity, and may enhance endothelial function. Butyrate, in particular, has been shown to improve epithelial barriers and reduce systemic inflammation, potentially facilitating better skin microcirculation.
- Immune cell trafficking and T-cell regulation are directly influenced by the gut microbiome, with regulatory T-cells mediating inflammatory responses in both the intestine and peripheral skin vasculature.
- Clinical correlation between gut disease and skin manifestations: Patients with conditions like inflammatory bowel disease (IBD) often exhibit parallel skin disorders, which may involve microvascular changes.
Dysbiosis, Disease, and Circulatory Consequences
What Is Dysbiosis?
Dysbiosis is a disruption or imbalance in the composition and function of the gut microbiome. Common causes include antibiotic use, poor diet, chronic stress, infections, and certain medications. Dysbiosis is characterized by reduced beneficial bacteria, increased pathogenic species, and decreased microbial diversity.
Skin Effects of Dysbiosis
- Impaired skin barrier: Harmful metabolites from pathogenic bacteria can compromise keratinocyte function, reducing skin hydration and resilience.
- Systemic inflammation: Increased gut permeability (“leaky gut”) can lead to the passage of endotoxins and inflammatory triggers into the bloodstream, impacting skin vessels and immunity.
- Chronic skin conditions: Acne, atopic dermatitis, psoriasis, and certain vascular disorders of skin have been connected to abnormal gut microbial patterns.
Therapeutic Strategies and Future Directions
Understanding the gut-skin-circulation axis opens new avenues for targeted therapies aimed at restoring balance and optimizing skin health. Emerging strategies include:
- Dietary intervention: High-fiber, plant-based diets encourage beneficial bacteria that produce SCFAs and other protective metabolites, improving both gut and skin health.
- Prebiotics and probiotics: Supplementation can reshape gut microbial communities, attenuating inflammation, promoting immune balance, and supporting skin microcirculation.
- Synbiotics: Combination of prebiotics (fiber, inulin) and probiotics for synergistic gut and skin benefits.
- Targeted therapies: Emerging drugs, postbiotics, and topical/systemic interventions that modulate specific gut microbial pathways or their downstream mediators.
- Personalized medicine: Microbiome sequencing and metabolic profiling may eventually allow customized prevention and treatment plans based on an individual’s gut microbial signature.
Example Table: Strategies Impacting Gut Microbiome and Skin Circulation
| Strategy | Effect on Gut Microbiome | Potential Skin Effects |
|---|---|---|
| High-Fiber Diet | Promotes SCFA-producing bacteria | Enhances skin barrier, reduces inflammation, supports microcirculation |
| Probiotic Supplementation | Increases beneficial bacteria, suppresses pathogens | Improves skin inflammation, supports immune modulation |
| Synbiotics | Synergistically improves microbiome diversity | Prevents skin dryness, supports vascular health |
Frequently Asked Questions (FAQs)
Q: Can improving my gut health directly make my skin look better?
A: Yes. A balanced gut microbiome can reduce systemic inflammation, improve skin barrier integrity, and may enhance skin circulation, all contributing to healthier, more resilient skin.
Q: What foods support both gut and skin health?
A: Foods rich in dietary fiber (vegetables, fruits, legumes, whole grains), fermented foods (yogurt, kefir, kimchi), and foods high in polyphenols (berries, green tea) foster beneficial gut bacteria that support skin health and circulation.
Q: Are probiotics safe for everyone aiming to boost skin health?
A: Most probiotics are safe for healthy individuals but may pose risks in immunocompromised people. Always consult a healthcare professional for personalized advice, especially if you have underlying conditions.
Q: Can gut microbiome testing help with skin problems?
A: Microbiome analysis reports can provide insight into gut-skin links, though the field is still evolving. Your results may aid in personalizing diet and treatment strategies for skin and vascular issues.
Conclusion
The gut microbiome’s impact stretches far beyond the digestive tract, intricately influencing skin homeostasis and peripheral circulation. Interventions that restore microbial balance stand to benefit not only our complexion but the vascular systems that support robust skin health. Continued research will unlock individualized, microbiome-directed therapies for an array of skin and vascular conditions—heralding a new era in integrative dermatology and vascular medicine.
References
- https://www.owlstonemedical.com/about/blog/2024/oct/01/how-the-gut-microbiome-influences-skin-health-exploring-the-gut-skin-axis/
- https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.01459/full
- https://jsstd.org/?article=2167ac1cc231287a31a0c82c01188859wRYDGOT7L58%3D&embedded=true&view-pdf=1
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7916842/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6920876/
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1231848/full
- https://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0298443
Read full bio of medha deb












