Gut Health and Skin Conditions: Unraveling the Link Between the Gut Microbiome, Eczema, and Psoriasis
Healing the gut microbiome can unlock clearer, calmer skin from the inside out.
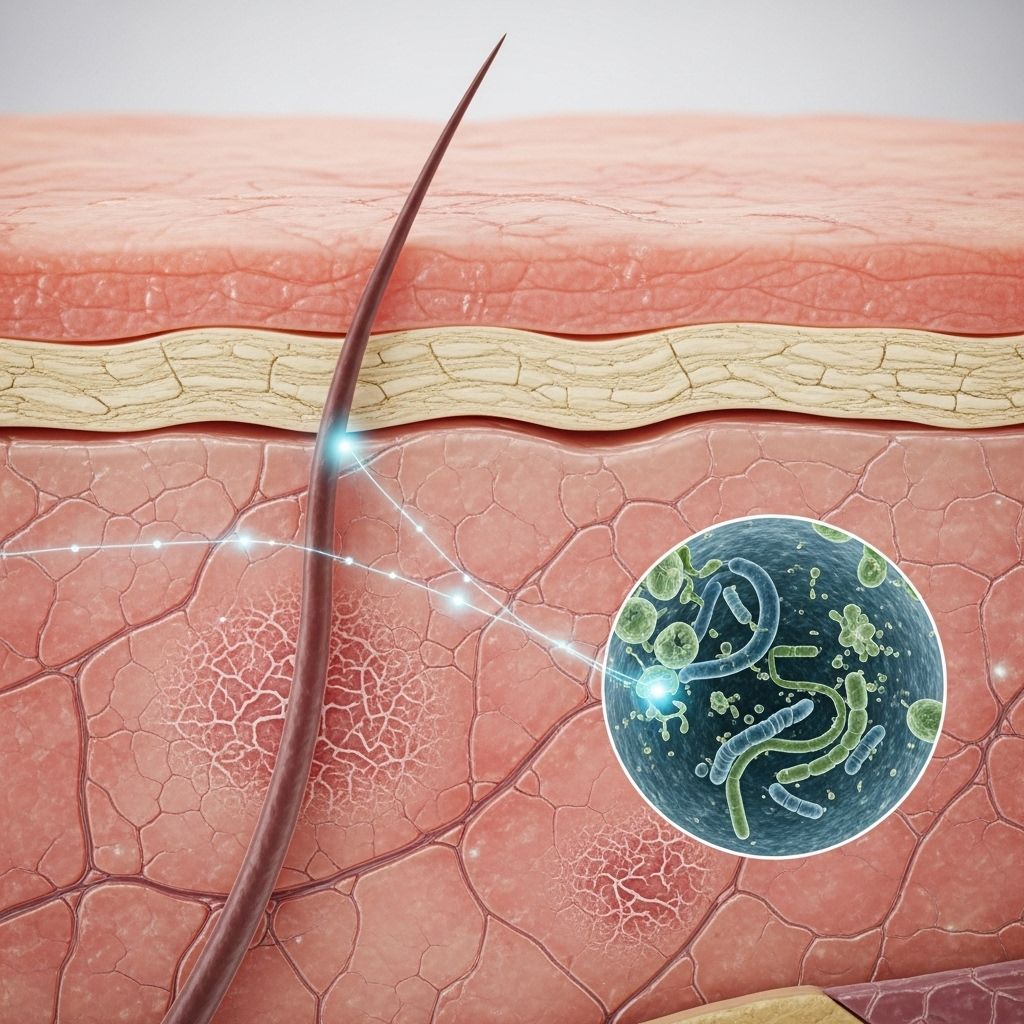
The intricate relationship between gut health and the skin has prompted a surge of research interest in recent years. Emerging evidence demonstrates that the gut microbiome—a diverse ecosystem of microorganisms in the digestive tract—communicates with the skin via what is known as the gut-skin axis. Imbalances in gut bacteria, called dysbiosis, have been linked to inflammatory skin conditions, including eczema (atopic dermatitis) and psoriasis. This article explores the science underpinning the gut-skin connection, the mechanisms at play, and the implications for treating skin disorders.
Table of Contents
- Introduction: The Gut-Skin Connection
- Understanding the Gut Microbiome
- The Gut-Skin Axis: How It Works
- Dysbiosis and Skin Dyshomeostasis
- Eczema and the Gut Microbiome
- Psoriasis and Gut Health
- Mechanisms of Gut Influence on Skin Health
- Diet and Lifestyle Factors
- Therapeutic Strategies for Gut-Skin Health
- Frequently Asked Questions (FAQs)
- Conclusion
Introduction: The Gut-Skin Connection
The skin and gut are the body’s largest organs of defense, both serving as barriers that protect against external threats. Fascinatingly, research over the past decade has revealed a dynamic, bidirectional communication pathway between gut health and skin health—termed the gut-skin axis. Gastrointestinal issues are often accompanied by skin problems, and inflammatory skin conditions frequently coincide with gut symptoms.
Studies have linked changes in gut microbial balance to skin conditions such as atopic dermatitis and psoriasis. Understanding the gut-skin axis opens new avenues for therapeutic interventions using diet, probiotics, and other microbiome-targeted modalities .
Understanding the Gut Microbiome
The gut microbiome refers to the trillions of bacteria, viruses, fungi, and other microorganisms living in the human digestive tract. In a healthy state, the microbiome forms an ecosystem characterized by high diversity and stability. Key functions include:
- Digesting complex carbohydrates
- Producing short-chain fatty acids (SCFAs), such as butyrate
- Regulating the immune system
- Protecting against pathogens
- Modulating gut barrier integrity
Disruptions—whether from antibiotics, diet, stress, or illness—can result in dysbiosis, tipping the scales toward inflammation. This state is increasingly recognized as a root cause of numerous systemic and inflammatory conditions, including those affecting the skin .
The Gut-Skin Axis: How It Works
The gut-skin axis describes the complex interplay between the gut microbiome and skin health. Signals generated by gut microbes—including metabolites like SCFAs, immune mediators, and microbial products—travel through the bloodstream to impact distant organs such as the skin.
Main routes of gut-skin communication include:
- Immune modulation: The gut microbiota helps regulate the balance between pro- and anti-inflammatory immune responses.
- Metabolic signaling: Byproducts such as SCFAs support the development of regulatory T cells, influencing skin immunity.
- Barrier integrity: Healthy gut flora maintain the gut lining, reducing systemic exposure to inflammatory molecules that can disrupt skin homeostasis.
Research demonstrates that when this axis is disrupted, as in dysbiosis, the outcome can be chronic inflammation and immune dysfunction—key drivers behind skin diseases like eczema and psoriasis .
Dysbiosis and Skin Dyshomeostasis
Dysbiosis—a disturbed or imbalanced gut microbiome—can have cascading effects on skin function. One mechanism involves the production of harmful metabolites (such as phenols and p-cresol) by certain pathogenic bacteria. These substances can enter the bloodstream, accumulate in the skin, impair the skin barrier, and trigger immune system responses .
Consequences of gut dysbiosis for the skin may include:
- Reduced skin hydration and altered keratinization
- Impaired skin barrier integrity
- Chronic, systemic inflammation due to leaky gut
- Enhanced susceptibility to skin infections and rashes
This state of skin dyshomeostasis is especially significant in inflammatory conditions, including eczema and psoriasis .
Eczema and the Gut Microbiome
Atopic dermatitis (eczema) is a chronic, inflammatory skin disorder marked by red, itchy skin and impaired barrier function. Recent advances highlight a tight link between gut microbial balance and the onset, persistence, and severity of eczema .
Key findings include:
- Children with eczema often display reduced diversity in their gut microbiome, particularly a lower abundance of beneficial bacteria.
- Certain gut-derived metabolites are found in higher concentrations in individuals with eczema, correlating with flares.
- Trials involving probiotics and prebiotics show potential for reducing eczema severity, although results are variable.
These results underscore the importance of gut microbial health in modulating immune responses that underlie eczema pathogenesis .
Psoriasis and Gut Health
Psoriasis is an autoimmune-driven skin disease featuring patches of thickened, scaly skin. A growing body of research points to a disrupted gut microbiome playing a central role in both the onset and perpetuation of psoriasis .
- Psoriasis patients frequently exhibit evidence of gut dysbiosis, including decreased bacterial diversity and alterations in specific microbial taxa.
- Lab studies reveal that these microbial changes can drive increased production of pro-inflammatory cytokines—such as TNF-α and IL-17—implicated in psoriasis pathology.
- Some patients experience improvement in skin symptoms following gut microbiome-targeted interventions (e.g., dietary modification, probiotics).
These features underline the importance of considering gut health as a potential therapeutic target for psoriasis .
Mechanisms of Gut Influence on Skin Health
The ways in which the gut microbiome affects the skin are multifaceted. Central mechanisms include:
| Mechanism | Effect on Skin | Example |
|---|---|---|
| Immune regulation | Balances inflammatory and anti-inflammatory signals | Enhances production of regulatory T cells, reducing skin inflammation |
| Barrier maintenance | Prevents translocation of bacterial products and endotoxins | Limits systemic inflammation that can trigger eczema or psoriasis |
| Metabolite production | Provides nutrients and immunomodulatory molecules | SCFAs (butyrate) support healthy skin barrier and immune tolerance |
| Neuroendocrine signaling | Modulates stress responses linked to skin conditions | Alters production of stress hormones impacting both gut and skin |
Diet and Lifestyle Factors
Diet is a powerful modifier of the gut microbiome. Diets rich in fiber and plant-based foods promote a healthy microbial balance, while excess sugar, processed foods, and saturated fats can diminish diversity and promote dysbiosis . Other lifestyle factors—such as sleep, stress, and medication use (e.g., antibiotics)—also play a role in shaping both gut and skin health.
- High-fiber, prebiotic-rich diets support the growth of beneficial gut bacteria and SCFA production.
- High-sugar or Western-style diets often correlate with increased skin inflammation and acne.
- Chronic stress disrupts both gut and skin barrier integrity through neuroendocrine pathways.
Food Allergies and the Gut-Skin Link
Food allergies are a concrete example of the gut-skin axis in action. Allergic reactions in the gut can result in skin symptoms such as hives or eczema, although the details of this link are still being explored .
Therapeutic Strategies for Gut-Skin Health
Given the evident influence of gut health on the skin, targeted interventions are being investigated for the management of inflammatory skin conditions. Approaches include:
- Probiotic supplementation: Select strains of probiotics have shown promise in improving symptoms of eczema and, to a lesser extent, psoriasis. However, results are inconsistent and strain-specific benefits require further research.
- Prebiotics: Non-digestible fibers that feed beneficial microbes may positively influence the microbiome and, by extension, the skin.
- Dietary interventions: Reducing processed foods, increasing fiber, and focusing on anti-inflammatory dietary patterns may support both gut and skin health.
- Antibiotic stewardship: Limiting unnecessary antibiotics preserves microbiome diversity, preventing dysbiosis that could worsen skin diseases.
Current Limitations and Future Directions
While mounting evidence advocates for gut-targeted therapies, most studies are still in early stages, and individual responses can vary widely. Personalized approaches and larger, high-quality clinical trials are needed to pinpoint the best strategies for skin disease management through the gut-skin axis .
Frequently Asked Questions (FAQs)
What is the gut-skin axis?
The gut-skin axis is the network of two-way communication connecting gut microbial health with skin health. Signals, metabolites, and immune mediators produced in the gut can affect skin inflammation and disease risk.
How does gut health influence eczema?
Poor gut microbial diversity, inflammatory metabolites, and a compromised gut barrier may all contribute to immune dysfunction that presents on the skin as eczema.
Can improving gut health help psoriasis?
Evidence suggests that restoring healthy gut microbial balance—through diet, probiotics, or other interventions—can reduce inflammation linked to psoriasis in some individuals.
Which foods are good for the gut-skin axis?
High-fiber vegetables, fruits, whole grains, and fermented foods support beneficial gut bacteria, while limiting processed sugary foods may help minimize inflammation.
Are probiotics effective for skin conditions?
Some probiotic strains may help alleviate symptoms of eczema and improve skin health, but the benefits depend on the specific strain and individual factors. More research is ongoing.
Conclusion
The evolving science of the gut-skin axis offers new hope in understanding and managing skin conditions like eczema and psoriasis. Maintaining gut microbiome balance through diet, lifestyle, and emerging gut-targeted therapies may unlock novel approaches to achieving healthier skin from the inside out.
References
- https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.01459/full
- https://www.gutmicrobiotaforhealth.com/the-gut-skin-axis-feel-it-in-your-gut-wear-it-on-your-skin/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9311318/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7916842/
- https://www.dermatologytimes.com/view/gut-health-and-its-impact-on-the-skin
- https://www.nature.com/articles/s41598-024-57649-z
Read full bio of medha deb












