Gut Health Restoration Protocols: Essential Steps After an Antibiotics Course
Replenish your gut’s beneficial bacteria and regain digestive vitality.
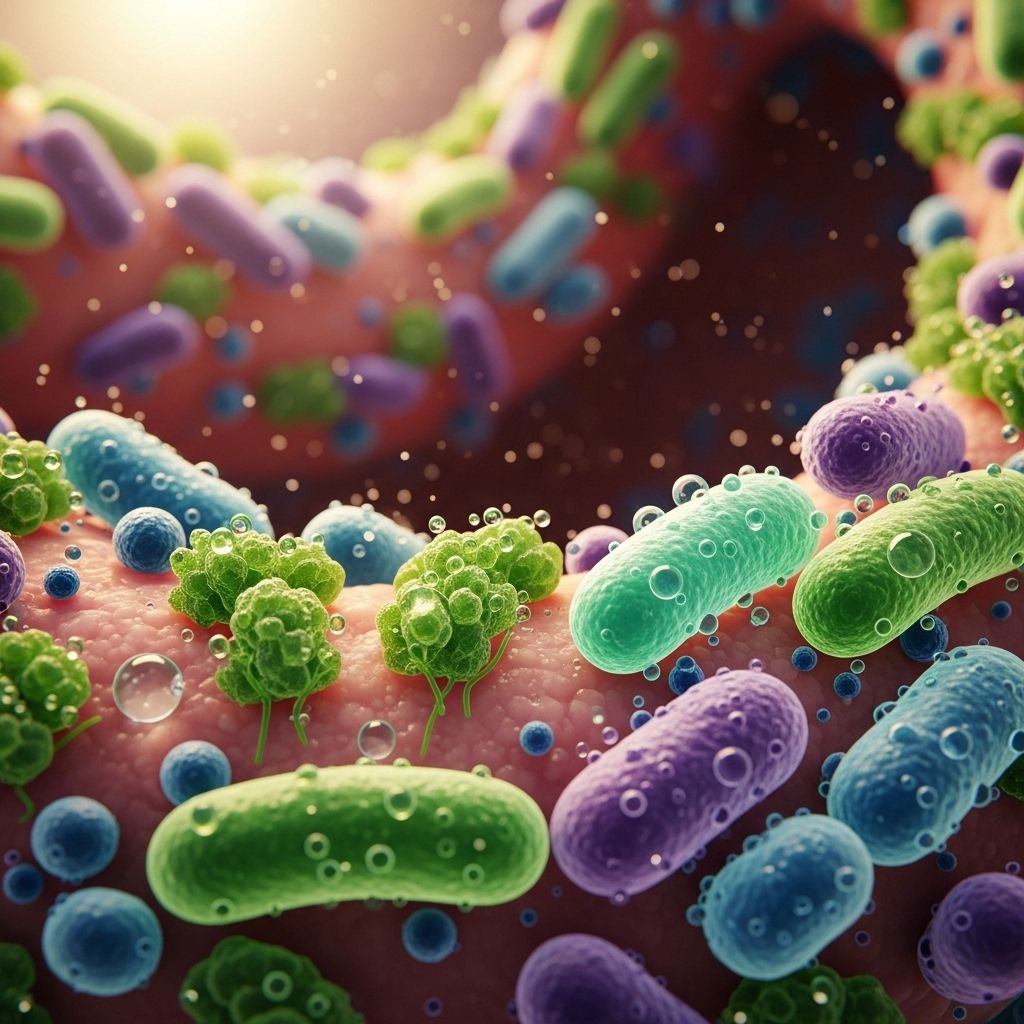
Table of Contents
- Introduction
- Impact of Antibiotics on Gut Health
- Common Gut Issues After Antibiotics
- Gut Restoration Protocols
- Probiotics: Types, Timing, and Efficacy
- Fermented Foods: Diversity and Benefits
- High-Fiber Diet and Prebiotics
- Other Dietary Recommendations
To further optimize your gut recovery, consider exploring our targeted probiotic strains specifically designed for post-antibiotic diarrhea. These scientifically-backed solutions can help you tackle gut imbalances efficiently and restore your digestive health. - Complementary Therapies and Lifestyle Factors
- Potential Complications and When to Seek Help
- Timetable for Recovery
- The Science Behind Gut Healing
- Individual Variability in Gut Recovery
- Frequently Asked Questions (FAQs)
Introduction
Antibiotics are essential for treating bacterial infections, but they can have a significant impact on the gut microbiome—the complex ecosystem of bacteria, fungi, and viruses that live in your digestive tract and play a crucial role in your overall health and immunity. Restoring gut health after a course of antibiotics requires a thoughtful, science-based approach. This article outlines practical protocols, dietary recommendations, and lifestyle strategies to help you rebuild a healthy gut microbiome and minimize adverse effects.
Impact of Antibiotics on Gut Health
Antibiotics are designed to kill harmful bacteria, but they do not discriminate between pathogens and beneficial gut bacteria. This collateral damage can disrupt the balance of your microbiome, sometimes leading to digestive symptoms such as diarrhea, bloating, cramping, and increased susceptibility to infections like Clostridium difficile. Long-term or repeated antibiotic use can also contribute to antibiotic-resistant bacteria and other complications.
Common Gut Issues After Antibiotics
- Antibiotic-associated diarrhea: One of the most frequent side effects, often due to the loss of beneficial bacteria.
- Bloating and cramping: Resulting from imbalances in gut bacteria and reduced digestive efficiency.
- Increased infection risk: Such as C. difficile colitis, which can be severe and difficult to treat.
- Yeast overgrowth: Including candida infections, due to disrupted microbial balance.
- Reduced nutrient absorption: As a result of impaired gut function.
Gut Restoration Protocols
Probiotics: Types, Timing, and Efficacy
Probiotics are live microorganisms that can help restore the balance of your gut microbiome after antibiotics. Research shows that specific strains—such as Lactobacillus, Bifidobacterium, and Saccharomyces boulardii—can reduce the risk of antibiotic-associated diarrhea and support gut recovery.
- When to take: Begin probiotics during your antibiotic course, spacing doses at least 2–4 hours apart from antibiotics to avoid interference. Continue for at least a few weeks after finishing antibiotics.
- Choosing a probiotic: Look for products with clinically studied strains and a high CFU (colony-forming unit) count. Strains like L. paracasei CNCM I-1518 and L. rhamnosus have shown benefits in accelerating microbiome recovery.
- Effectiveness: While the effect size may be modest, probiotics can help speed up the return of gut microbial diversity and function.
Fermented Foods: Diversity and Benefits
Fermented foods are natural sources of probiotics and other bioactive compounds that support gut health. Examples include yogurt, kefir, sauerkraut, kimchi, miso, kombucha, and cultured cheeses.
- Benefits: These foods introduce a variety of beneficial bacteria, supporting microbial diversity more effectively than supplements alone.
- Homemade vs. store-bought: Homemade fermented foods often contain higher and more diverse bacterial counts compared to commercial products.
- Dose and frequency: Aim to include at least one serving of fermented food daily during and after antibiotic therapy.
High-Fiber Diet and Prebiotics
Dietary fiber and prebiotics serve as fuel for beneficial gut bacteria, helping them thrive and repopulate your digestive tract.
- Fiber sources: Fruits, vegetables, whole grains, legumes, nuts, and seeds.
- Prebiotic foods: Garlic, onions, leeks, asparagus, bananas, and whole grains. These contain indigestible fibers that selectively nourish good bacteria.
- Timing: Increase fiber intake after completing your antibiotic course, as fiber can reduce antibiotic absorption if taken simultaneously.
- Special considerations: Soluble fiber, in particular, has been shown to reduce antibiotic resistance genes in the gut.
Other Dietary Recommendations
- Hydration: Drink plenty of water to support digestion and mucosal health.
- Polyphenol-rich foods: Foods like red wine (in moderation), cocoa, berries, and green tea contain polyphenols that act as prebiotics, supporting beneficial bacteria.
- Avoid irritants: Limit processed foods, added sugars, and alcohol, which can worsen gut inflammation and delay recovery.
Complementary Therapies and Lifestyle Factors
While diet is central, other factors also influence gut recovery:
- Stress management: Chronic stress can impair gut healing. Practices like meditation, yoga, and adequate sleep are beneficial.
- Physical activity: Regular moderate exercise supports overall gut motility and microbial diversity.
- Supplemental support: In some cases, additional nutrients like zinc, vitamin D, and glutamine may aid gut repair, though individual needs vary.
Potential Complications and When to Seek Help
Most people recover gut health within a few weeks, but complications can occur:
- Persistent diarrhea: Especially if accompanied by fever, blood in stool, or severe abdominal pain, may indicate C. difficile infection.
- Signs of malnutrition: Such as unexplained weight loss or nutrient deficiencies.
- Chronic symptoms: Bloating, constipation, or food intolerances lasting more than a month may require medical evaluation.
Timetable for Recovery
Gut microbiome recovery is highly individual, but a general timeline can be outlined:
| Timeframe | Focus | Actions |
|---|---|---|
| During antibiotic course | Minimize disruption | Take probiotics 2–4 hours apart from antibiotics; stay hydrated; avoid irritants |
| 0–2 weeks post-antibiotics | Rebuilding phase | Continue probiotics; introduce fermented foods; gradually increase fiber |
| 2–4 weeks post-antibiotics | Diversification | Emphasize diverse, fiber-rich, and prebiotic foods; monitor symptoms |
| Beyond 1 month | Maintenance | Sustain healthy dietary patterns; address persistent symptoms with healthcare provider |
The Science Behind Gut Healing
Advanced studies using metagenomics have shown that specific probiotic strains in fermented dairy products can accelerate microbiome recovery after antibiotics, as reflected by increased microbial diversity and the production of beneficial metabolites like short-chain fatty acids (e.g., butyrate, valerate). Strains such as S. thermophilus and L. paracasei contribute to amino acid synthesis and cross-feeding interactions that stimulate butyrate producers, which are essential for gut barrier function. Valerate, another fermentation product, has been linked to increased microbial richness and may inhibit pathogens like C. difficile.
While these effects are generally modest, they highlight the importance of microbial diversity and the potential for targeted interventions to support gut health after antibiotics. Future research may identify even more effective strains or synergistic combinations (synbiotics) to enhance recovery.
Individual Variability in Gut Recovery
Gut microbiome recovery is not one-size-fits-all. Factors influencing individual responses include:
- Initial microbiome composition: Baseline diversity affects resilience and recovery speed.
- Type and duration of antibiotics: Broad-spectrum and prolonged courses cause greater disruption.
- Diet and lifestyle: Consistent healthy habits support faster recovery.
- Age and health status: Children, elderly, and those with chronic conditions may recover more slowly.
Frequently Asked Questions (FAQs)
How long does it take to restore gut health after antibiotics?
Most people notice improvement within 2–4 weeks, but full recovery of microbiome diversity can take several months, depending on individual factors and adherence to recovery protocols.
Should I take probiotics during or after antibiotics?
Taking probiotics both during (spaced apart from antibiotics) and after an antibiotic course is recommended to support gut recovery and reduce side effects like diarrhea.
Are all probiotics equally effective?
No, effectiveness varies by strain and individual. Look for products containing clinically studied strains such as Lactobacillus, Bifidobacterium, and S. boulardii for best results.
Can I rely only on supplements, or should I also eat fermented foods?
Combining supplements with a variety of fermented foods provides greater microbial diversity and may lead to better outcomes.
Can high-fiber foods interfere with antibiotics?
Yes, consuming high-fiber foods during antibiotic treatment may reduce drug absorption. Focus on increasing fiber after finishing the course.
When should I seek medical help for post-antibiotic gut issues?
Seek medical attention if you experience persistent diarrhea, blood in stool, fever, severe abdominal pain, or symptoms lasting more than a few weeks.
How can I support my gut health long-term after antibiotics?
Maintain a diverse, fiber-rich diet, include fermented foods, manage stress, stay active, and consider periodic probiotic supplementation if needed.
Conclusion
Restoring gut health after antibiotics is a multifaceted process that involves probiotics, fermented foods, a fiber- and prebiotic-rich diet, and healthy lifestyle habits. While recovery varies by individual, following these science-backed protocols can help you rebuild a resilient microbiome, reduce side effects, and support long-term digestive and overall health. Always consult your healthcare provider for personalized advice, especially if symptoms persist or worsen.
References
- https://www.healthline.com/nutrition/what-to-eat-antibiotics
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9348039/
- https://tristategastro.net/how-to-heal-your-gut-after-antibiotics/
- https://windsordigestivehealth.com/restore-gut-health-after-antibiotics/
- https://www.gutmicrobiotaforhealth.com/what-you-need-to-know-about-the-effects-of-antibiotics-on-the-gut-microbiome-and-how-to-recover-after-taking-them/
- https://www.uclahealth.org/news/article/antibiotics-can-temporarily-wipe-out-gut-microbiome
- https://www.nature.com/articles/d41586-025-00477-6
- https://www.staceycollinsnutrition.com/blog/abx-and-supporting-yourself-getting-off
- https://www.youtube.com/watch?v=Q105opZ4XAU
Read full bio of Sneha Tete












