Gut Health & Preventing Recurrent Ear Infections: The Microbiome-Ear Connection Explained
Microbial balance reveals avenues for protecting children from persistent infections.
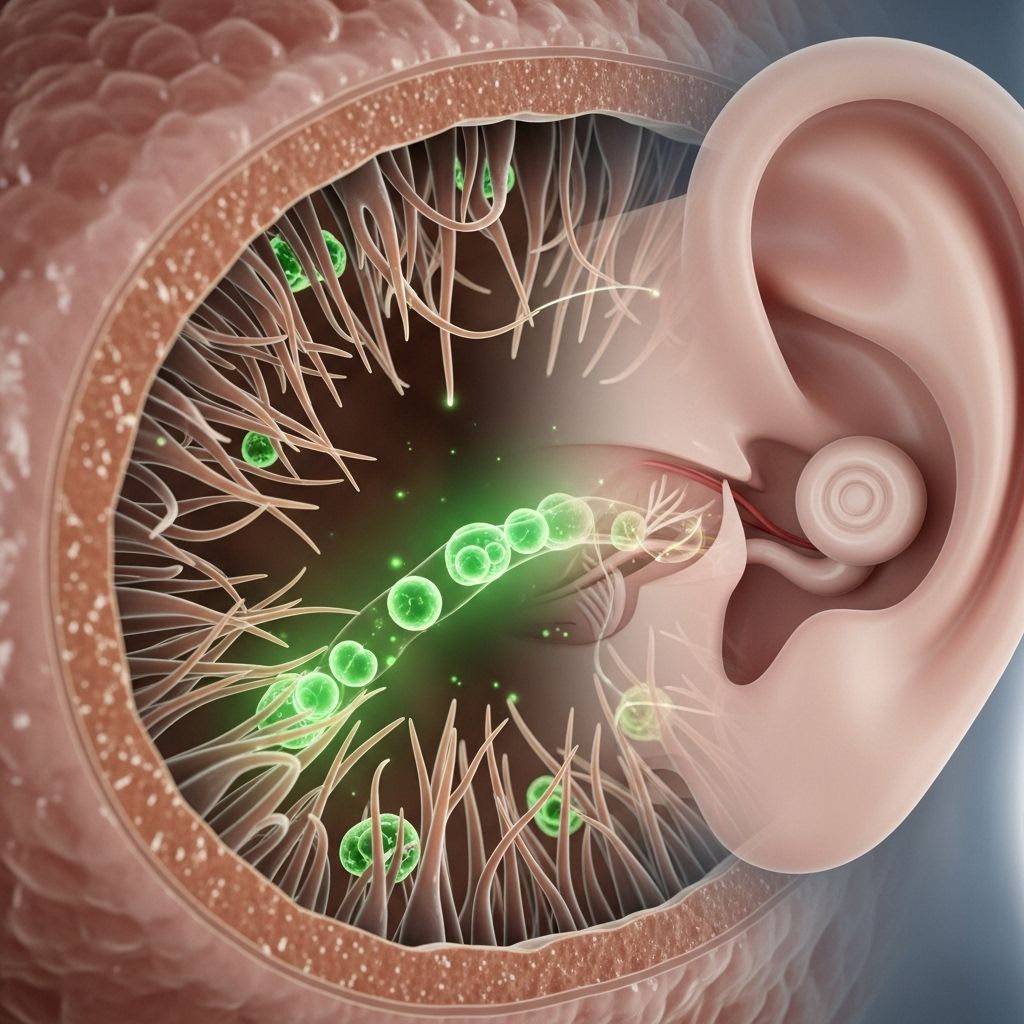
Why do some people, especially children, get repeated ear infections—and could the answer lie in the gut? Increasing medical evidence suggests that the gut microbiome may play a significant role in the development, prevention, and management of recurrent ear infections. This article explores the science behind the gut–ear axis, top strategies for optimizing gut health, and tips for long-term ear infection prevention.
Table of Contents
- Introduction to Ear Infections and Gut Health
- Understanding the Human Gut Microbiome
- Ear Infections: Causes and Risk Factors
- The Gut–Ear Axis: How Gut Health Impacts Ear Health
- Probiotics, Prebiotics, and the Prevention of Ear Infections
- Diet, Lifestyle, and Microbiome Optimization
- Antibiotics, Dysbiosis, and Combined Approaches
- Natural Health Products and Additional Prevention Strategies
- Frequently Asked Questions (FAQs)
- Conclusion and Future Directions
Introduction to Ear Infections and Gut Health
Ear infections, especially acute otitis media (AOM), remain one of the most common childhood infections and a leading reason for pediatric physician visits. While ear infections are often considered a localized problem, new research reveals that the roots of prevention may extend far beyond the ear itself—to the depths of the gastrointestinal tract. The emerging science of the gut–ear axis is opening new frontiers in both paediatric and adult preventive care.
Understanding the Human Gut Microbiome
The gut microbiome refers to the trillions of microbes—primarily bacteria—living within the human digestive tract. These organisms perform crucial roles in:
- Digestion and nutrient synthesis
- Regulation of the immune system
- Inflammation control
- Protection against pathogens
An individual’s microbial ecosystem develops from birth and is shaped by genetics, birth mode (vaginal vs. C-section), diet, antibiotic exposure, and environmental factors. Microbiome imbalances, known as dysbiosis, can predispose individuals to infection and immune dysfunction.
Ear Infections: Causes and Risk Factors
Pediatric and adult ear infections have several contributing factors:
- Upper respiratory tract infections
- Exposure to pathogens (bacteria, viruses)
- Allergies and inflammation
- Frequent antibiotic use
- Weakened or immature immune systems
- Environmental exposures (e.g. tobacco smoke, daycare attendance)
Recurrent ear infections, or repeated episodes over months or years, can lead to hearing loss and developmental complications in children. Traditionally, prevention focuses on vaccinations, improved hygiene, and antibiotic therapy—but as antibiotic resistance rises, alternative and adjunctive approaches are urgently needed.
The Gut–Ear Axis: How Gut Health Impacts Ear Health
Recent studies show a complex and bi-directional relationship between the gut microbiome and the auditory system:
- The gut microbiota influences systemic immunity, which can affect the ear’s ability to fend off infection and recover from inflammation.
- Dysbiosis may promote excessive immune responses, impair pathogen defense, and increase susceptibility to infections—including in the middle ear.
- Gut microbiome changes contribute to inflammation locally (gut and body) and systemically, which correlates with higher risk of otitis media and other auditory conditions.
- Certain gut-derived metabolites (like short-chain fatty acids) may directly support healthy blood flow to the ear and protect against inflammatory hearing loss.
One important finding: antibiotic treatment for ear infections can disrupt both nasopharyngeal (upper throat) and gut microbial populations, increasing the risk of resistant infections and persistent dysbiosis.
Scientific Evidence for the Gut–Ear Connection
- Probiotic administration has reduced the incidence of acute otitis media (AOM) in several studies, suggesting a preventive role for gut-focused strategies.
- Dietary patterns such as the Mediterranean diet, rich in omega-3 fats and polyphenols, modulate the microbiome and may lower inflammation related to ear disease.
- Combination probiotic-antibiotic regimens appear more effective than antibiotics alone, reducing recurrence and adverse effects.
Probiotics, Prebiotics, and the Prevention of Ear Infections
Probiotics are live microorganisms (most commonly Lactobacillus and Bifidobacterium) which confer health benefits by restoring or maintaining a healthy gut flora. Prebiotics are fibers and compounds that nourish beneficial bacteria already present. Their benefits for ear infection prevention may include:
- Strengthening immune responses: Probiotics can help train the immune system for balanced, targeted responses, reducing harmful inflammation while enhancing defense against pathogens.
- Restoring balance after antibiotics: Antibiotics may wipe out beneficial bacteria, but probiotics and prebiotics help re-establish a protective microbial community.
- Competition with pathogens: Beneficial bacteria may out-compete, inhibit, or directly neutralize disease-causing organisms in both the gut and respiratory tract.
- Production of anti-inflammatory metabolites: These include short-chain fatty acids and neurotransmitters (like GABA), which can modulate inflammation systemically—including in the ears.
Key Probiotic Strains Involved:
- Lactobacillus species: Widely studied for supporting immune and mucosal health.
- Bifidobacterium: Linked to gastrointestinal and immune benefits, as well as neurotransmitter modulation.
- Streptococcus salivarius: Shows promise as an upper respiratory tract probiotic, targeting pathogens relevant to otitis media.
Prebiotics and Synbiotics
Prebiotics—such as inulin, fructo-oligosaccharides, and other dietary fibers—promote the growth of beneficial bacteria. Synbiotics refer to combinations of probiotics and prebiotics for a synergistic effect.
Diet, Lifestyle, and Microbiome Optimization
Diet and lifestyle choices have a profound impact on the diversity and stability of the gut microbiome, and by extension, overall immune health and infectious risk. The following practices support optimal gut (and ear) health:
- Follow a Mediterranean-style diet: High in vegetables, fruits, legumes, whole grains, nuts, extra virgin olive oil, and fish (omega-3 sources). This diet increases microbiome diversity and reduces inflammation.
- Limit processed foods, added sugars, and refined grains: These can disrupt gut microbial equilibrium and promote inflammation.
- Include regular sources of dietary prebiotics: Examples are onions, garlic, leeks, asparagus, bananas, and artichokes.
- Fermented foods can enhance probiotic intake: Consider yogurt with live cultures, kefir, sauerkraut, kimchi, tempeh, or miso.
- Hydration matters: Keep your gut lining healthy and support microbial metabolism by drinking enough water.
- Physical activity supports a healthy microbiome: Regular moderate exercise has been shown to increase beneficial gut bacteria.
- Avoid unnecessary antibiotics and reduce exposure to environmental toxins/smoke, both of which alter microbiome composition.
Antibiotics, Dysbiosis, and Combined Approaches
While sometimes essential, antibiotics can lead to collateral damage by eradicating both harmful and helpful bacteria, contributing to:
- Dysbiosis: Imbalance in microbial communities, impairing protective functions and immune modulation.
- Antibiotic resistance: Recurrent or broad-spectrum antibiotic use selects for resistant pathogens, increasing health risks.
Research suggests that combining a reduced dose of antibiotics with probiotic administration may yield better outcomes in children with recurrent ear infections, lowering relapse rates, and minimizing adverse effects.
Comparison Table: Standard vs. Combined Probiotic-Antibiotic Therapy
| Aspect | Standard Antibiotic Therapy | Combined Probiotic & Reduced Antibiotic |
|---|---|---|
| Effectiveness | Controls infection | Reduces infection, maintains gut balance |
| Side Effects | Digestive upset, yeast overgrowth, dysbiosis | Fewer adverse effects |
| Antibiotic Resistance | May increase with repeated use | Reduced risk due to lower exposure |
| Immune Modulation | Minimal | Enhanced; supports healthy immune responses |
Natural Health Products and Additional Prevention Strategies
- Echinacea, Propolis, and Vitamin C: Common herbal and natural products shown in some studies to reduce the risk of otitis media.
- Xylitol: A natural sugar alcohol found in some chewing gums and lozenges; may reduce pathogenic bacteria in the mouth and upper airway and lower the risk of ear infections.
- Micronutrients: Zinc, vitamin D, and other micronutrients may support mucosal immunity and reinforce the gut–ear preventative connection.
- Hygiene and Environmental Measures: Avoiding secondhand smoke, promoting breast feeding in infants, and minimizing unnecessary exposures may also help prevent recurrence by maintaining immune homeostasis.
Frequently Asked Questions (FAQs)
What is the most important step for reducing recurrent ear infections through gut health?
Focus on building and maintaining a diverse gut microbiome through diet (Mediterranean style), probiotics, and minimizing unnecessary antibiotic use. These all support stronger systemic immunity, which is vital for preventing infections in the ears and elsewhere.
Are probiotics safe for children?
Most probiotics are safe for healthy children when used as directed, but it’s always advisable to consult with a pediatrician before starting any supplement, especially in infants or children with immune compromise.
How long does it take for gut health interventions to impact ear infection risk?
Changes in the microbiome can occur within days to weeks of dietary or probiotic changes; however, lasting protection often requires sustained lifestyle and dietary changes.
Can diet alone be enough, or are supplements needed?
A nutrient-rich, whole foods diet can go a long way toward promoting optimal gut health. Probiotic supplementation may provide additional help, particularly after antibiotics or during periods of recurrent infections.
Do these approaches protect against all forms of ear infection?
No prevention strategy is 100% effective for all people or types of ear infections, but optimizing gut health lowers risk and improves recovery in many cases. Chronic, severe, or complicated infections may require specialized medical care.
Conclusion and Future Directions
Modern research continues to underscore the vast—and often surprising—relationships between gut health and ear disease. As science unravels the details of the gut–ear axis, practical interventions such as diet, probiotics, prebiotics, natural products, and judicious use of antibiotics are emerging as valuable tools in preventing recurrent ear infections.
Personalized, microbiome-centered care represents a promising frontier for families seeking additional support beyond standard medical and surgical approaches. As research advances, new probiotic strains, synbiotic formulas, and precision nutrition therapies are likely to become standard components of infection prevention and ear health programs.
Consult with your healthcare provider for guidance tailored to your family and individual needs, especially before making major changes or starting supplements in children.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10603848/
- https://hearinghealthfoundation.org/blogs/recent-research-from-erg-alumni
- https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1661871/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5819196/
- https://greaterknoxent.com/the-link-between-gut-health-and-ent-health/
- https://www.cochrane.org/evidence/CD012941_probiotics-healthy-bacteria-preventing-acute-middle-ear-infection-children
Read full bio of medha deb












